What hormones are responsible for ovulation: types, norm and deviations
Conceiving and bearing a child occurs due to the interconnected work of the hypothalamus, pituitary gland, and ovaries.
One of their functions is to coordinate the production of hormones - biologically active organic substances. They regulate metabolic processes and affect the functioning of organs. Algorithm for starting the ovulatory process in a woman:
- enlargement of follicles under the influence of follicle-stimulating hormone (FSH). In this case, growth of one or more dominant follicles is observed;
- an increase in luteinizing hormone in the blood, its stimulating effect on estrogen synthesis and suppression of FSH secretion. As a consequence, the growth of non-dominant follicles fades;
- accumulation of estrogens, increased secretion of FSH, LH;
- a sharp increase in progesterone, LH, the onset of ovulation;
- formation of the corpus luteum, progesterone production;
- in the absence of pregnancy - suppression of the secretion of gonadotropins by steroids.
A necessary condition for the onset of ovulation is the growth of follicles. Hormones are responsible for this process in a woman’s body.
everything about health and medicine
The endocrine system is responsible for the normal functioning of the entire body, including fertility. According to experts, the problem of hormonal disorders affects about 30-40% of women who have problems conceiving.
According to statistics, doctors recommend that a woman who cannot become pregnant within a year undergo a comprehensive examination to determine the reproductive capacity of both partners.
Hormones that control fertility
A group of hormones are responsible for female fertility, primarily secreted by the hypothalamus, pituitary gland, ovaries and thyroid gland. In particular, these are:
- prolactin,
- luteinizing hormone LH,
- follicle stimulating hormone FSH,
- estradiol,
- testosterone,
- progesterone,
- thyroid hormones.
Prolactin is primarily responsible for proper lactation and is secreted by the pituitary gland.
Follicle stimulating hormone (FSH) and luteinizing hormone LH are released by the pituitary gland under the influence of proper stimulation through the hypothalamus.
The main task of FSH is to stimulate follicles to grow in the first phase of the monthly cycle, while a sharp increase in the hormone LH immediately before ovulation causes the final maturation of the egg in the follicle.
After ovulation, LH stimulates the formation and maintenance of corpus luteum function.
Estradiol is produced in the ovaries through growing and maturing follicles (which are stimulated to grow by FSH). During the menstrual cycle, the job of this hormone is to prepare the uterus for implantation (along with progesterone) and increase the secretion of fertile cervical mucus and libido.
Even more interesting:
Unidox solutab treatment
Eggworm photo of a child
Testosterone is produced by the ovaries and adrenal glands. Its excess may be associated with other hormonal disorders that lead to ovulation disorders.
Progesterone is secreted into the corpus luteum, which is formed in the ovary after ovulation under the influence of LH. Its task is to prepare the uterus for embryo implantation and maintain pregnancy. After 6 weeks from fertilization, the placenta takes over the production of progesterone.
Thyroid hormone - TSH. Just like FSH and LH, it is produced by the pituitary gland. An imbalance of thyroid hormones can reduce fertility and cause infertility in women.
Symptoms of hormonal disorders
Hormonal imbalance can be caused by diseases of the glands responsible for producing hormones.
The main signal indicating hormonal problems in women is ovulation disturbance. The most common cause of menstrual irregularities due to hormonal imbalance in the body is polycystic ovary syndrome. Less commonly, the cause is a high concentration of prolactin or impaired thyroid function.
Follicle stimulating hormone
FSH is produced by the anterior pituitary gland, where it then accumulates. Its release into the blood is observed every 1–4 hours. When the level of sex hormones is low, FSH increases, and when the level of sex hormones is high, it is inhibited.
FSH affects the maturation of follicles in the ovaries, prepares them for the effects of LH, and helps increase the concentration of estrogen.
Thanks to the action of FSH, the follicular phase occurs, which is necessary for the maturation of the egg. Under its influence, the level of estradiol increases, and before ovulation, a sharp increase in LH and FSH provokes the release of the egg.
If the follicles do not grow to the required size - 18–24 mm, ovulation does not occur.
You can determine the moment of release of the egg using the folliculometry method. This is monitoring the growth of the follicle from 8-10 days after the start of the menstrual cycle using ultrasound (interval - 2 days).
The dominant is visualized on the 10th day, its size reaches 12–15 mm. Under the influence of FSH, the dominant grows at a rate of 3 mm per day, and the remaining follicles regress. With normal levels of FSH, LH and estradiol, ovulation occurs on days 12–14 after the onset of menstruation, the average duration of which is 1.5 days.
If it is absent, the woman is tested for FSH levels. The results are assessed according to the following standards:
| Day after menstruation | FSH level value, mIU/ml |
| Period of menstrual bleeding, 1–6 | 3,5–12,5 |
| Follicular phase, 3–14 | |
| Ovulatory phase, 13–15 | from 4.7 to 21.5 |
| 15 – beginning of a new menstrual cycle | 1,7–7,7 |
| Menopause | 25,8–134,8 |
The best time to take an analysis to determine follicle maturation is days 5–8 of the menstrual cycle.
Luteinizing hormone
The pituitary gland is responsible for the production of gonadotropic ovulation hormone luteinizing hormone (LH). Its main task is to stimulate the production of estrogen by the ovaries.
LH is a complex glycoprotein protein. Its constituent alpha subunit repeats the components of FSH and human chorionic hormones. The beta subunit determines the action of LH. It consists of 121 amino acids, the sequence of which is the same as in hCG. Its activity depends on the amount of gonadotropin-releasing hormone, the production of which is responsible for the hypothalamus.
As the follicles mature, they stimulate the production of estrogen. Estradiol, produced by granulosa cells of the follicles, has the most powerful effect on the process of maturation and release of the egg. It is its increase that activates the hypothalamus and stimulates the pituitary gland to release LH and FSH.
At the same time, the concentration of LH increases so much that it triggers the process of releasing the egg. As a result of this process, the egg is released and the residual follicle becomes the corpus luteum.
A sharp increase in LH in the urine allows you to determine the period of ovulation using a test. A positive result on the strip indicates the likelihood of ovulation. The appearance period is 24–48 hours.
The temporary endocrine gland (corpus luteum) formed after the release of the egg is supported by luteinizing hormone for another 2 weeks. When pregnancy occurs, the luteal phase will be supported by the hormone hCG.
When determining the causes of difficulties with conception, the ratio of LH and FSH is analyzed.
LH norms
There are standard indicators:
| Period after menstruation, day | FSH level, mIU/ml |
| 1–6 | 2,4–12,6 |
| 2–15 | |
| 13–15 | from 14 to 96 |
| 15 | 1–11,4 |
| Menopause | 7,7–59 |
After puberty, the level of LH, the hormone responsible for ovulation, should be 1.5–2 times higher than FSH. A 1:1 hormone ratio is acceptable for girls at the stage of puberty.
If LH exceeds FSH by more than 2.5 times, this means the possible development of pathology:
- polycystic ovary syndrome;
- ovarian exhaustion;
- the occurrence of a pituitary tumor;
- ovarian hyperstimulation.
These conditions significantly reduce the likelihood of follicle maturation, egg release, and conception.
Estradiol
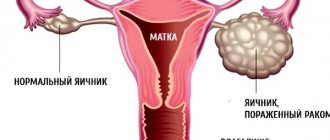
Of the group of estrogenic steroid hormones, estradiol has a greater effect on the functioning of the reproductive system in women. Its production occurs predominantly by the ovaries, a certain amount is produced by the adrenal cortex, and another small proportion is obtained as a result of the transformation of androgens and adipose tissue.
Estradiol does not have a direct effect on ovulation, however, it regulates the menstrual cycle and prepares the uterine mucosa for the implantation of a fertilized egg.
The level of estradiol in the blood depends on the time of day and the phase of a woman’s menstrual cycle. The peak growth of estradiol is associated with LH secretion. It occurs at 15–18 hours, 24–2 hours. The level of estradiol is minimal in women of childbearing age at the beginning of the menstrual cycle, and its maximum concentration is 24–36 hours before ovulation.
Small amounts of estrogen stimulate the growth of FSH, which is necessary for the growth of follicles, without which the release of an egg will not be possible. A large amount of estrogen blocks the rise of FSH, but stimulates the rise of LH to cause ovulation.
What drugs restore hormonal levels?
The treatment plan is drawn up by the gynecologist together with the endocrinologist. At the same time, they take into account the reason that led to the hormonal imbalance, as well as secondary factors, these include:
- age;
- nutritional features;
- sexual activity;
- clinical manifestations;
- diseases.
Drugs for restoring hormonal levels can be divided into hormonal and non-hormonal. The former are highly effective, but cause side effects and have contraindications, the latter are more gentle, but such therapy may be delayed.
Phytoestrogens are substances of natural origin; they are one of the key elements in the composition of plants. Their structure resembles human estrogens. Preparations with phytoestrogens are prescribed when hormonal drugs are contraindicated for a woman. The most effective include:
- Remens. Eliminates estrogen deficiency, regulates the psycho-emotional state of a woman, eliminates pain.
- Climaxan. One of the most effective and safe medications during menopausal syndrome, which causes headaches, hot flashes, excessive sweating and irritability.
- Tribestan. The main component of the product is Tribulus plant extract. It contains steroid saponins and improves the functioning of the reproductive system.
- Estrovel. Replenishes estrogen levels in the body, improves psychophysical condition.
Therapy using drugs with sex hormones is considered replacement therapy. As a rule, the specialist prescribes treatment in cycles, which continues until menopause is completely restored. Medicines containing the following hormones show excellent results:
Prolactin
In a woman’s body, prolactin is produced by the anterior lobe of the pituitary gland and is responsible for the lactation process; its target organ is the mammary glands. However, deviations from the norm in prolactin levels during the planning period of a child lead to infertility.
Prolactin inhibits the maturation and release of the egg by suppressing the secretion of FSH and gonadotropic releasing factor (GnRF), reducing the production of estradiol and progesterone. Under such conditions, the processes of egg maturation and the onset of ovulation become impossible.
Forms of anovulatory infertility
The congenital form of pathology occurs as a result of mutation of genetic material. Acquired occurs due to the occurrence of dangerous diseases, these include:
- anorexia;
- Sheen's syndrome;
- disturbance of the psycho-emotional background;
- increased physical activity.
Hyperprolactemia is an independent form. According to statistics, with hormonal infertility, this type accounts for 40% of cases. Increased production of prolactin leads to secondary infertility.
Progesterone
Most progesterone is produced by the ovaries, a small amount is produced by the adrenal glands. After conception, progesterone is produced by the corpus luteum, the placenta. Its main purpose is to prepare the body for pregnancy, but the level of progesterone in the blood also affects the onset or absence of ovulation.
In the first phase of the menstrual cycle, progesterone has the power to both suppress and stimulate ovulation. Its norm on days 1–14 of the cycle is 0.31–2.23 nmol/l. If progesterone levels are below or above reference values, ovulation is suppressed.
When the egg is released, the amount of hormone increases 10 times.
It is recommended to take a test to determine progesterone levels on the 22nd day of the menstrual cycle.
Source: https://MedLazaret.ru/ginekologiya/lechenie-anovulyacii.html
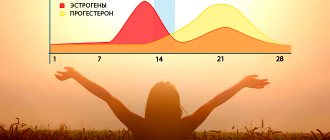
How do hormones work?
In one of the follicles produced by the ovaries, the maturation of the egg occurs. FSH is responsible for this process. Its level increases in the initial phase. With the simultaneous growth of the follicle, the level of estrogen begins to increase. Estrogens, in turn, stimulate the production of LH. It is the growth of this hormone that allows women to track the maturation of the egg. Those women who regularly measure their basal temperature know that an increase of several tenths indicates impending ovulation. It is the luteinizing hormone that leads to a slight jump in temperature. Typically, LH levels rise 48 hours before expected ovulation. This period is considered the most successful for conception.
After the rupture of the follicle, which occurs at the highest level of LH, the egg begins its movement along the fallopian tube, slowly moving directly to the uterus. If fertilization does not occur within 24 hours after the follicle ruptures, then cell death occurs and it is rejected.
A malfunction of the hypothalamus can lead to early or late ovulation, and sometimes to its absence. Delayed or early maturation of the egg may have serious deviations in time from the norm. For example, with a 28-day cycle, the egg may mature not on day 14, but on 8 or 17. Those women who use the calendar method for calculating ovulation may make mistakes when planning conception. But those women who constantly keep a chart of basal temperature will be able to track changes in the period of egg formation.
Hormonal stimulation in IVF protocols: what hormones are used and why
DRA Medical – Treatment in Israel
Hormonal stimulation of the ovaries is one of the stages of preparation for the IVF procedure.
The exception is IVF in a natural cycle, although in this case, as a rule, the use of hormonal drugs is provided - to prepare the endometrium for implantation of the embryo and to maintain normal hormonal levels.
Every month in the natural cycle, 1-2 follicles mature in a woman’s ovaries. This amount is not enough for the IVF procedure, so before the puncture of the oocytes, the woman undergoes a course of hormonal therapy, the purpose of which will be the maturation of several eggs at once.
The more eggs you can get, the higher your chances of pregnancy. It is worth saying that hormonal induction of the ovaries can give rise to a serious side effect - ovarian hyperstimulation syndrome, but we will talk about this below.
In order to understand the principle of action of hormonal stimulation of the ovaries, let us consider how ovulation occurs in natural conditions.
The birth and development of the egg is controlled by two main hormones that are produced in the pituitary gland: luteinizing hormone and follicle-stimulating hormone.
Under the influence of follicle-stimulating hormone in the follicular phase of the menstrual cycle (before ovulation), the ovarian follicle begins to grow and gradually reaches 2 cm in diameter. An egg develops inside the follicle. When the follicle matures, it releases estrogens - hormones that have a systemic effect, primarily on the woman’s reproductive organs.
Under the influence of estrogens, the anterior lobe of the pituitary gland secretes an increased amount of luteinizing hormone (LH), which, reaching its maximum, triggers the “maturation” of the egg. There is approximately 36-48 hours between the ovulatory LH peak and ovulation.
If ovulation has taken place, the corpus luteum of the egg begins to produce the hormone progesterone, which is of great importance for embryo implantation and a successful pregnancy.
Hormonal stimulation before IVF involves artificial hormones and drugs that imitate their functions. For each natural hormone there are several analogue drugs, and in each specific case the use of one or another drug is determined by the decision of the attending physician and the patient’s condition, so there is no point in naming brand names of medications. Before entering into the IVF protocol, a woman undergoes hormone tests; the results of these tests will determine the hormonal therapy regimen and dosage of drugs. The main list of hormones responsible for female reproductive health and involved in the IVF protocol is as follows: TSH (thyroid-stimulating hormone of the thyroid gland), estradiol, progesterone , follicle-stimulating hormone (FSH), luteinizing hormone (LH).
Thyroid-stimulating hormone (TSH)
– this hormone is produced by the thyroid gland and is responsible for the functioning of many systems, including the reproductive one. Deviations from the norm, both larger and smaller, cause various cycle disorders in a woman.
TSH imbalances can manifest themselves in the form of conditions such as amenorrhea (cessation of menstruation), anovulatory cycles (when the egg is not released from the follicle), progesterone deficiency (in the absence of ovulation, the corpus luteum is not produced, and accordingly, progesterone is not produced), primary infertility.
Data on the concentration of TSH in a woman’s blood is also important because this hormone affects the production of other thyroid hormones T3 and T4, which have a direct effect on conception and development of pregnancy. An imbalance of these hormones can lead to severe malformations of the fetus, the threat of termination of pregnancy or its complete impossibility.
That is why, at the planning stage, it is necessary to take a TSH test (and then T3 and T4), so that if hormonal disorders are detected, they can be corrected and further complications can be avoided.
Follicle stimulating hormone (FSH)
- a hormone of the anterior pituitary gland that has a direct effect on the functions of the gonads. FSH is involved in the development of follicles in the female ovaries and is involved in the creation of estrogens.
Its level changes during the menstrual cycle, reaching a maximum before ovulation. Determining the level of FSH in the blood plays an important role in assessing female fertility. FSH is of great importance during IVF, because
Based on its initial indicators, an ovarian stimulation protocol is selected.
Luteinizing hormone (LH)
It is produced by the cells of the pituitary gland, under its action the synthesis of sex hormones occurs: estrogen, progesterone, testosterone.
Reaching the maximum concentration of LH in the blood gives impetus to ovulation and stimulates the development of the corpus luteum, which produces progesterone. During hormonal induction, human chorionic gonadotropin is most often used to initiate egg maturation as a replacement for LH.
If a woman is predisposed to ovarian hyperstimulation syndrome, gonadotropin agonists are used as a “trigger” of ovulation.
Estradiol
– a hormone produced in the ovaries and adrenal glands, which is involved in the development of reproductive organs, as well as the occurrence of pregnancy naturally or as a result of IVF. Estradiol during IVF is responsible for providing the conditions necessary for favorable implantation of the embryo in the uterine cavity.
Based on the concentration of estradiol in the blood, the approximate number of maturing follicles can be determined.
Its level doubles every 48 hours. Progesterone
is a key hormone for all processes associated with pregnancy planning, its course and subsequent breastfeeding. It is not for nothing that it is also called the “pregnancy hormone”.
In non-pregnant women it is produced by the corpus luteum of the follicle, and during pregnancy by the placenta.
The main function of progesterone is to prepare the female body for reproduction: it is responsible for the necessary changes in the uterus associated with preparation for possible conception and gestation, thanks to which the placenta is formed.
During IVF, the level of progesterone in the blood is critically important, since the success of subsequent implantation largely depends on the concentration of this hormone in the blood.
The state of the female reproductive system depends on the balance of the concentration of all these hormones.
A skew in any direction of any component will cause an imbalance in the entire system, which means there will be difficulties with conception and pregnancy.
Therefore, in order to minimize risks, hormonal stimulation temporarily “turns off” the production of some of its hormones and the woman receives again those doses of hormones that will be optimal in her particular case.
The schedule for taking hormonal drugs, scheduled by day and hour, is called an IVF protocol.
There are several protocol options - short, long, ultra-short, ultra-long, French, Japanese, cryoprotocol and others.
Choosing the right protocol is one of the key factors for the success of the entire IVF procedure. This choice depends on the patient’s hormonal status, her health characteristics, and past experience in the field of reproduction.
The principle of operation of all IVF protocols is generally the same and has one goal - the maturation of the optimal number of follicles in the ovaries. The difference will be in the number of days of taking hormonal drugs and their sequence. It goes without saying that the list of these drugs and their doses will also differ. Therefore, there is no point in asking friends what drug regimen was prescribed for them; it will still be different for each patient. These two schemes are most often used. Other protocols are also being developed based on them. The long protocol is indicated for women with average ovarian reserve, endometrial problems, ovarian cysts, and fibroids. It begins on days 21-22 of the previous cycle with the use of drugs that suppress the production of one’s own hormones FSH and LH. This is done to ensure that follicle maturation and ovulation occur at the right time for the doctor, strictly under his control. While taking these drugs, ovarian stimulation begins from day 2-3 of the new cycle, and taking stimulating drugs lasts 10-12 days. Hormonal drugs in IVF protocols stimulate the production of two hormones: FSH and LH. In a normal cycle, non-dominant follicles die before ovulation occurs as FSH levels drop. FSH injections keep it at a high level, so the ovaries produce several eggs at once. When the follicles reach the desired size, a drug is administered, the principle of which is similar to natural LH, to start the process of egg maturation. This drug is administered in such a way that the process of egg maturation is started, and ovulation has not yet occurred, since the collection of eggs must be done before the egg leaves the follicle. After which it becomes possible to successfully puncture the follicle and “get” the egg. The short protocol is more stringent in terms of timing, it is clearly tied to the woman’s menstrual cycle. Stimulating therapy should begin no later than day 2 of the cycle. In the short protocol, ovarian stimulation is carried out over 10 days. Once the follicles reach the desired size, a “trigger” drug is prescribed to trigger ovulation. Most often, this is a large dose of the hormone human chorionic gonadotropin (hCG), which triggers the process of maturation of several follicles at once. The main condition for prescribing hCG is the presence of several follicles of the required size. In addition, the concentration of estradiol must be at a sufficient level. After 35 hours, the follicles are punctured. In place of the punctured follicles, corpus luteum is formed, which produces progesterone, the task of which is to prepare the uterine mucosa for implantation of the embryo. In stimulated cycles, estradiol levels are higher than progesterone levels, so additional doses of progesterone are administered to restore the balance of estrogen and progesterone.
During stimulation, the woman donates blood several times for hormones and does an ultrasound so that the doctor can understand how the body responds to hormonal therapy and whether everything is going according to plan.
The advantage of a long protocol is its manageability and flexibility: stimulating therapy can be started from days 2-6 of the new cycle. You can also shift the date of follicle puncture by 1-2 days, if necessary.
When using a long protocol, doctors achieve the maturation of a larger number of eggs of the same quality and size, but this is its disadvantage - it can lead to ovarian hyperstimulation syndrome, so women prone to this complication are not prescribed a long protocol.
What is ovarian hyperstimulation syndrome
A powerful attack on the female body with large doses of hormones carries a heavy load. Speaking about hormonal stimulation before IVF, one cannot help but mention such a serious complication as ovarian hyperstimulation syndrome. It occurs most often in long IVF protocols in women with a rich ovarian reserve. It is associated with the formation of a large number of follicles - 15 on each side. An increase in the number of follicles increases the concentration of estrogen in the blood, as well as the content of vasomotor substances, which affect the walls of blood vessels throughout the body. As a result, fluid leaks from the vessels and accumulates in the abdominal cavity and pericardium. A lack of fluid in the vascular bed disrupts the activity of the brain, kidneys and other vital organs. This is a serious complication, and the attending physician must consider all possible risks when choosing a stimulation protocol.
The advantage of the short protocol is the possibility of prescribing a gonadotropin agonist drug (not hCG) as a “trigger” to reduce the risk of developing ovarian hyperstimulation syndrome to zero. The use of these drugs, however, also reduces the chances of pregnancy. In such cases, segmented protocols are used, when stimulation is performed in one cycle and embryo transfer in the next.
Each protocol has its pros and cons; if one does not work in one cycle, the next time the doctor may suggest a different regimen and the body’s response may change dramatically. In general, they all pursue the same goals and are approximately equal in efficiency and cost.
Source: https://www.dramedical.ru/eko/gormonalnaya-stimulyatsiya-ovuljatsii