Parakeratosis
Parakeratosis is a pathological condition that is accompanied by keratinization and other changes in epithelial tissues. At the same time, the deformed uterus has a wrinkled appearance.
Most often, the development of parakeratosis occurs for the following reasons:
- hormonal imbalance in the female body;
- human papillomavirus and other viral infections;
- chaotic intimate life;
- gonorrhea, chlamydia and other sexually transmitted diseases;
- damage to the uterine cervix during childbirth, abortion, and various gynecological procedures.
In some cases, the cause of parakeratosis lies in a decrease in the level of immunity, as well as various gynecological diseases in the pelvic area.
If the disease is not detected and treated in a timely manner, the outer layer of the cervix becomes covered with whitish spots and dots, which are evidence of keratinization of the skin.
Medical experience confirms that in most cases the pathology is completely asymptomatic and is discovered completely by accident during a gynecological examination. Sometimes a woman may be bothered by vaginal discharge with a strong, unpleasant odor, which may contain blood, as well as pain and discomfort after sexual intercourse.
general information
Pelvic inflammatory disease (PID) is an infection of the upper female genital organs (uterus, fallopian tubes, and ovaries).
- PID is usually transmitted during sexual intercourse with an infected partner.
- Typically, women experience pain in the lower abdomen, vaginal discharge, and irregular vaginal bleeding.
- Diagnosis is made based on symptoms, analysis of cervical and vaginal discharge, and sometimes ultrasound.
- Having sex with only one partner and using condoms reduces the risk of infection.
- Antibiotics can clear up the infection.
Pelvic inflammatory disease can be caused by infection:
- uterine mucosa (endometritis);
- fallopian tubes (salpingitis);
- both.
If the infection is severe, it may:
- spread to the ovaries (oophoritis);
- lead to the accumulation of pus in the fallopian tubes (tubo-ovarian abscess).
PID is the most common preventable cause of infertility. Infertility occurs in about one in five women with PID.
In about one third of women who have had PID, the infection recurs.
PID usually occurs in sexually active women. The disease rarely occurs in girls before their first period (menarche) or in women during pregnancy or after menopause. The risk increases for the following categories of women:
- sexually active and under 35 years of age;
- those whose partner does not use a condom;
- those with multiple sexual partners or a new sexual partner;
- those infected with sexually transmitted infections or women with bacterial vaginosis;
- those who have had pelvic inflammatory disease in the past;
- those with low socioeconomic status (who typically have less access to health care).
Blueness of the cervix
Blueness of the cervix is a fairly common problem that many representatives of the fair sex face. Normally, the vagina and mucous surface of the cervix have a healthy beige-pink color. If the cervix acquires a bluish tint, this condition is called cyanosis.
Inflammation, hyperemia and cyanosis of the mucous surface of the cervix are a common sign of pregnancy. The main reason for the change in color of the mucous surface of the cervix is poor circulation in the pelvic organs. But in most cases, blueing of the epidermis is the result of hormonal changes in the female body that accompany pregnancy. In this case, the level of progesterone in the blood increases significantly, which clearly indicates the presence of pregnancy.
In order to definitively determine that a woman has succeeded in becoming pregnant, an ultrasound examination is recommended.
Redness or blue discoloration of the mucous surface of the cervix is a common symptom of many gynecological diseases, which include:
- Dysplasia.
- Pseudo-erosion.
- Leukoplakia.
- Adnexitis.
- Endometritis.
- Cervicitis.
- Condyloma.
- Eversion of the mucous membrane of the uterine cervix.
- Polyp.
- Prolapse or prolapse of the uterus.
- A tumor of a benign or malignant nature.
For these diseases, modern gynecology also offers the name background process.
If the epithelium of the uterine cervix acquires a bluish tint, this may indicate a precancerous process in the pelvic area. In order to diagnose cancer at the earliest stages, a tissue biopsy is performed. That is why any change in the normal, healthy color of the mucous surface should be a reason for an urgent visit to the gynecologist.
Cervicitis and endocervicitis
Cervicitis and endocervicitis are inflammatory processes, the form of which can differ significantly depending on which part of the cervix was hyperemic.
Main forms of the disease:
- inflammation or atrophy of the cervical canal;
- pathology affecting the vaginal area of the cervix.
Cervicitis and endocervicitis can be acute or chronic. The most common causes of the disease are associated with the penetration of infection into the vaginal opening, as well as mechanical injury to the reproductive organ during childbirth, abortion, gynecological curettage or installation of an intrauterine device.
Types of cervicitis:
- Spicy.
- Chronic.
- Purulent.
An acute edematous process is accompanied by symptoms such as discharge of mucus from the vagina, the consistency of which is foamy, a feeling of itching and burning in the genital area, heaviness, aching pain in the lower abdomen. Also, a woman is often worried about blood in the middle of the menstrual cycle or after sexual intercourse.
The chronic stage of cervicitis develops due to uterine prolapse, neglect of intimate hygiene rules, and the use of hormonal contraceptives. With this form of the disease, the symptoms appear vaguely; in some cases, the patient is bothered by a frequent urge to urinate, scanty vaginal discharge of a mucous nature, and aching, nagging pain in the lower abdomen.
The purulent form of cervicitis is characterized by copious purulent discharge from the cervical canal. At the same time, the mucous membrane of the cervix can become quite hyperemic. Infection with purulent cervicitis occurs through sexual contact; the main pathogens are sexually transmitted diseases, chlamydia or gonococci.
Inflammatory diseases of the female genital organs
Vulvitis is an inflammation of the mucous membrane of the vaginal vestibule. It develops mainly in girls. Infection is promoted by diaper rash, scratching, abrasions, endocrine pathology (IDDM), helminthic infestations, and childhood viral infections. In adults, as a rule, vulvitis is combined with inflammation of the vaginal mucosa.
Clinic: pain, swelling of the vulva, purulent discharge.
Bartholinitis is an inflammation of the large glands of the vaginal vestibule. Very often, if the rules of genital hygiene are not observed, various bacteria and STIs get into it. Its excretory duct becomes clogged and an inflammatory process occurs in the gland. Unilateral damage to the Bartholin gland is more common.
It first appears as redness around the external opening of the excretory duct, then inflammatory swelling can clog the gland duct, preventing the release of purulent secretion, which, lingering in the duct, stretches it, forming a false abscess (ulcer), which protrudes the inner surface of the labia majora and closes the entrance to the vagina . Body temperature and soreness in the perineal area may increase. In rare cases, the inflammatory process can directly involve the gland tissue, resulting in a true abscess with severe suppuration and enlargement of the gland. The labia majora and minora are swollen. The inguinal lymph nodes are enlarged. Body temperature rises. A true abscess differs from a false abscess by constant pain, severe swelling of the labia, immobility of the skin over the abscess, and high fever.
The abscess can spontaneously open with the flow of thick yellow-green contents, after which the condition improves. The inflammatory process can die out on its own (without suppuration). In this case, compaction and slight enlargement of the gland are observed. However, quite often after some time the inflammatory process resumes and becomes more complicated.
Colpitis is inflammation of the vagina (vaginitis).
The clinical picture includes a triad of symptoms: pain, leucorrhoea, itching.
Colpitis can be caused by gonococci, trichomonas, chlamydia, as well as conditionally pathogenic microorganisms such as staphylococci, streptococci, fungi of the genus Candida, E. coli, etc. There are acute and permanent vaginitis. During an acute process, women complain of itching in the area of the vaginal vestibule, burning, a feeling of pressure, heat in the genitals and pelvis, many note dysuric disorders. Characteristic is copious discharge - leucorrhoea. The inflammatory process caused by various pathogens has its own characteristics. For example, profuse, frothy, yellowish-green discharge with an unpleasant odor is characteristic of Trichomonas vaginitis; discharge of a white, curd-like appearance - for fungal. In chronic forms of inflammation, there is no pain; patients mainly complain of discharge, itching, burning, and small ulcerations in the area of the vaginal vestibule.
Bacterial vaginosis (diagnosed since 1980) Gardner's disease. The only complaints are about increased discharge of leucorrhoea (profuse discharge, foul-smelling). There are no symptoms of inflammation. Often women complain of discomfort and burning in the vagina. Recently, bacterial vaginosis has been considered as a kind of vaginal dysbacteriosis, which occurs when the number of lactobacilli secreting lactic acid decreases and the pH of the vaginal secretion increases (more than 4.5). This creates conditions for the massive proliferation of microorganisms such as gardnerella and obligate anaerobic bacteria. This disease is rare in prepubertal girls and postmenopausal women, indicating a significant hormonal component in causing this imbalance.
Cervicitis is an inflammation of the cervix, which occurs as a result of penetration of gonococci, trichomonas, chlamydia, staphylococci, streptococci and other bacteria, and less commonly viruses, into the cervical canal. The occurrence is facilitated by cervical ruptures during childbirth, prolapse of the genital organs, infectious processes in the vagina and, conversely, in the internal genital organs. In an acute process, a woman is bothered by mild pain in the lower abdomen, discomfort in the vagina, sometimes itching, mucous or purulent mucous discharge from the vagina, pain during sexual intercourse. In a chronic process, complaints are less pronounced.
Endocervicitis is an inflammation of the mucous membrane of the cervical canal. It can occur with the penetration of various bacteria (staphylococci, streptococci, gonococci, intestinal Escherichia, etc.). Endocervicitis is often combined with an inflammatory process in other parts of the reproductive system - colpitis, salpingoophoritis, cervical erosion.
Symptoms: mucopurulent vaginal discharge, no pain. Clinical signs are mild. In the acute stage, hyperemia around the external pharynx and mucopurulent discharge are determined. In the chronic stage there is almost no hyperemia, the discharge remains. With a long course of the process, hypertrophy (thickening) of the cervix develops - cervicitis
Condylomas acuminata (multiple growths on the surface of the external genitalia and vaginal opening). May spread to the perineum, vagina, cervix. The cause of condylomas is a filterable virus (human papillomavirus); the development of the process is facilitated by abundant discharge from the genital tract during colpitis and endocervicitis. Genital warts grow very quickly during pregnancy.
Symptoms: condylomas are most often localized on the external genitalia, perineum, and around the anus. In cases of necrosis of condylomas and the addition of a secondary infection, purulent discharge appears. Condylomas of the vagina and cervix during pregnancy and childbirth can cause bleeding. The diagnosis is made based on examination.
Basic diagnostic methods
In order to quickly and effectively get rid of a gynecological disease, it is necessary to consult a specialist immediately after the first symptoms of the pathology appear. The doctor will conduct a full examination of the genital organs and prescribe all the necessary tests and examinations.
The most accurate and informative diagnostic measures:
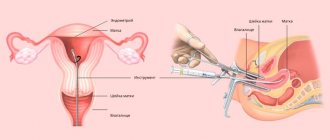
- gynecological examination of the reproductive organs, carried out using special mirrors;
- bacteriological study of a vaginal smear;
- cytogram - a cytological study through which the cell of the uterine cervix, its size and condition are studied;
- general clinical analysis of blood and urine;
- PCR is a laboratory study of vaginal mucus, which is used to identify infectious agents;
- Ultrasound - helps to determine the inflammatory uterine process in its earliest stages;
- colposcopy - performed using a special instrument called a colposcope and allows you to carefully examine all the pelvic organs.
In order to clarify and confirm the presence of an inflammatory process in the uterus, a biochemical analysis for tumor markers or a biopsy are additionally prescribed.
Treatment
The success and duration of treatment depends on the individual characteristics of the female body and the development of inflammation, so therapy is selected for each patient individually.
For inflammatory diseases of the cervix, it is recommended to take antibacterial drugs, immunomodulators, and multivitamin complexes. Antibacterial therapy is aimed at stopping the pathological process, eliminating its symptoms and causes. Among the most effective and efficient medications are the following:
- Erythromycin;
- Levofloxacin;
- Ofloxacin;
- Doxycycline;
- Tetracycline;
- Ceftriaxone;
- Azithromycin;
- Roxithromycin.
For genital hygiene, medications from the group of antiseptics are used - Miramistin, Chlorhexidine, Chlorophyllipt, Malavit.
Treatment of the inflammatory process provoked by Trichomonas is carried out with the help of drugs such as Novonidazole, Trichopolum, Efloran, Metronidazole and its other analogues.
It is important to remember that in the presence of inflammatory diseases of the uterine cervix, which are infectious in nature, treatment is carried out immediately in both partners, even if the man does not have any symptoms of inflammation.
For cervicitis and endocervicitis, it is very useful to regularly take sitz baths with decoctions of medicinal herbs - chamomile, oak bark, calendula flowers. For hygiene procedures, it is also recommended to use herbal infusions, replacing cosmetics with them. Maximum attention should be paid to maintaining intimate hygiene, washing the genitals with warm water at least 2 times a day.
Inflammation of the cervix is a serious gynecological disease that can have the most dangerous consequences for the female body, including the development of cancer or infertility. It is for this reason that any inflammation should be taken as seriously as possible and be sure to seek medical help when the first signs of the disease appear.
Video: chronic endometritis
Chronic endometritis
Inflammatory diseases of the pelvic organs in women
V. N. Kuzmin
Doctor of Medical Sciences, Professor, MGMSU, Moscow
Pelvic inflammatory diseases (PID) are characterized by various manifestations depending on the level of damage and the strength of the inflammatory response. The disease develops as a result of penetration of a pathogen (enterococci, bacteroids, chlamydia, mycoplasmas, ureaplasmas, trichomonas) into the genital tract and in the presence of favorable conditions for its development and reproduction. Such conditions are created in the postpartum or post-abortion period, during menstruation, during various intrauterine manipulations (insertion of an IUD, hysteroscopy, hysterosalpingography, diagnostic curettage) [1, 5].
Existing natural protective mechanisms, such as anatomical features, local immunity, the acidic environment of the vaginal contents, the absence of endocrine disorders or serious extragenital diseases, can in the vast majority of cases prevent the development of genital infection. An inflammatory response occurs to the invasion of a particular microorganism, which, based on the latest concepts of the development of the septic process, is usually called a systemic inflammatory response [16].
Acute salpingoophoritis
It is one of the most common diseases of inflammatory etiology in women. Every fifth woman who has suffered salpingo-oophoritis is at risk of infertility. Adnexitis can cause a high risk of ectopic pregnancy and pathological course of pregnancy and childbirth. The fallopian tubes are the first to be affected, and the inflammatory process can involve all layers of the mucous membrane of one or both tubes, but more often only the mucous membrane of the tube is affected, and catarrhal inflammation of the mucous membrane of the tube occurs - endosalpingitis. Inflammatory exudate, accumulating in the tube, often flows through the ampullary opening into the abdominal cavity, adhesions form around the tube, and the abdominal opening of the tube closes. A saccular tumor develops in the form of a hydrosalpinx with transparent serous contents or a pyosalpinx with purulent contents. Subsequently, the serous exudate of the hydrosalpinx resolves as a result of treatment, and the purulent pyosalpinx can perforate into the abdominal cavity. The purulent process can capture and melt increasingly large areas of the pelvis, spreading to all internal genitalia and nearby organs [9, 10, 13].
Inflammation of the ovaries (oophoritis) as a primary disease is rare; infection occurs in the area of the ruptured follicle, since the rest of the ovarian tissue is well protected by the covering germinal epithelium. In the acute stage, edema and small cell infiltration are observed. Sometimes, in the cavity of the follicle of the corpus luteum or small follicular cysts, ulcers and microabscesses form, which, merging, form an ovarian abscess, or pyovarium. It is almost impossible to diagnose an isolated inflammatory process in the ovary, and this is not necessary. Currently, only 25-30% of patients with acute adnexitis have a pronounced picture of inflammation, while the rest experience a transition to a chronic form, when therapy is stopped after the clinic quickly subsides.
Acute salpingoophoritis is treated with antibiotics (preferably third generation fluoroquinolones - ciprofloxacin, tarivid, abactal), since it is often accompanied by pelvioperitonitis - inflammation of the pelvic peritoneum.
Endometritis
Acute endometritis always requires antibacterial therapy. The basal layer of the endometrium is affected by the inflammatory process due to the invasion of specific or nonspecific pathogens. Endometrial protective mechanisms, congenital or acquired, such as T-lymphocyte aggregates and other elements of cellular immunity, are directly related to the action of sex hormones, especially estradiol. These mechanisms act in conjunction with the macrophage population and protect the body from damaging factors. With the onset of menstruation, this barrier on a large surface of the mucous membrane disappears, which makes it possible to become infected. Another source of protection in the uterus is the infiltration of the underlying tissues with polymorphonuclear leukocytes and the rich blood supply of the uterus, which promotes adequate perfusion of the organ with blood and nonspecific humoral protective elements contained in its serum: transferrin, lysozyme, opsonins [16].
The inflammatory process can spread to the muscle layer, resulting in metroendometritis and metrothrombophlebitis with a severe clinical course. The inflammatory reaction is characterized by a disorder of microcirculation in the affected tissues, expressed by exudation; with the addition of anaerobic flora, necrotic destruction of the myometrium can occur [12].
Clinical manifestations of acute endometritis: already on the 3-4th day after infection, an increase in body temperature, tachycardia, leukocytosis and a shift in the blood, an increase in ESR are observed. Moderate enlargement of the uterus is accompanied by pain, especially along its ribs (along the blood and lymphatic vessels). Purulent-bloody discharge appears. The acute stage of endometritis lasts 8-10 days and requires quite serious treatment. With proper treatment, the process ends, less often it turns into a subacute and chronic form, and even less often, with self-administered indiscriminate antibiotic therapy, endometritis can take a milder abortive course [5, 12].
Treatment of acute endometritis, regardless of the severity of its manifestations, begins with antibacterial infusion, desensitizing and restorative therapy.
Antibiotics are best prescribed taking into account the sensitivity of the pathogen to them; doses and duration of antibiotic use are determined by the severity of the disease. Due to the frequency of anaerobic infections, metronidazole is additionally recommended. Considering the very rapid course of endometritis, cephalosporins with aminoglycosides and metronidazole are preferred among antibiotics. For example, cefamandole (or cefuroxime, claforan) 1-2 g 3-4 times a day IM or IV drip + gentamicin 80 mg 3 times a day IM + Metrogyl 100 ml IV drip.
Instead of cephalosporins, you can use semi-synthetic penicillins (for abortive cases), for example, ampicillin 1 g 6 times a day. The duration of such combined antibacterial therapy depends on the clinic and laboratory response, but not less than 7-10 days. To prevent dysbiosis from the first days of antibiotic treatment, use nystatin 250,000 units 4 times a day or diflucan 50 mg per day for 1-2 weeks orally or intravenously [5].
Detoxification infusion therapy may include a number of infusion agents, for example, Ringer-Locke solution - 500 ml, polyionic solution - 400 ml, hemodez (or polydesis) - 400 ml, 5% glucose solution - 500 ml, 1% calcium chloride solution - 200 ml, unithiol with a 5% solution of ascorbic acid, 5 ml 3 times a day. In the presence of hypoproteinemia, it is advisable to carry out infusions of protein solutions (albumin, protein), blood replacement solutions, plasma, red blood cells or whole blood, and amino acid preparations [12].
Physiotherapeutic treatment occupies one of the leading places in the treatment of acute endometritis. It not only reduces the inflammatory process in the endometrium, but also stimulates ovarian function. When normalizing the temperature reaction, it is advisable to prescribe low-intensity ultrasound, inductothermy with an HF or UHF electromagnetic field, magnetic therapy, and laser therapy.
Pelvioperitonitis
Inflammation of the pelvic peritoneum most often occurs secondary to the penetration of infection into the abdominal cavity from an infected uterus (with endometritis, infected abortion, ascending gonorrhea), fallopian tubes, ovaries, intestines, with appendicitis, especially with a pelvic location. In this case, an inflammatory reaction of the peritoneum is observed with the formation of serous, serous-purulent or purulent effusion. The condition of patients with pelvioperitonitis remains satisfactory or moderate. The temperature rises, the pulse quickens, but the function of the cardiovascular system is almost not impaired. With pelvioperitonitis, or local peritonitis, the intestine remains unbloated, palpation of the upper half of the abdominal organs is painless, and symptoms of peritoneal irritation are determined only above the pubis and in the iliac regions. However, patients note severe pain in the lower abdomen, there may be retention of stool and gas, and sometimes vomiting. The level of leukocytes is increased, the formula shifts to the left, the ESR is accelerated. Gradually increasing intoxication worsens the condition of patients [14, 15].
Treatment of salpingoophoritis with or without pelvioperitonitis begins with a mandatory examination of the patient for flora and sensitivity to antibiotics. Most importantly, the etiology of inflammation should be determined. Today, benzylpenicillin is widely used for the treatment of specific gonorrheal process, although preference should be given to drugs such as Rocephin, Cephobid, Fortum.
The “gold standard” of antibacterial therapy for salpingoophoritis is the prescription of claforan (cefotaxime) at a dose of 1-2 g 2-4 times a day intramuscularly or one dose of 2 g intravenously in combination with gentamicin 80 mg 3 times a day (can Gentamicin is administered once at a dose of 160 mg IM). It is imperative to combine these drugs with Metrazdil, which is administered intravenously at a dose of 100 ml 1-3 times a day. The course of antibiotic treatment should be carried out for at least 5-7 days, you can vary mainly basic drugs by prescribing cephalosporins of the second and third generation (Mandol, Zinacef, Rocephin, Cephobid, Fortum and others at a dose of 2-4 g per day) [14].
In case of acute inflammation of the uterine appendages, complicated by pelvioperitonitis, oral administration of antibiotics is possible only after the main course of therapy and only if necessary. As a rule, such a need does not arise, and the persistence of previous clinical symptoms may indicate that the inflammation is progressing and, possibly, a suppurative process is occurring.
Detoxification therapy is mainly carried out with crystalloid and detoxification solutions in an amount of 2-2.5 liters with the inclusion of solutions of hemodez, rheopolyglucin, Ringer-Locke, polyionic solutions - acessol, etc. Antioxidant therapy is carried out with a solution of unithiol 5 ml with a 5% solution of ascorbic acid 3 times a day intravenously [14].
In order to normalize the rheological and coagulation properties of blood and improve microcirculation, aspirin 0.25 g/day is used for 7-10 days, as well as intravenous administration of rheopolyglucin 200 ml (2-3 times per course). Subsequently, a complex of resorption therapy and physiotherapeutic treatment is used (calcium gluconate, autohemotherapy, sodium thiosulfate, humisol, plasmol, aloe, FIBS) [3, 15]. Of the physiotherapeutic procedures for acute processes, ultrasound is appropriate, which causes analgesic, desensitizing and fibrolytic effects, as well as strengthening metabolic processes and tissue trophism, inductothermy, UHF therapy, magnetic therapy, laser therapy, and subsequently sanatorium-resort treatment.
Purulent tubo-ovarian formations
Among 20-25% of patients suffering from inflammatory diseases of the uterine appendages, 5-9% develop purulent complications requiring surgical interventions [9, 13].
The following provisions regarding the formation of purulent tubo-ovarian abscesses can be highlighted:
- chronic salpingitis in patients with tubo-ovarian abscesses is observed in 100% of cases and precedes them;
- the spread of infection occurs predominantly through the intracanalicular route from endometritis (with IUD, abortion, intrauterine interventions) to purulent salpingitis and oophoritis;
- there is often a combination of cystic transformations in the ovaries and chronic salpingitis;
- there is a mandatory combination of ovarian abscesses with exacerbation of purulent salpingitis;
- Ovarian abscesses (pyovarium) are formed mainly from cystic formations, often microabscesses merge.
Morphological forms of purulent tubo-ovarian formations:
- pyosalpinx - predominant lesion of the fallopian tube;
- pyovarium - predominant damage to the ovary;
- tubo-ovarian tumor.
All other combinations are complications of these processes and can occur:
- without perforation;
- with perforation of ulcers;
- with pelvioperitonitis;
- with peritonitis (limited, diffuse, serous, purulent);
- with pelvic abscess;
- with parametritis (posterior, anterior, lateral);
with secondary lesions of adjacent organs (sigmoiditis, secondary appendicitis, omentitis, interintestinal abscesses with the formation of fistulas).
Clinically differentiating each localization is almost impossible and impractical, since the treatment is fundamentally the same: antibacterial therapy in this case takes the leading place both in the use of the most active antibiotics and in the duration of their use. The basis of purulent processes is the irreversible nature of the inflammatory process. Its irreversibility is due to morphological changes, their depth and severity caused by impaired renal function [3, 9].
Conservative treatment of irreversible changes in the uterine appendages is unpromising, since it creates the preconditions for the occurrence of new relapses and aggravation of metabolic disorders in patients, increases the risk of upcoming surgery in terms of damage to adjacent organs and the inability to perform the required volume of surgery [9].
Purulent tubo-ovarian formations are associated with great difficulties both diagnostically and clinically. Nevertheless, a number of characteristic syndromes can be identified:
- intoxication;
- painful;
- infectious;
- early renal;
- hemodynamic disorders;
- inflammation of adjacent organs;
- metabolic disorders.
Clinically, intoxication syndrome is manifested by the phenomena of intoxication encephalopathy: headaches, heaviness in the head and severe general condition. Dyspeptic disorders (dry mouth, nausea, vomiting), tachycardia, and sometimes hypertension (or hypotension in the onset of septic shock, which is one of its early symptoms along with cyanosis and facial hyperemia against the background of severe pallor) are noted [4].
The pain syndrome, present in almost all patients, is of an increasing nature, accompanied by a deterioration in general condition and well-being; pain during a special examination and symptoms of irritation of the peritoneum around the palpable formation are noted. Pulsating increasing pain, persistent fever with a body temperature above 38°C, tenesmus, loose stools, lack of clear contours of the tumor, lack of effect from treatment - all this indicates the threat of perforation or its presence, which is an absolute indication for urgent surgical treatment. The infectious syndrome is present in all patients and is accompanied in most of them by high body temperature (38°C and above). Tachycardia corresponds to fever, as well as an increase in leukocytosis, the ESR and leukocyte index of intoxication increase, the number of lymphocytes decreases, the shift to the left increases, the number of molecules of average mass increases, reflecting ever-increasing intoxication. Often, due to impaired urine passage, renal dysfunction occurs. Metabolic disorders manifest themselves in the form of dysproteinemia, acidosis, electrolyte disturbances, and changes in the antioxidant system.
The treatment strategy for this group of patients is based on the principles of organ-preserving operations, which nevertheless provide for radical removal of the main source of infection. Therefore, for each specific patient, the time and scope of the operation must be selected individually. Clarifying the diagnosis sometimes takes several days, especially in cases where there is a borderline variant between suppuration and acute inflammatory process or in the differential diagnosis of an oncological process. Antibacterial therapy is required at each stage of treatment [1, 2].
Preoperative therapy and preparation for surgery include:
antibiotics (cephobid 2 g/day, fortum 2-4 g/day, reflin 2 g/day, augmentin 1.2 g intravenously once a day, clindamycin 2-4 g/day, etc.); they must be combined with gentamicin 80 mg IM 3 times a day and an infusion of Metragil 100 ml IV 3 times;
detoxification therapy with infusion correction of volemic and metabolic disorders;
mandatory assessment of the effectiveness of treatment based on the dynamics of body temperature, peritoneal symptoms, general condition and blood counts.
At the surgical stage, it is necessary to continue antibacterial therapy. It is especially important to administer one daily dose of antibiotics on the operating table, immediately after the end of the operation. This concentration is necessary because it creates a barrier to the further spread of infection: penetration into the area of inflammation is no longer prevented by dense purulent capsules of tubo-ovarian abscesses. Betalactam antibiotics (cephobid, rocephin, fortum, claforan, tienam, augmentin) overcome these barriers well.
Postoperative therapy involves continuing antibacterial therapy with the same antibiotics in combination with antiprotozoal, antimycotic drugs and uroseptics. The duration of treatment depends on the clinical picture and laboratory data (at least 7-10 days). The discontinuation of antibiotics is carried out in accordance with their toxic properties, therefore gentamicin is often discontinued first after 5-7 days of therapy or replaced with amikacin.
Infusion therapy should be aimed at combating hypovolemia, intoxication and metabolic disorders. Normalization of gastrointestinal motility is very important (intestinal stimulation, HBOT, hemosorption or plasmapheresis, enzymes, epidural blockade, gastric lavage, etc.). Hepatotropic, restorative and antianemic therapy is combined with immunostimulating treatment (UVR, laser blood irradiation, immunocorrectors) [2, 9, 11].
All patients who have undergone surgery for purulent tubo-ovarian abscesses require post-hospital rehabilitation in order to prevent relapses and restore specific body functions.
Literature
- Abramchenko V.V., Kostyuchek D.F., Perfileva G.N. Purulent-septic infection in obstetric and gynecological practice. St. Petersburg, 1994. 137 p.
- Bashmakova M. A., Korkhov V. V. Antibiotics in obstetrics and perinatology. M., 1996. P. 6.
- Bondarev N. E. Optimization of diagnosis and treatment of mixed sexually transmitted diseases in gynecological practice: Abstract of thesis. dis. ...cand. honey. Sci. St. Petersburg, 1997. 20 p.
- Ventsela R.P. Nosocomial infections. M., 1990. 656 p.
- Gurtovoy B. L., Serov V. N., Makatsaria A. D. Purulent-septic diseases in obstetrics. M., 1981. 256 p.
- Keith L. G., Berger G. S., Edelman D. A. Reproductive health. T. 2. Rare infections. M., 1988. 416 p.
- Krasnopolsky V.I., Kulakov V.I. Surgical treatment of inflammatory diseases of the uterine appendages. M., 1984. 234 p.
- Korkhov V.V., Safronova M.M. Modern approaches to the treatment of inflammatory diseases of the vulva and vagina. M., 1995. P. 7-8.
- Kumerle X. P., Brendel K. Clinical pharmacology during pregnancy / Ed. X. P. Kumerle, K. Brendel: Trans. from English In 2 volumes. T. 2. M., 1987. 352 p.
- Serov V.N., Strizhakov A.N., Markin S.A. Practical obstetrics: A guide for doctors. M., 1989. 512 p.
- Serov V.N., Zharov E.V., Makatsariya A.D. Obstetric peritonitis: Diagnosis, clinic, treatment. M., 1997. 250 p.
- Strizhakov A. N., Podzolkova N. M. Purulent inflammatory diseases of the uterine appendages. M., 1996. 245 p.
- Khadzhieva E.D. Peritonitis after cesarean section: Textbook. St. Petersburg, 1997. 28 p.
- Sahm DE The role of automation and molecular technology in antimicrobial susceptibility testing // Clin. Microb. And Inf. 1997. Vol. 3. No. 2. P. 37-56.
- Snuth CB, Noble V, Bensch R et al. Bacterial flora of the vagina during the mensternal cycle // Ann. Intern. Med. 1982. P. 48-951.
- Tenover F. Norel and emerging mechanisms of antimicrobial resistance in nosocomial pathogens // Am. J. Med. 1991. 91. P. 76-81.
The article was published in the journal The Attending Physician