Classification of cervical cancer
Like other malignant diseases, cervical cancer is classified depending on the severity of the stage of development of oncological processes. There are four stages of cervical cancer:
Stage 1 - the malignant tumor is localized exclusively on the cervix. The results of treatment started on time are favorable; 90% of patients survive within five years.
Stage 2 - the tumor grows, leaves the cervix, but does not affect neighboring organs. Survival rate is 75%.
Stage 3 - cancer cells develop on the walls of the pelvis, and timely therapy guarantees survival in only 40% of women.
Stage 4 - the tumor spreads beyond the pelvic organs and affects the bladder. Metastasis to distant sites is observed. Complete recovery is observed in only 15% of patients.
Timely diagnosis allows you to identify a tumor in the early stages of development and helps to begin the correct treatment at each stage.
Classification
Malignant and benign neoplasms can occur on the cervix; there are pre-tumor and background pathologies, in which the risk of tissue degeneration is high and constant medical supervision is required.
When malignant formations are detected on the cervix of the uterus, an additional oncological scale is used to assess the degree of spread of metastases to nearby organs and the invasiveness of the tumor - this makes it possible to determine the stage of development of the disease.
If the tumor grows deeper, it is called endophytic, but if the tumor grows beyond the outer limits of the organ, it is called exophytic. Endophytic neoplasms are divided into germinating and non-invasive.
What are the types of formations on the cervix:
- Formations of glandular and squamous epithelial origin are often diagnosed and are considered potentially dangerous. Squamous cell – papillomas, condylomas, Nabothian follicles, carcinomas of the verrucous, papillary type. Glandular neoplasms – cervical canal polyp, Müllerian papilloma, glandular dysplasia, carcinomas and adenocarcinomas.
- Mesenchymal formations – leiomyomas, various types of sarcomas.
- Uterine fibroids, which are formed from muscle cells.
- Formations in which epithelial and stromal tissues are present are called mixed.
- Tumors of other types are blue and melanocytic nevus, melanoma, lymphoma, teratoma.
- Cervical stenosis - hematometers, pyometras appear, the cervix becomes swollen and increases in size. In elderly women, such manifestations indicate atrophy of organ tissue.
- Primary and secondary malignant formations.
- Neoplasms from metastases.
Formations can occur in the mucous membrane of the vaginal cervix, in the cervical canal, in the muscle layer or connective tissue. Only histological examination allows us to identify the type of tumor, the likelihood of malignancy, and create the correct treatment regimen.
Causes of cervical cancer
There are many reasons for the development of this disease. The top priority among them is the human papillomavirus, which can reside in the body of an absolutely healthy person and will not wither for many years. Human papillomavirus infection is a dormant type, but can manifest itself in the form of growths on the skin or warts. It is this infection that 100% leads to the manifestation of a malignant tumor in the cervical cavity. Modern research in the field of medicine distinguishes almost fifty varieties of human papillomaviruses, which can manifest themselves in the genital area and are sexually transmitted in nature. Anogenital type papillomas are usually divided into two small groups. The main criterion for division is their ability to become malignant. The following types of human papillomavirus have a high level of carcinogenic risk: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68. The above viruses are quite dangerous to health, but in a small percentage of women, infected with papilloma, a malignant formation develops.
All other types of the virus do not pose any particular danger, and therefore belong to the group with a low carcinogenic risk. Types 6 and 11 often appear as condylomas and never develop into a malignant tumor. The aesthetic appearance of the formations can cause some discomfort, so for hygienic reasons it is recommended to remove them.
To determine the stage of cervical cancer, the development of which is provoked by the papilloma virus, it is necessary to carefully monitor cytological changes and undergo regular tests. The most optimal way to detect changes at the cellular level is considered to be a Pap smear. The gynecologist must take this smear from absolutely all patients during an annual routine examination. Further laboratory testing will indicate therapy to be administered for abnormal indications. If the result of the smear examination raises suspicions among the doctor, additional DNA and HPV tests are prescribed. Even if the detected virus belongs to a group with cancer risk, this does not mean the presence of cancer cells. Therefore, there is no need to worry ahead of time. To exclude the development of a malignant tumor of the cervix, it is necessary to conduct additional tests: biopsy and colposcopy. Timely diagnosis of cancer cells allows you to select the most effective methods of influencing malignant cells. Timely treatment can prevent the possible manifestation of malignant tumors in the uterine cavity and on its cervix.
Scientists have repeatedly proven that human papillomavirus is transmitted through sexual contact and is distinguished by its transient nature. Women should realize that an annual examination should become an integral part of their lives, since it is quite simple to remove identified foci of the virus in the early stages of development.
The causes of cervical cancer may be the following:
- early onset of sexual activity and sexual maturity of girls under eighteen years of age;
- promiscuity;
- smoking more than five cigarettes in one day;
- refusal to use condoms, which allows sexually transmitted infections to penetrate the female body without barriers;
- lack of hygienic care for the genitals;
- insufficient intake of vitamins A and C;
- the presence of herpes virus and HPV in the body.
Mature and elderly women are at greatest risk. The majority of patients suffering from cervical cancer are observed in this age category. Young girls suffer much less from the development of a tumor on the cervix.
What kind of disease is this, what is the prognosis for life and reproductive function, and what should be done?
The word erosion in Latin means a defect in a surface. In our case, this is a defect in the cervical mucosa. I would like to draw your attention to the fact that the phrase “cervical erosion” is a collective medical term. The doctor makes such a very inaccurate diagnosis by examining the patient in mirrors with the naked eye. Most often, he sees redness in part of the cervix. To make an accurate diagnosis, it is necessary to undergo an “extended colposcopy” procedure. It involves examining the cervix using a colposcope (similar to a microscope), and performing tests using special solutions to stain the cervix. All these manipulations are absolutely harmless and painless (they are carried out even during pregnancy). There is only one contraindication: an allergy to iodine, because. it is used in samples. In addition to colposcopy, the doctor is required to take smears from the surface of the cervix. Which ones exactly? The most important is a smear for oncocytology, i.e. for the presence of abnormal, precancerous and cancerous cells.1 Next are smears for the degree of purity (for flora) and for the determination of STIs using the PCR method. Only after receiving all the examination data can the doctor make an accurate diagnosis and prescribe treatment.
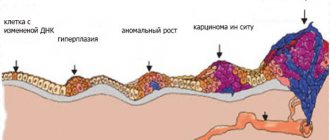
It happens that redness of the cervix is caused only by an infectious process, and it is enough to cure it so that the cervix takes on its normal color. In other cases, growth of glandular tissue (ectopia) is visible on the visible part of the cervix. This tissue is normally located in the cervical canal, but in various situations it goes beyond its limits, outward. The body tries to cure itself, and the ectopia is slowly overgrown with vaginal epithelium. It is during the healing process of ectopia that various malfunctions can occur and abnormal cells appear, especially when harmful bacteria and viruses settle on the cervix. Some infections cause acute symptoms and changes in the cervix, while others can remain inside the cells for a very long time and not manifest themselves for years. But this does not mean at all that the latter are weak or not very dangerous. It has been proven that many of them, for example, the human papillomavirus, are integrated into the genome of the host cell and make it work for itself. In this case, the cell changes, loses its original functions and qualities and acquires new ones (for example, rapid growth and reproduction).
All cells together make up the tissue - the integumentary epithelium of the cervix, which, accordingly, also changes. It is these changes that are visible upon examination. The next mandatory stage of diagnosis is a cervical biopsy. Using a special instrument, the doctor plucks off a small piece from a suspicious area of the cervix and sends it for an even more detailed examination - histological, during which they evaluate not only the condition of individual cells, but also the condition of all the tissues that form the cervix. If there are no signs of cancer, then treatment is carried out by a gynecologist. If so, the patient is referred to a gynecological oncologist.
The prognosis for benign diseases of the cervix, including ectopia, is favorable both for life and for the birth of children.
There are tactics for treating ectopia only after the first birth. In this case, the woman must undergo the above examination annually, except for a biopsy, which is done immediately before treatment. If precancerous diseases are detected, treatment is not delayed, and the prognosis can be favorable. When diagnosing cervical cancer, the prognosis depends on the stage of the process: the lower the stage, the more favorable the prognosis and the greater the chance of a 100% cure.
Genital warts (papillomas) - a sexually transmitted disease associated with the presence of the human papillomavirus in the body, can manifest as growths on the external genitalia, around the anus, in the vagina and on the cervix. The growths have a variety of shapes, from single cone-shaped growths to cauliflower-type growths. But there are also those that spread deep into the tissue and are therefore visible only during colposcopy. The examination is the same as for cervical erosion. The prognosis depends on the structure of the condyloma.
There are many methods for treating cervical diseases. We will touch on the treatment of benign diseases only. The very first method to use, cauterization of the cervix with electric current, has many contraindications and complications (it is not used in women who have not given birth). A more gentle technique is cryodestruction of the cervix with liquid nitrogen, which can be carried out in several stages, depending on the size of the defect. In this case, the healthy part of the cervix is not affected. Very often, in young girls with small ectopia, chemical treatment of the cervix with special solutions is used, but the frequency of return of ectopia after this method is quite high. Recently, progressive techniques using laser and radio wave energy have been widely used. Both methods have very few contraindications, good tolerability (no pain), a lasting effect of treatment, and it is possible to treat women who have not given birth.
Symptoms of cervical cancer
How to identify cervical cancer symptoms (the forum and the information provided on it can greatly help in this matter). One of the first symptoms indicating the development of a malignant tumor will be discharge from the genital area. Their formation indicates irreversible malignant processes in the lymph nodes and tumor tissues. Discharge from cervical cancer comes with blood clots and is watery in nature. Purulent leucorrhoea does not occur during the development of cancer. If discharge appears immediately after minor physical activity, this indicates contact bleeding - symptoms of early stage cervical cancer. Late stages of the disease are accompanied by additional symptoms: cutting pain, swelling, dysfunction of the urinary system.
The first symptoms of cervical cancer are not the only manifestation of the disease. In the later stages, pain appears after metastases involve the lymph nodes and pelvic organs. Pain is localized in the lumbar region, lower abdomen and rectal cavity.
Swelling appears on the hands and organs of the reproductive system already in the last stages of cancer progression. Metastases of the lymph nodes of the pelvic part of the body, blocking the work of large vessels, provoke swelling and worsen the body's water balance.
Frequent urination indicates a dysfunction of the urinary system. The walls of the bladder lose their anatomical features, its distensibility deteriorates. Partial emptying of the bladder leads to chronic cystitis. When the tumor begins to grow through the walls of the bladder, the formation of fistulas is also possible.
Disorders in the functioning of the intestines can manifest themselves in the form of constipation, disturbances in the contraction of the walls of the rectum and the formation of intestinal fistulas.
Diagnostics
To identify the type of neoplasm on the cervix, instrumental and laboratory research methods are used. Only after a thorough comprehensive examination can the nature, size, and phase of tumor development be determined.
What diagnostic methods are used to identify cervical formations?
During the examination, the doctor uses mirrors to assess the size, position and degree of mobility of the cervix, the presence and size of formations, and the nature of the discharge.
- Bimanual palpation is performed to assess the condition of the uterus.
- Rectovaginal diagnosis - it is carried out if there is a suspicion that the formation has penetrated the tissue of the rectum, or for virgins.
- Oncocytology smear (Pap test, Papanicolaou smear) – screening for early stages of cervical cancer.
- Colposcopy – the cervix is examined using a colposcope, tests are performed, and tissue samples are taken for biopsy.
- Targeted biopsy - tumor tissue is sent for histological and histochemical examination.
- Diagnostic curettage.
Additionally, the gynecologist may prescribe an ultrasound of the reproductive and pelvic organs, and lymph nodes. Using CT and MRI, the size of the formation, the condition of nearby organs, and lymph nodes in the pelvis are determined. If necessary, the doctor can write out a referral for sigmoidoscopy or cystoscopy.
In case of squamous cell neoplasms, dysplasia, or the presence of atypical cells in the epithelium, it is necessary to do a PCR analysis to identify the type of human papillomavirus.
Diagnosis of cervical cancer
Diagnosing a malignant tumor of the cervix in the final stages is very simple, since the majority of women complain of uncharacteristic bleeding from the vaginal area.
How to identify cervical cancer, symptoms? The initial examination in the gynecologist’s office is based on the study of the patient’s complaints and examination of the uterine cavity using a special gynecological speculum. If a gynecologist has suspicions about the condition of a particular area of the cervix, a biopsy and histological analysis are prescribed, which allows one to finally verify the correctness of the diagnosis. A general blood test is also performed for cervical cancer, or more precisely if it is suspected.
When examining the cervix, experts advise taking material for a Chrobak test - using a special umbrella to press on the area with the malignant tumor that has formed. This makes it possible to distinguish an inflammatory process from an oncological one. If cervical cancer has an endophytic form, the umbrella can penetrate the tumor tissue without much difficulty, but during an inflammatory process this is impossible.
When diagnosing, the Schiller test is often used, which is based on studying the reaction of the epithelium located on the upper part of the uterus. If the epithelium turns brown, then no cancerous tumor is detected; areas affected by cancer cells remain unpainted.
The results of a bimanual examination depend on the density of the uterine cervix and its level of mobility.
The development of a cancerous tumor is indicated by cervical hypertrophy, vaginal variant, enlarged uterine body, and manifestation of the tumor in parametric tissue.
To get a complete picture of the ongoing process, it is necessary to conduct a rectovaginal examination of the patient. In the early stages of the development of the disease, it is customary to use additional research methods such as cytology and colposcopy.
The patient’s medical history is also subject to careful examination, so the doctor must find out the presence of chronic inflammatory processes, pseudo-erosion, and polyps of the cervical canal. The number of births and the presence of spontaneously terminated pregnancies and medical abortions must be taken into account. The nature of sex life should not be overlooked. Promiscuous sexual relations cause the development of many diseases, not only cervical cancer. During interviews and clarification of complaints, the gynecologist clarifies deviations in the menstrual cycle and disorders of secretory function.
To confirm the diagnosis, scraping of material from the cervical canal is often used with further histological examination of the resulting scraping.
When the diagnosis has been confirmed, for the optimal choice of therapeutic method, the degree of spread of the malignant process is studied. Therefore, the doctor often prescribes a comprehensive examination of the body: lymphography, phlebography, arteriography, etc. Analysis of the diagnostics performed allows us to answer the main question: “Can cervical cancer be treated?”
Prognosis for cervical cancer
Can cervical cancer be cured? The prognosis for the first stage of cancer development is quite favorable, since the five-year survival threshold is 90% of the total number of patients. In the second stage, the five-year survival rate decreases significantly and is only 60%. At the third stage - 35%. The fourth stage is the most difficult to diagnose and treat, so the prognosis for recovery and survival is not very favorable - only 10% of all patients suffering from cervical cancer.
Cervical cancer treatment
The most effective is considered to be the beginning of cancer treatment in the first stages, when the tumor has not yet spread to the surrounding organs and tissues.
How to treat cervical cancer? When treating patients of childbearing age, doctors try to use all possible measures to preserve her reproductive function: excision of the area infected with cancer cells with a scalpel; laser removal, liquid nitrogen and ultrasonic removal.
Microinvasive cancer (the tumor grows three millimeters deep into the tissue) is subject to treatment with mandatory hysterectomy. Girls of childbearing age retain their appendages, but in older women they are subject to amputation. If lymph nodes are involved in the oncological process, they should also be removed. To obtain a better result, extirpation can be used in combination with radiation treatment.
Is cervical cancer curable at later stages of the malignancy process? At the second stage, radiation may be prescribed as an independent type of treatment. Non-surgical therapy can be carried out either through the vagina or externally. The choice of one or another method of therapy is based on the results of previous studies of the patient’s tests, an analysis of her general condition and her psychological readiness.
If the tumor has grown into the tissue of neighboring organs, the uterus may be removed along with parts of the affected organs. When a tumor reaches a large size, it may not be considered inoperable, so the doctor, in order to reduce the size of the tumor, prescribes radiation therapy to cancer cells. In the later stages of disease progression, patients undergo palliative surgery, which is aimed at alleviating the symptoms of cervical cancer.
Another method of treating cervical cancer is chemotherapy, which is used at the beginning of the metastasis process.
After long-term therapy, the patient is observed by a gynecologist and every three months comes to the office for colposcopy and smear analysis.
Under no circumstances should you self-medicate, as precious time is lost that could save the woman’s life.
How does the tumor manifest itself?
As a rule, a malignant neoplasm does not manifest itself in any way in the early stages. The disease is discovered by chance during a routine appointment with a gynecologist. The first symptoms of cancer are bloody vaginal discharge and profuse leucorrhoea. At first, discharge is observed during or after sexual intercourse; over time, it appears periodically due to the destruction of deeper capillaries by the tumor. Occasional watery discharge may occur.
As the tumor disintegrates, the discharge becomes pus-like and acquires a foul odor. In later stages, pain in the lower abdomen also appears. This is due to the fact that the tumor begins to compress the nerve endings in the sacrum area. It extends to parametric tissue.
If the neoplasm compresses the lymphatic vessels, then lymph stagnation begins in the legs. The development of a neoplasm at the same stage leads to disturbances in the outflow of urine and renal failure. At a later stage, the cancer spreads to the bladder, so diuretic disorders are added to the symptoms. Disturbances in bowel movements may occur due to damage to the rectum. In complex cases, severe complications develop and their symptoms are added. Such complications include peritonitis and uremia.
Be sure to read: How long do people live with spinal cancer?
Prevention of cervical cancer
The most effective method of prevention rightfully remains gynecological examinations at least once a year. In addition to the initial examination, it is imperative to undergo an analysis of smears taken from the cervical cavity and cervical canal. If your gynecologist has detected suspicious activity of the human papillomavirus, unquestioningly follow his recommendations and instructions. Considering the risk of developing cancer due to the presence of papillomas, experts advise vaccination against this type of virus. Unfortunately, such vaccinations are not yet so often used in our medicine, although all over the world they have proven themselves to be a worthy way to protect against the development of a malignant tumor. Vaccination is necessary before the start of sexual activity - up to 26 years of age.
From childhood, little girls need to be taught about the rules of self-care and about mandatory hygienic care of the external genitalia. During puberty, a child should be told about sexual intimacy and sexually transmitted infections. Particular attention should be paid to information about condoms and the importance of their use. Sex education will help protect a child from rash actions and possible consequences.