Uterine fibroids are benign nodular formations in the myometrium (the muscular wall of the uterus).
The tumor is one of the most common gynecological diseases and is most often found in women of late reproductive age, before menopause. The frequency of the disease is approximately 25% of all gynecological pathologies.
At CELT you can get advice from a gynecologist.
- Cost of initial consultation - 2,700
- Cost of consultation with ultrasound - 4,200
Make an appointment
Myomectomy
- Cost: 120,000 - 170,000 rubles.
- Duration: For laparoscopy and laparotomy - 60-90 minutes, for hysteroscopy - 20-40 minutes
- Hospitalization: 1-3 days in hospital
More details
Causes
Experts around the world cannot name the cause of the pathology with 100% accuracy. Damage to ovarian tissue can affect the growth of the tumor. This impairs their basic function, which leads to increased production of female sex hormones. Studies have shown that estrogens promote tumor growth. As soon as women stopped taking oral contraceptives, the growth of fibroids stopped, and subsequently it completely resolved. But this is not the exact cause, since uterine fibroids can develop in the absence of endocrine disorders. Among other reasons, experts identify:
- Genetic predisposition.
- Lack of pregnancy until 30-35 years of age.
- Diseases of the immune and endocrine system.
- Endometriosis.
- Inflammation of the ovaries and fallopian tubes.
- Abortion.
- Difficult birth.
- Polycystic ovary syndrome.
How to determine the size of fibroids
Myoma is a benign tumor that forms in a woman’s reproductive organ. Girls aged 20 years and older experience the disease, but the risk of developing it increases after menopause. The main reason for the development of the disease is changes in hormonal levels, therefore, crisis periods are defined as:
- pregnancy;
- postpartum period;
- breastfeeding period;
- menopause.
At the initial stage, when uterine fibroids are small in size, the disease does not manifest itself. A characteristic clinical picture can be seen as the formation grows; the woman experiences bleeding that has no connection with menstrual bleeding, and pain in the lower abdomen. The size of the uterus is compared with the size of the fetus during pregnancy; a similar conclusion can be obtained after an ultrasound scan.
Attention! The size of a benign neoplasm is determined in centimeters and then compared with the obstetric gestational age.
There are 3 types of fibroids, depending on their size:
- Small - no more than 2 cm, determined for a period of 4-6 obstetric weeks. Removal is carried out if there is a risk of bleeding and if the woman develops anemia. Also, the neoplasm requires surgical intervention if it causes infertility.
- Average - up to 6 cm in diameter, which corresponds to 11 weeks of pregnancy. The tumor is monitored and removed if it continues to grow. When placed on the outer wall, it may put pressure on the abdominal organs. If malfunctions occur in their work, they resort to surgical intervention.
- Large (large) - more than 6 cm in diameter, which corresponds to the 12th week of pregnancy. The tumor puts pressure on nearby organs and therefore undergoes surgical removal. The woman is prescribed long-term drug treatment after the intervention.
A small tumor is not dangerous. There are no disturbing symptoms; it can be detected by an attentive gynecologist during a routine examination or during an ultrasound.
Characteristics of small fibroid tumors
A small fibroid is a tumor whose size does not exceed 2 cm in diameter. As it grows, the uterus enlarges and corresponds to the 5th week of pregnancy. The main characteristic feature of the neoplasm is a dense myomatous node. Which is represented as a growth center. Bimanual examination reveals a dense core, which persists even in the absence of blood supply to the reproductive organ. At the initial stage of growth, a peripheral growing volume is localized along the edges of the neoplasm. The tumor is considered small until it acquires its own growth mechanism.
There is no clinical picture at this stage; the woman may notice minor changes:
- increased volume of menstrual blood loss;
- cycle reduction;
- severe pain accompanying menstruation;
- bloody discharge outside the menstrual cycle;
- discomfort in the lower abdomen.
The prognosis for the patient with timely detection of the tumor is favorable.
Features during menopause
Postmenopausal fibroids may appear on their own and disappear after some time. Sometimes fibroids not only do not resolve, but also grow rapidly.
The danger of a tumor during the menopausal period is that the symptoms appear unexpressed, until the tumor reaches gigantic proportions. It is necessary to pay attention to this feature: fibroids rarely progress during menopause due to a lack of hormones. The rudiments of its development are laid immediately before the onset of menopause and symptoms include:
- heavy menstrual flow;
- dysmenorrhea;
- bleeding between periods;
- nagging pain in the lower abdomen and lower back;
- increase in abdominal size;
- difficulty urinating;
- constipation;
- anemia;
- weakness;
- dizziness;
- darkening of the eyes.
The presence of any of the listed symptoms indicates the need for an unscheduled visit to a gynecologist. It is not always possible to identify small fibroids with a two-handed examination, but ultrasound will give an accurate answer.
Attention! The treatment regimen, regardless of the patient’s age, is determined individually. Treatment is provided on an outpatient basis.
Diseases during menopause do not pose a threat to women, because reproductive function has already been lost. The main risk is that due to insufficient production of estrogen, the tumor can degenerate into malignant.
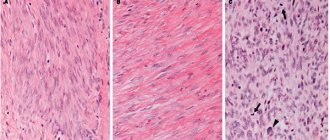
The statistics on gynecological oncology are frightening; uterine cancer is the leading cause of death among women over the age of 60. The development of the oncological process can be announced after histological examination. Atypical cells are formed in the tumor tissues, representing foci of increased growth. Against this background, the rate of cell division is activated.
Small fibroids during menopause are not a reason for surgical intervention if there is no tendency to proliferate. The growth of the tumor is controlled, and the woman should regularly visit the gynecologist. Therapy consists of oral progestogen and progesterone. Medication helps to reduce the size of fibroids and relieves the patient of bothersome symptoms.
Self-resorption
The development of fibroids is provoked by hormones, because the tumor is hormone dependent. With an excess of estrogen and a lack of progesterone, noticeable progress in formation can be observed. The ability to self-resorb during menopause is associated with these fluctuations, but the outlook for women of reproductive age looks different. The tumor may disappear if it is mobile; there is no chance of eliminating ingrown nodes without medical intervention.
For some time, a popular theory was based on the fact that a woman with a small fibroid needs to get pregnant. During pregnancy, hormonal levels change and the fibroids resolve. Doctors deny this possibility. It is better to correct hormonal levels with medications. Pregnancy with a small fibroid is dangerous for both the mother and the fetus, and certainly not a means to get rid of a benign tumor.
Symptoms of the disease
Symptoms of uterine fibroids are varied and depend on the location of the fibroids, size and individual characteristics of the body. The most typical manifestations are:
- for submucosal (submucosal) fibroids - heavy and prolonged menstruation; metrorrhagia - uterine bleeding leading to anemia; pain resembling contractions;
- for intermuscular fibroids - often asymptomatic at first, and with increasing size - lengthening and increasing pain of menstruation; bleeding; with significant growth - compression of the organs adjacent to the uterus, resulting, for example, in an increased urge to urinate, sometimes - the development of inflammatory diseases; if the nodes are located on the back wall of the uterus - difficulty defecating and constipation;
- for subperitoneal (subserous) fibroids - disturbances in the menstrual cycle; pain in the lower abdomen; increased temperature and severe pain due to poor nutrition (blood supply) of the myomatous node; with growth - compression of internal organs with difficulty urinating and defecating.
Nonspecific symptoms accompanying uterine fibroids in some cases are infertility, inability to bear a child. They are not always signs of a tumor, but often are its consequence with a pronounced increase in nodes.
Deciphering the results
Ultrasound parameters:
- What shape is the uterus;
- Its dimensions;
- Thickness of the endometrial layer;
- Heterogeneous myometrium or what structure does it have?;
- Myoma signs or polyps will be revealed. Possibly a tumor + polyp, several.
What size is the organ, shape, where is it located?
If the uterine space is normal, then on ultrasound the organ will be pear-shaped. For women of childbearing age, it has the following parameters:
- From 45 to 67 mm length;
- From 46 to 64 mm width;
- From 30 to 40 mm thickness.
When menopause occurs, the uterus will become significantly smaller. How enlarged the uterus is is noted in weeks, which correspond to the weeks of pregnancy. If fibroid proliferation occurs, the uterus will become as large as from 14 to 17 weeks. Such fibroids are visible on ultrasound.
If the uterus is normally located, then it is tilted forward. The bottom is located forward and slightly upward. The vaginal area goes back and then down. There is an obtuse angle between the neck and the body. This position during ultrasound examination is called anteversio/anteflexio.
If the location is described as retroversio/retroflexio or lateroversio/lateroflexio, this means that the bend goes to the posterior pelvic wall or to the lateral one. You can determine uterine fibroids:
Uterine fibroids: diagnosis
First of all, it is necessary, of course, to consult a gynecologist for an examination. The simplest and most informative (up to 95% accuracy) test for the presence/absence of a tumor is ultrasound. During the study, fibroids manifest themselves as rounded lesions with reduced echogenicity. The exact location of the nodes can be obtained using a 3D study.
To differentiate myomatous nodes and ovarian tumors, MRI is prescribed if necessary. To diagnose small submucosal nodes, hysteroscopy is used - a minimally invasive endoscopic examination of the uterine cavity with a hysteroscope.
Pregnancy with fibroids
With small fibroids up to 2 cm in diameter, pregnancy may occur, but there are some risks. There are many cases where pregnancy failure occurred in the early stages due to a tumor in the cavity of the reproductive organ.
If pregnancy occurs in a woman with fibroids, she will have to visit the gynecologist much more often and get tested. It is precisely because of this particularity of the disease that it is recommended to get rid of myomatous nodes even before conception, which increases the chance of giving birth to a healthy child.
Video: why are uterine fibroids dangerous? Subserous, nodular and interstitial.
Why are uterine fibroids dangerous? Subserous, nodular and interstitial.
Video: uterine fibroids and motherhood
Health. Uterine fibroids and motherhood. (27.11.2016)
Treatment of uterine fibroids
Uterine artery embolization
- Cost: 72,000 rub.
- Duration: from 15 to 50 minutes
- Hospitalization: 1 day in hospital
More details
Treatment of uterine fibroids involves several options - expectant management, conservative treatment, surgical intervention.
Watchful waiting, although still highly controversial, is quite common if the nodes detected are small. The patient is prescribed dynamic observation by a doctor, ultrasound control at least once a year. If the nodes do not grow or decrease over time, and no new symptoms of the disease arise, then this tactic is maintained for a long time. During observation, the woman receives recommendations for preventing the growth of myomatous nodes - avoiding intense thermal procedures (solarium, sun tanning, saunas), hardware cosmetic procedures, and normalizing nutrition.
In conservative treatment of uterine fibroids, the goal is inhibition, complete cessation of the growth of the myomatous node and its reduction. For this, hormonal drugs are used (capable of reducing the volume of nodes by half or more), tranexamic acid, and other drugs. Non-surgical methods of treating uterine fibroids also include uterine artery embolization (UAE), in which the blood supply to the node is stopped and, as a result, the node decreases in size. You can read more about this treatment method and about uterine fibroids on our website in the article “Stop Fibroids.”
Surgical intervention for symptomatic uterine fibroids can be of two types.
Conservative (organ-preserving) myomectomy is performed during reproductive age to remove only the nodes, while preserving the uterus for the possibility of bearing a child. Myomectomy can be performed endoscopically (in particular, after previously performed embolization of the uterine arteries) - during hysteroscopy (or hysteroresectoscopy), laparoscopy or laparotomy.
Radical surgery - total/subtotal hysterectomy involves removal of the uterus with or without appendages. The indication for radical treatment is a large tumor, multiple fibroids, and the patient is perimenopausal (over 45 years old).
Prognosis and prevention
If pathology is detected at an early stage and treated conservatively, then further complications are excluded. If a safe surgical operation is prescribed while preserving the integrity of the organ, it is possible to preserve reproductive function. But this applies only to the initial stages of pathology. If the fibroid grows strongly and the patient’s condition worsens, then complete removal of the uterus is required, even at a young age. This is why you need to visit a specialist twice a year for diagnosis, as the disease can lead to infertility.
To avoid relapse after surgery, you need to take hormonal medications. Regular visits to a specialist and MRI and ultrasound are recommended in order to detect tumor formation at an early stage. It is important to avoid severe disruptions in the hormonal system and mechanical damage to the vagina and uterus. The specialist must select the optimal method of contraception to avoid abortion or complicated childbirth. People over 35 years of age should not sunbathe for a long time if surgical treatment of the pathology has been performed.
The multidisciplinary CELT clinic employs experienced specialists.
After a comprehensive examination, the gynecologist will choose the optimal treatment method or (most often) a sequential combination of methods, i.e. will develop an individual treatment program for uterine fibroids. Our doctors try in most cases to resort to organ-preserving laparoscopic operations, which are the least traumatic and allow you to preserve the uterus and ovaries and have children in the future. We answer the most popular questions from patients about uterine fibroids on our website.
Our services
The administration of CELT JSC regularly updates the price list posted on the clinic’s website. However, in order to avoid possible misunderstandings, we ask you to clarify the cost of services by phone: +7
| Service name | Price in rubles |
| Preoperative hysteroscopy | 35 000 |
| Embolization of the uterine arteries without taking into account the cost of embolic agents and consumable instruments (radial access) | 86 000 |
| Endoscopic conservative myomectomy | 100 000 — 145 000 |
All services
Make an appointment through the application or by calling +7 +7 We work every day:
- Monday—Friday: 8.00—20.00
- Saturday: 8.00–18.00
- Sunday is a day off
The nearest metro and MCC stations to the clinic:
- Highway of Enthusiasts or Perovo
- Partisan
- Enthusiast Highway
Driving directions