Radiation therapy for cervical cancer can be used as primary and adjuvant treatment. As a result of a course of procedures, it is possible to cure cancer, since the process of tumor spread at the cellular level is stopped. The radiation dose and number of sessions are determined by the attending physician based on the results of a comprehensive examination of the patient.
Modern medicine has the ability to carry out both external and internal irradiation of the focus of the pathological formation. In most cases, these methods are combined to obtain maximum results. Despite a number of side effects, this method of therapy can be recommended, since with its help it is possible to fight the oncological process at different stages and save the lives of patients.
The essence of the method
Radiological irradiation as an independent method is effective at the second and first stages of the oncological process. At the third stage, especially in the presence of metastases, this treatment is combined with chemotherapy.
The method is based on the interaction of radio rays with cancer cells. Radioactive radiation stops the proliferation of the tumor, since the processes of division of pathological cells stop, while healthy tissues retain this ability.
The mechanism of action of ionizing radiation is as follows:
- Water molecules are converted into peroxide radicals, which damage the cell.
- Active cells are damaged most severely (cancer cells are characterized by maximum activity). Radiation has a negative effect on DNA.
- The tumor loses its ability to grow as division processes stop. Healthy tissues retain their regenerative properties and therefore can fully restore their functionality.
- In addition to stopping the division processes, many mutations occur in a malignant neoplasm, which causes the death of pathological cells.
Treatment of cervical cancer (cervical cancer) with radiation therapy is possible for large tumor sizes and in case of spread of the oncological process. This method is also used after surgery, especially with a high risk of disease relapse, and is combined with chemotherapy. Irradiation sessions are carried out for 5-8 weeks with breaks.
How long can you live with stages 1, 2, 3, 4 of cervical cancer?
Cervical cancer is one of the intractable diseases that is often diagnosed in patients of all ages.
The development of such a pathology leads to various unpleasant consequences and may result in the death of the patient. Many women ask their doctors how long they can live with cervical cancer and whether it is possible to get rid of this disease forever.
Experts distinguish several stages of the disease, and each of them has different prognosis for recovery.
Characteristics of the disease
Cervical cancer begins its progression from the moment healthy cells undergo mutation at the genetic level. The consequence of this pathological process is the transformation of healthy cells of the body into atypical ones.
In the female body, healthy cells grow and multiply quickly, but over time they die completely. A feature of pathological cells is the fact that they also rapidly divide, but do not die.
When a large number of cancer cells accumulate in a woman’s body, malignant tumors form. Further progression of the pathology leads to the fact that such neoplasms begin to spread to nearby organs, and metastases form. Experts still do not have data on what triggers the development of cervical cancer.
There are some factors whose impact on the body can provoke the development of cancer:
- extra pounds on the body or obesity;
- disruption of the body's immune system;
- living in unfavorable conditions;
- the presence of infections, predominantly sexually transmitted.
This type of cancer can be detected both in young girls and in old age. Medical practice shows that most often cancer of the reproductive organ is diagnosed in patients after 35 years of age.
The appearance of certain symptoms is determined by the stage of the pathology and at the very beginning of its development the woman does not complain about anything.
The first sign of cancer is usually bloody discharge from the uterus, and it has nothing to do with menstruation.
Doctors believe that women must pay attention to such a symptom. Bleeding often appears after heavy physical exertion, gynecological examination and sexual intercourse.
The most common signs of cervical cancer in women are:
- severe pain localized in the lower abdomen;
- swelling of the lower extremities;
- increased fatigue;
- rise in body temperature;
- loss of appetite or its complete absence;
- discomfort when urinating;
- renal colic.
In addition, there is general intoxication of the body and the woman constantly vomits. The appearance of such symptoms in a woman may indicate the presence of a tumor, so if they appear, you should definitely consult a specialist. Cervical cancer can spread quite quickly and affect other organs located in the pelvic area, so do not delay visiting a doctor.
Stages of the disease
In its development, cancer can go through several stages and each of them is accompanied by the appearance of certain symptoms.
Zero stage
Carcinoma is a pathological condition of the body, which is accompanied by the appearance of a small number of cancer cells. At this stage, there is no serious damage to the organ, so it is not entirely correct to call this condition oncology.
Doctors call this disease stage zero, and by removing such atypical cells, it is possible to prevent the development of cancer of the uterine pharynx. In the absence of modern and effective therapy, stage zero can transform into a dangerous malignant tumor, which seriously aggravates the patient’s condition.
First stage
The first degree of cervical cancer in women is a small tumor that cannot be detected without special examination. The fact is that during a gynecological examination it is quite problematic to see accumulations of atypical cells, since they are still invisible.
At the first stage of cancer, the malignant neoplasm is located within the organ and does not affect nearby tissues. The disease can mainly be diagnosed during colposcopy or examination of the genital organ through a microscope. The prognosis for survival with early stage cancer depends on the timeliness of the therapy started and compliance with all doctor’s recommendations.
Cervical cancer stage 1 (a and b) - treatment and prognosis
Second stage
A woman may notice the appearance of bloody fluid or copious discharge on her underwear, which gives off an unpleasant odor.
They may contain pieces of tissue, which indicates that the decomposition process has begun. Survival at 5 years is observed in half of the recorded cases of this type of cancer.
After surgery, the prognosis is favorable only if the tumor has not metastasized.
Third stage
The tumor at this stage grows into the cervix of the reproductive organ and affects the tissues of the pelvis and lower vaginal area. The pathology progresses rapidly and can lead to problems with the patency of the ureters, and the consequence of this pathological process is a violation of the outflow of urine.
It is quite problematic to answer the question of how long patients with this stage of the disease live, since much is determined by the individual characteristics of the body and the effectiveness of the selected therapy.
Prompt initiation of treatment after diagnosis greatly increases the chances of survival.
In fact, it is quite difficult to cure such a disease in young and elderly people and treatment methods are aimed only at slowing down the progression of the tumor.
Source: //sheika-matka.ru/zabolevaniya/rak/vyzhivaemost-pri-rake-shejki-matki-na-razlichnyx-stadiyax/
Types of exposure
It is possible to use various types of radiation for therapeutic purposes. The equipment models used affect the tumor using neutrons, electrons, photons and protons. The proton method is recognized as the most gentle, but also less accessible due to its high cost.
Not so long ago, the latest equipment called the “Neutron Knife” began to be used in medical practice. The particular value of this installation lies in the possibility of treating cancer in the final stages with minimal side effects. This treatment is applicable for weakened patients for whom intracavitary surgery is too dangerous and ineffective.
There are the following methods of influencing a tumor using radiotherapy:
- External exposure. A special installation is used to remotely influence the focus of the oncological process.
- Internal exposure. A special capsule containing a radioactive substance is inserted into the uterine cavity. A targeted effect on pathological cells is achieved, which promotes rapid recovery after treatment.
In most cases, doctors use both of these methods in combination to achieve maximum results. In addition, radioactive radiation can be used for preparatory purposes before surgery to reduce the size of the tumor. After surgery, radiotherapy is used to permanently eliminate cancer cells to prevent relapses.
External beam radiation therapy does not require hospitalization and is performed on an outpatient basis. The course consists of short procedures, during which the area with the tumor is targetedly irradiated using a linear catalyst. Previously, the patient undergoes a computed tomography scan, which allows obtaining a three-dimensional image of the tumor. Then special markers are applied to the skin to limit the area of treatment. The session lasts several minutes, and the procedure itself does not cause discomfort.
Internal radiation therapy is performed more often after external radiation therapy. The course of treatment is carried out in a hospital setting, since the radiation source is placed in applicators (tubes) that are located in close proximity to the tumor. If the patient has not had her uterus removed, then the applicators are placed in her cavity and vagina.
The applicators are installed surgically under general anesthesia.
To prevent displacement of radiation sources, a gauze or cotton swab is installed in the genital canal. To reduce pain, the patient is prescribed painkillers. If the patient's uterus has been removed, then only one large applicator is installed. In this case, there is no need for pain relief.
Using computed tomography or x-rays, the placement of applicators is monitored. According to the degree of impact on the tumor during internal radiation therapy, they are distinguished:
- High-dose treatment - during sessions the patient receives a large dose of radiation over a quarter of an hour. This method is used most often.
- Low-dose treatment is a short-term course of therapy and can take from 12 hours (one session) to several days. The patient is kept in bed, a catheter is installed in her bladder and strong anesthetics are prescribed to reduce pain.
- Pulse therapy differs from low-dose radiation in that it periodically affects the tumor. During the entire treatment, the applicators remain inside the patient’s body.
How is it carried out?
Internal irradiation is carried out after remote irradiation no earlier than 2 weeks. The applicator is inserted under general or spinal anesthesia. Before administration, an examination is carried out to clarify the effect of remote irradiation. A radiopaque mark is applied to the neck. The uterine cavity is measured with a uterine probe. The cervical canal is expanded and an applicator is inserted. The vagina is tamponed.
Later, a 131Cs source is inserted into the applicator. The bladder is catheterized and 7 ml of radiopaque contrast agent is injected into it. Marks are applied to the anus. If possible, a dosimeter is inserted into the anus.
Photographs of the pelvis are taken in direct and lateral projections. Calculate the dose for points A and B, bladder, rectum. According to indications, antibiotics, anticoagulants, and corticosteroids are prescribed.
When deciding whether a cancerous lesion has been identified and needs to be treated, the specialist focuses on the structure of the tumor, whether it is malignant, its size, and the age category of the patient.
The fact that radioactive rays pose a direct threat to tissues not affected by atypia is also taken into account. Such therapy is necessarily carried out in several stages - with breaks of several weeks between procedures. If necessary, separate procedures are applied to target specific areas.
Preliminary setup of equipment is a mandatory step. A careful selection of the correct direction of the rays is carried out to accurately hit the tumor site. After taking a series of images, the information is displayed on the screen, and the specialist identifies the location of the carcinoma, its boundaries, and calculates the radiation therapy load.
Then the device system itself will manage the process of placing and subsequent rotation of the patient, the emitter itself, and also adjusts the position of the protective devices. If the contours of the tumor were clearly marked on the pictures, then the laser beam will highlight the point of direct impact on the body of the irradiated person.
It is somewhat more difficult if the malignant lesion has moved to neighboring tissues and organs. However, modern equipment makes the task easier for specialists - tomographs make it possible to obtain a three-dimensional image of the tumor, followed by a radiation treatment program.
Indications for use
Radiation therapy is used as the main treatment for stage 1 cervical cancer. In the second degree of the disease, this method can be considered as an auxiliary method, and the main one is surgical intervention. Indications for treatment with radioactive irradiation are:
- tumor metastasis to nearby organs;
- high risk during surgery due to various diseases;
- carcinoma or other poorly differentiated tumor that metastasizes at different stages;
- the last stage of the cancer process, when surgical treatment is dangerous and impractical.
Radiotherapy is part of treatment for all stages of cervical cancer. At the first stage of the oncological process, this may be the only method of therapy, and at the second and third stages it can be used as part of a combination treatment. In most cases, cervical cancer is diagnosed at stages 2 and 3, when the patient begins to experience discomfort.
Due to the fact that radiological treatment negatively affects reproductive function and often causes infertility, they try not to prescribe this type of therapy to young patients who are capable of childbearing.
The use of radiation in such a case may be justified in critical cases with great caution. Women may be asked to move their ovaries higher to remove them from the radiation exposure area or reduce its negative effects. The displacement is performed surgically.
Description of the technique
A malignant focus in the cervix is one of the most frequently detected cancers in the female half of the population. Up to half of all identified cases are in advanced forms, so treatment tactics include not only chemotherapy, but also radiation exposure.
A similar technique can be the main way to get rid of a malignant lesion if it was detected at stages 1-2. To describe the process briefly, the essence is that beams of directed radiation, having encountered an atypical cell, contribute to the destruction of its very basis. As a result, it is unable to fulfill its functional purpose.
Preparation for the procedure
Before conducting a course of radiological treatment, the oncologist performs the following actions:
- calculates the radiation dose in accordance with the individual characteristics of the patient;
- determines the size of the tumor and its exact location;
- Applies markers to the patient’s skin according to the projection of the contours of the tumor.
Preparation for radiation exposure is carried out a week before the start of therapy and consists of the following:
- You must drink at least 2 liters of water per day;
- to eat well;
- give up bad habits, including smoking.
After starting the procedures, you must follow these recommendations:
- do not wear woolen or synthetic clothing;
- It is unacceptable to thermally influence the irradiation area (cool, warm);
- The irradiated area must not be rubbed, or cosmetics, deodorants or soap solutions applied to it.
It is recommended to eat high-calorie foods after the session. Sweet dishes are good for this.
Side effects
As a result of radiotherapy, the patient's general condition may worsen. The following post-radiation complications are observed:
- nausea;
- decreased appetite;
- diarrhea;
- itching;
- frequent urination;
- prostration;
- weight loss;
- weakening of the body's resistance;
- swelling of the legs, genitals and pelvic area due to lymphostasis (if radiation has affected adjacent lymph nodes);
- blood in urine and feces due to fragility of blood vessels due to radiation exposure;
- intestinal obstruction or narrowing of the intestines, which manifests itself as abdominal pain, vomiting and constipation;
- vaginal dryness and bleeding from it.
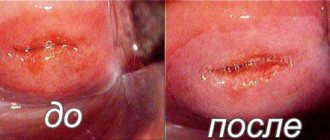
For severe digestive disorders, high-calorie drinks are prescribed instead of food. The only thing that helps with general weakness is long rest and the absence of stressful situations. During treatment, tissue changes occur, which causes shortening and dryness of the genital canal; scar tissue forms in certain areas, which makes examination difficult and negatively affects the patient’s intimate life.
Rehabilitation period
After radiation exposure for cervical cancer, recovery lasts a long time. In order not to aggravate side effects and minimize their manifestation, it is recommended to adhere to the following rules:
- provide moderate physical activity;
- reduce the consumption of coffee and tea if it is impossible to completely stop drinking these drinks;
- take regular walks in the fresh air;
- provide nutritious, healthy nutrition;
- give up bad habits (they enhance the negative effects of radiation).
The diet during and after radiation therapy includes the inclusion of a large amount of vegetables and fruits, as well as fermented milk products. The proportion of meat in the diet should be reduced and consumed boiled or stewed. It is necessary to exclude flour, fatty, sweet and smoked dishes from the daily menu.
Recovery after radiotherapy
Radiation therapy is usually well tolerated by patients, and recovery is uneventful. However, side effects may occur during the recovery period. In such cases, you should consult a doctor.
Side effects
One of the most common consequences during the recovery period is the occurrence of bleeding.
Side effects during recovery from radiation therapy include the following:
- Stool disorders. This is a fairly common consequence that occurs during recovery from radiation therapy treatment. During the recovery process, doctors recommend consuming at least two liters of water to prevent dehydration.
- Nausea. Usually this manifestation is accompanied by vomiting and loss of appetite. In such cases, the woman is recommended to drink high-calorie drinks.
- Weakness. Fatigue often occurs during radiation therapy. In order to reduce unpleasant consequences, it is advisable for the patient to pay special attention to rest.
- Narrowing of the vagina. This condition may make it difficult to perform a gynecological examination and insert special applicators. To maintain the required vaginal diameter, gynecologists recommend inserting tubes. Moreover, the risk of injury with proper treatment is minimal.
Sometimes, minor side effects lead to serious consequences, such as premature menopause. With the combined use of radiotherapy and surgery, lymphedema may appear during the recovery period. With this consequence, swelling of the lower extremities is observed.
Often side effects and complications cannot be treated. That is why a woman should be attentive to her well-being during the recovery period.
The method of radiation therapy is constantly being optimized, which reduces the risk of consequences during the recovery period and increases the effectiveness of treatment.
Consequences
One of the most unpleasant and dangerous complications of radiological treatment is bleeding, which may be accompanied by pain. In this case, you should immediately contact your doctor for further treatment and to prevent the condition from worsening.
One of the consequences of a radiation burn is the formation of adhesions in the vagina, which makes intimate life impossible and requires surgical treatment. Narrowing or shortening of the genital canal also interferes with sexual intercourse and negatively affects the sensations of partners. To correct the situation, the doctor may prescribe topical application of hormonal creams and the installation of a dilator (a plastic dilator in the form of a tube) in the vagina.
Infertility as a consequence of exposure to radioactive rays on a woman’s ovaries is a common and in most cases irreparable consequence of such treatment. Radiation therapy at the first and second stages of cancer allows achieving high survival rates for patients (97% and 75%, respectively). At the third stage, this figure drops to 60%, and at the fourth - to 10%. To prevent relapse of the disease, it is recommended to be examined by your doctor every 3 months.
Life expectancy for cervical cancer – Gynecology
Stage 3 cervical cancer is a serious oncological disease, reflecting a disappointing prognosis for the recovery of patients. The pathology is characterized by the most advanced form of cancer at the third stage. Treatment of stage 3 uterine tumors involves the use of a variety of techniques.
Cervical cancer of the uterus is the formation and development of a malignant neoplasm arising from squamous epithelium and glandular material. The disease is considered widely known and widespread.
The disease occurs very often, leaving breast tumors behind in the number of diagnosed pathologies.
Causes of cervical cancer
Oncological formation in the uterine cervix of the third stage is the result of serious dysplastic changes that have developed over many years. A healthy cell is destroyed under the destructive effects of negative factors. Subsequently, the cell structure loses its standard shape, the number of nuclei increases, and separation into layers stops.
The causes of cervical cancer are:
- An infectious process introduced through the genital tract - herpes or HPV.
- Long-term foci of inflammation.
- Regular injury to the cervical epithelium.
- Carcinogenic effect of male smegma.
- Use of tobacco products.
- Genetic predisposition, poor heredity.
- Exposure to harmful environmental conditions.
- Long lasting stress.
- Disorders of the immune system, hormonal levels and metabolic functioning.
- Early onset of sexual activity.
- Promiscuous relationships, having more than one sexual partner.
- Neglect of protective equipment.
- Development of precancerous conditions of the cervix.
The background picture is pseudoerosion and leukoplakia. Ambiguous pathologies can cause a malignant oncological process in the organ. Therefore, if a benign neoplasm is detected, it is recommended to immediately begin treatment.
Symptoms of stage 3 cervical cancer
A pronounced sign of cancer in most cases appears by the third stage. The initial stage of the disease occurs without specific symptoms. As a result, a dangerous growth is diagnosed and treated belatedly. Symptoms indicating the presence of pathogenic foci in the cervix:
- release of a watery structure;
- bloody or cloudy fluid, in rare cases accompanied by a foul odor;
- spotting blood clots are released in the period between menstruation;
- postmenopausal bloody fluids;
- bleeding from the uterine cavity other than menstruation, also in postmenopause;
- painful sensations during sexual intercourse, spotting after sexual intercourse;
- painful manifestations during a gynecological examination, blood is released after the procedure.
General symptoms of atypical and chronic intoxication and the presence of an inflammatory focus:
- poor health, malaise, decreased performance;
- weakness in the body, decreased or lack of appetite;
- pain in the pelvis;
- headache, migraine;
- persistent low-grade fever.
Together with atypical fluid secretion and factors of the intoxication process in stage 3b cancer, signs of hydronephrosis are observed:
- pain in the abdomen and lumbar region;
- re-developed pyelonephritis;
- colic in the kidneys;
- when you press on the abdomen, you feel an increase in the size of the affected kidney and the presence of a tumor in the area of the affected organ;
- nausea, indigestion;
- symptoms of a urinary tract infection, fever, fever, pain or discomfort during urination;
- disordered urination;
- presence of blood clots in urea;
- high blood pressure;
- swelling of the lower extremities;
- constipation.
With type 3b cervical cancer, pain manifests itself in different ways:
- dull;
- pulling;
- tolerant;
- in the form of contractions;
- constantly present, systematic, sudden;
- during sexual intercourse;
- while going to the toilet;
- during defecation.
Diagnostics
Often, symptoms at the initial stage of cancer can be confused with signs of organ pathology. To check and confirm the diagnosis, the doctor prescribes a list of special research techniques:
- Blood biochemistry - the analysis is designed to detect atypicalities in the structure of the blood. Cancer is primarily reflected by decreased iron levels.
- A gynecological examination is a standardized examination method performed at every visit to a gynecologist. The doctor examines the cervix using a special examination mirror. If suspicious abnormalities are detected in the results of the study - elevation, compaction or ulcerative lesions - this acts as a prescription for a more thorough analysis.
- Colposcopy is prescribed for bimanual analysis and similar techniques that are accompanied by a risk of bleeding. The research method is carried out within the boundaries of the simplest and extended examination. Simple diagnosis involves studying the mucous tissue of the uterine cervix through a colposcope microscope. This device contains a magnifying and lighting function that helps to reflect the smallest atypical changes. If during a simple colposcopy the doctor detects atypia, an expanded algorithm of actions is carried out. The doctor applies acetic acid to the uterine cervix. If you have HPV, white patches appear. The affected area does not turn into the typical brownish tint after using Lugol's.
- Diagnostic test - designed to determine the quality of the tissue covered and the intensity of the spread of tumor cells.
- Smear for oncocytology - diagnostic screening is a cytological analysis. The doctor takes biomaterial from various places on the mucous membrane of the cervix and transfers it to a special glass. A sample of the material is stained in the laboratory and subsequently analyzed through a microscope. A smear allows you to identify cellular atypicality and an inflammatory process.
- Bimanual examination of the vagina - the procedure helps to evaluate tightness that is not visible to the human eye.
- Biopsy is prescribed to detect the type of pathogenic cell, on the basis of which suitable and effective treatment will be prescribed.
- Rectal-vaginal examination - the form of cancer is reflected, and the intensity of organ mobility is examined.
- Rectal-abdominal-wall examination - performed to indicate the position of the sacral ligaments in the uterus, an infiltrating wall is detected.
- Ultrasound of the pelvic organs, peritoneum, retroperitoneal cavity.
- Ultrasound of lymph nodes in the supraclavicular and inguinal region.
- MRI or SCT of the pelvis, peritoneum with the introduction of a contrast agent intravenously.
- PET-CT.
- Intravenous urography.
- Cystoscopy.
- X-ray of the chest area.
- X-rays of the bone structure of the skeleton.
- Renal scintigraphy.
- Residual laboratory tests.
Treatment options for cervical cancer
Treatment at stage 3 of organ pathology depends on the degree of damage to nearby materials and contact with the organ. In most cases, removal of the uterus and lymph nodes is performed in the early stages of disease progression.
Therapy in the later stages of a malignant cancer of an organ is intended to block the subsequent development and spread of oncology. The result is achieved after chemotherapy and radiation therapy.
Regional production of metastases contributes to the use of treatment for third-stage cancer as a complex effect on the female body.
Elimination of a pathological disease in the later stages can be achieved using the following methods:
- Radiation therapy - the procedure is highly effective and gives a positive result in combination with chemotherapy. The method is considered central, since at stage 3 of cancer, surgery is not performed.
- Chemotherapy is a method often prescribed in conjunction with the use of cytostatic drugs in a complex group with radiation treatment. According to doctors, such a combined effect of the drug on the body leads to many unpleasant consequences and side effects. However, after combined therapy, survival is higher.
- Immunotherapy is a method designed to enhance the protective properties of the body’s immune system using anticancer drugs.
When diagnosing stage 3 tumor of the uterine cervix, difficulties arise in performing treatment, which are excluded after surgery due to limitations. The prognosis for cure and survival as a result is disappointing.
However, one cannot relax, as women live quietly in parallel with the developing disease. It is difficult for doctors to say exactly how long it will be possible to live with stage 3 malignant cervical cancer after completing the prescribed therapy.
A woman largely independently determines her future; the result depends on personal characteristics and body traits.
Radiation therapy
Oncological pathology is treated using combination radiation therapy. Radiation therapy consists of external beam and intracavitary radiation. The remote method is carried out in 2 approaches. At the first stage, the entire pelvis is irradiated towards the abdominal aorta. At the next stage, an irradiation procedure is performed on a regional group of lymph nodes.
In most cases, double radiation of the nodules is prescribed with a dosage of up to 48 GH. Therapy is performed 5 times a week. Then there is a break. After a pause, the patient is sent for intracavitary treatment. Intracavitary irradiation refers to the targeted effect of gamma rays on the cervix. For the procedure, a special tube is inserted into the vagina, through which X-rays are released.
The method is performed no more than 3 times every 7 days. The procedure consists of repeated courses of radiation therapy. In the modern world, the treatment method is most effective for cancer that forms on the uterine cervix. High-dose radiation guarantees a favorable outcome in 55-60% of cases.
Chemotherapy
Chemotherapy is prescribed in cases where the cancer is highly differentiated. In another situation, the use of chemicals gives only a slight favorable result. The problem lies in the peculiarities of blood movement through the blood vessels to the pelvic organs.
When tissue structures are injured, blood has difficulty penetrating the uterus together with medications in a small volume. As a result of deficiency, the therapeutic effect is reduced to 0%. In frequent situations, the chemotherapy procedure becomes an auxiliary, complementary technique in treatment.
It requires the use of the following medications:
- Paclitaxel is used intravenously once a day.
- Cisplatin is administered intravenously twice a day.
Chemicals are administered over 3-5 days. The duration depends on the intensity of the affected area. The course of therapy consists of several procedures carried out with a time interval of 21 days.
For cancer at the last stage, medications are prescribed a month before the date of expected radiation therapy, using once every 7 days.
According to statistics, the number of surviving patients who underwent a complex of radiation and chemotherapy procedures reaches 60%.
Immunotherapy
Immunotherapy is prescribed only in the form of an auxiliary and supportive treatment method.
The therapy involves the use of high-dose interferon, which enhances the protective properties of the human immune system and promotes increased performance of the body.
As a result, the body's overall resistance to pathological diseases increases. The dosage in each individual situation is calculated on an individual basis, based on the general well-being of the patient and the condition of the organs.
Immune therapy is carried out after the combined effects of chemotherapy and radiation therapy. The procedure is carried out in a one-time course without adding interval time. The purpose of the procedure does not affect the subsequent prognosis after treatment. However, strengthening the immune system reduces the likelihood of a primary relapse by 30%.
Recovery prognosis
The third stage of cancer is characterized by a decrease in the effectiveness of the prescribed treatment. Moreover, during the first year after therapy, patients experience a relapse in 30% of cases.
Source: //cmsch71.ru/molochnitsa/prodolzhitelnost-zhizni-pri-rake-shejki-matki.html