In recent years, cervical cancer (CC) has occupied a leading position among the problems of oncology and gynecology; high morbidity and mortality rates remain, despite increased interest in the problem and numerous studies in this area [1–3]. The absence in our country of primary mass prevention of cervical cancer through vaccination, the increase in infection with highly oncogenic strains of the human papillomavirus (HPV) among the world's population [4-7], the high frequency of background diseases of the cervix, which contribute to the process of carcinogenesis [8-10], are of particular importance development of methods of secondary prevention. The main directions in this area are the study of risk factors for tumor transformation with a view to their timely correction, improvement of screening methods and development of new management algorithms aimed at increasing the effectiveness of therapy and preventing relapses of cervical dysplasia [11-14]. A special place is occupied by the issue of rehabilitation of reproductive health disorders in patients treated for dysplasia, taking into account the main increase in the incidence of cervical cancer among patients of active reproductive age [15-17].
The trigger mechanism for carcinogenesis is the long-term persistence of papillomaviruses in the cells of the endocervix and exocervix with the development of immune failure and structural changes at the cellular and tissue levels, leading to the emergence of pre-invasive pathology [5, 18, 19]. However, the fact of infection itself is not the only reason necessary for the occurrence of a tumor [20–22]. In the majority of infected women, especially at a young age, with the correct management tactics, it is possible to achieve elimination of the pathogen before the development of the dysplastic process [14, 23, 24]. Timely diagnosis and adequate treatment of background pathology of the cervix, identification and correction of risk factors can prevent the development of cervical dysplasia and subsequent carcinogenesis. Complex treatment tactics using modern highly effective organ-saving therapy techniques provide the possibility of cure in almost 98% of patients with preinvasive processes and carcinoma in situ
[8, 15, 25]. However, the emerging trends in the treatment of patients with CIN are mainly aimed at removing the pathological focus, which leads to excessive, in some cases unjustified, surgical aggression with the development of complications, including anatomical incompetence of the cervix, miscarriage and complicated labor [24, 26]. Conventional treatment methods often do not provide for the stimulation of a systemic antiviral effect and the rehabilitation stage after excisional surgery, which can lead to relapse of the disease [14, 27, 28].
According to the literature [16, 20, 29], predisposing factors for relapse of CIN II-III after surgical organ-preserving treatment include: re-infection with HPV in the early postoperative period or the presence of a positive polymerase chain reaction test (PCR test) after excision (virus - positive resection margin), disruption of methylation processes in adjacent tissues, especially in combination with active or passive smoking, as well as the presence of a cone of dysplastic cells at the resection margin, regardless of the degree of their changes.
From the data obtained it follows that removal of the pathological focus is necessary, but not sufficient to stop carcinogenesis and prevent relapse.
The purpose of the study was to improve the algorithm for the management of patients with recurrent severe dysplasia of the cervical epithelium.
Conization in cervical dysplasia
Conization of the cervix is an operation that involves a cone-shaped excision of the mucous epithelium of the cervical canal.
The procedure got its name from the shape of the segment being removed. Conization of the cervix for grade 3 dysplasia is one of the effective treatment options for the pathology. The disease is considered quite dangerous, as it has a high risk of malignancy. With cervical dysplasia, atypical cells grow in the area where the squamous epithelium combines with the cylindrical epithelium.
Conization for cervical dysplasia has the main goal: removing atypical cells from the cervical canal and stopping the pathological process. The procedure not only stops cell division, but also determines the initial stages of cancer.
Diagnosis of the remote site is carried out for all women who have undergone conization. The tissues are subjected to histological examination, the results of which can confirm or refute invasive cancer.
Identifying a dangerous disease in the early stages allows you to receive effective and timely treatment. Surgery is performed not only for grade 3 dysplasia. Indications for its implementation will be various disorders in the epithelial layer: erosion, scarring, deformation, cervical ectropion, as well as grade 2 and 4 dysplasia.
What is the difference between erosion and cervical dysplasia
Erosion is a chronic inflammation of the cervix. In modern gynecology, a distinction is made between true erosion and pseudo-erosion. The true one appears quite rarely. The prerequisites for its development are created against the background of serious neck injuries during surgical interventions. A bleeding wound forms on the surface. Pseudo-erosion of the cervix or ectopia is diagnosed by identifying atypical cells, the inner layer lining the uterus to the outside.
Cervical dysplasia is much more dangerous. This condition is classified as precancerous. Against the background of the process, changes appear in the structure of the cells of the mucous membrane lining the uterus. Thickening and proliferation of tissues occurs and their functional purpose is disrupted.
Considering the difference between the two gynecological conditions, it is worth noting that erosion affects only the superficial epithelial layers, unlike dysplasia. With dysplasia, the pathological process extends to all 3 layers. The main danger of both diseases manifests itself when they are not detected in a timely manner, therefore women aged 25 to 35 years old must undergo an examination by a gynecologist once a year. Not only a visual examination is necessary, but also an extended colposcopy, because it is impossible to detect atypical cells with the naked eye.
Symptoms of pathological conditions are presented in the table.
| Clinical picture characteristic of cervical erosion and dysplasia | |
| Erosion | Dysplasia |
| It often occurs in a latent form, making diagnosis difficult. Bloody discharge may occur after sexual intercourse, douching, or a gynecological examination. When a bacterial infection occurs, itching and burning of the genitals occurs, and copious vaginal discharge with an unpleasant odor appears. |
Attention! You should not try to determine the diagnosis and prescribe treatment on your own. Delay in the case of dysplasia is dangerous. In the absence of treatment, mild dysplasia develops into severe dysplasia, and then into squamous cell carcinoma.
Erosion, like dysplasia, is an independent nosological entity. There is only one connection between these diseases: a dangerous precancerous condition develops at the last stage of erosion. In this case, there is a risk of rapid formation of a malignant tumor.
Contraindications
If a woman has cervical dysplasia, conization is not always carried out. This type of treatment is contraindicated in patients with confirmed cancer. In this case, the entire organ is usually removed, after which long-term treatment is prescribed, including chemotherapy and radiation.
It is forbidden to perform conization if a woman has an inflammatory process in the vagina. It is necessary to first undergo treatment, and then carry out the chosen method of surgical intervention. Conization is contraindicated for patients during pregnancy, as this may cause its termination. Before conization is performed, preparation and examination are required.
The procedure for cauterization of dysplasia in nulliparous girls
Electrocoagulation is rarely used to treat dysplasia in nulliparous women. This is due to the fact that after the procedure, a noticeable, rough scar forms on the surface of the woman’s cervix, which can interfere with conception and complicate the process of bearing a pregnancy. Doctors always try to preserve a woman’s reproductive function, so they refuse such a procedure so as not to provoke infertility.
The most commonly used method is radio wave and laser cauterization. Such therapeutic manipulations make it possible to cure dysplasia in nulliparous girls without reproductive dysfunction.
Preparation
Cervical dysplasia is often asymptomatic. The disease develops over a long period of time, moving from one stage to another. The presence of cells unusual for a particular area of the cervix can be determined during a gynecological examination. However, a diagnosis cannot be made with certainty. To verify dysplasia, a colposcopy is performed.
Colposcopy is a detailed study of the mucous layer of the cervix using a magnifying device and reagents. Diagnostics allows you to examine pathological areas and take tissue for further study - do a biopsy. Colposcopy is a mandatory examination before conization.
If the results of colposcopy show that the cervix does not have malignant neoplasms, then further preparation for surgery is carried out:
- vaginal smear - determines the degree of cleanliness and helps ensure the absence of infectious processes;
- blood tests - the list of basic ones includes general examination, biochemistry, TORCH infections, as well as determination of group and rhesus;
- coagulogram – establishes the rate of blood clotting, which is important for preventing bleeding;
- urine analysis – allows you to assess the functionality of the urinary system, and also gives an indirect assessment of the body’s functioning;
- PCR diagnostics is necessary to determine HPV in the body, which often becomes a provocateur of the disease.
In order for the recovery period to go as smoothly and easily as possible, conization must be done in the first days of the menstrual cycle, immediately after the end of bleeding. Treatment is usually prescribed on days 5-7, but can also be carried out on days 10. The need to perform the procedure in the first phase of the cycle is determined by the patient’s hormonal background.
Immediately after the end of monthly bleeding, estrogen production begins. These hormones help the mucous membrane to recover. Therefore, when conization is performed in the first phase, the risk of complications is minimized.
Grade 3 dysplasia can be found in postmenopausal patients. If a woman does not have a menstrual cycle, then the operation is performed on any day.
Results and discussion
Analysis of risk factors for recurrence of dysplastic processes in the cervix in patients showed that 17 (27.4%) patients in the 1st main group and 16 (26.7%) in the 1st control group did not use contraception. The frequency of use of various methods of contraception in the main and control groups did not differ.
Destructive treatment methods in the anamnesis before verification of the diagnosis of CIN were noted equally often in women with recurrent CIN and in the control group: in 56 (90.3%) and 53 (88.3%) patients, respectively, including repeated ones in 35 (56 .5%) and 25 (41.7%) patients of the main and control groups ( p
>0.05). In the structure of methods of destruction in patients of both groups, diathermocoagulation predominated (48.3 and 45%); less often - cryotherapy (29 and 25%) and radio wave therapy (RWT) (23.2 and 20%).
Anatomical changes in the cervix were noted in 27 (43.5%) women with recurrent CIN. In 14 (22.6%) patients, cicatricial deformation and hypertrophy of the cervix were noted, in 7 (11.3%) - isthmic-cervical insufficiency (ICI), in 6 (9.7%) severe hypertrophy of the organ was caused by multiple retention cysts . Displacement of the transformation zone into the cervical canal, which complicates colposcopic and cytological examinations, was noted in the majority of patients who suffered destructive effects on the cervix (42 women, or 68%). In the control group, anatomical changes in the cervix were diagnosed somewhat less frequently - in 30 (50%) women ( p
>0,05).
Diagnosis of CIN II-III centuries. In the 1st main group, it was initially established on the basis of a targeted biopsy in 46 (74.5%) patients, excisional diagnostic intervention was performed in 16 (25.8%). Curettage of the cervical canal at the examination stage was performed in 23 (37.1%) women. During subsequent therapeutic excision, additional foci of severe dysplasia in the removed conus were identified in 14 (22.6%) patients, undiagnosed CIN in the cervical canal - in 3 (4.8%), which confirms the data [10] on the underdiagnosis of severe lesions of the cervical epithelium when performing point biopsies.
Combined pathology of the vagina and vulva was noted in 52 (83.8%) patients of the main group. In the control group, the same indicator was significantly lower and amounted to 32 (53.3%) observations ( p
≤0.05).
In the structure of vulvovaginal pathology during recurrent dysplasia, bacterial vaginosis predominated in 37 (59.6%) patients, chronic vaginitis was diagnosed in 15 (24.2%), anogenital condylomas - in 18 (29%). Prolapse of the vaginal walls, accompanied by an increase in pH more than 4.5 (53.3%; p
≤0.001), was noted in 16 (25.8%) women of the main group, which was significantly more often than in the control group - 6 (10%) (
p
≤0.05).
Smoking patients made up the majority of the main group - 43 (69.4%), in the control group there were significantly fewer of them - 21 (35%) ( p
≤0,001).
Excess body weight and prolapse of the vaginal walls were observed significantly more often in the main group than in the control group, amounting to 37.1% versus 20%, respectively ( p
≤0.05) and 25.8% versus 10% (
p
≤0.05).
37 (59.7%) patients in the main group and 12 (20%) in the control group had more than 3 sexual partners ( p
≤0.001).
Localization of dysplasia on the exocervix was observed in the majority of patients in the control group - 50 (83.3%), while in the group with recurrent CIN, endocervical localization and a combination of endo- and exocervical location of CIN were significantly more often observed - 24 (38.8%) versus 10 (16.6%) in the control group ( p
≤0,01).
Combined gynecological pathology was noted in 41 (66.1%) women in the main group and in 35 (58.3%) in the control group ( p
>0.05). The structure of the pathology was dominated by chronic inflammatory processes in the pelvic organs (51.6%) and hyperplastic processes in the reproductive organs: uterine fibroids (25.8%), hyperplastic processes in the endometrium (17.1%), endometriosis (19.5% ). Menstrual dysfunction was noted in 31.7% of women in the 1st main group. It should be noted that 3 (4.8%) of the examined patients with recurrent CIN III were diagnosed with concomitant atypical endometrial hyperplasia. Combined pathology of the mammary glands was diagnosed in 29 (46.7%) patients of the 1st main group. In the structure of the pathology, focal formations (cysts, fibromas) amounted to 17.7 and 24.1%, respectively, diffuse formations (fibrous and fibrocystic mastopathy) - 28.4%. There were no differences in the structure of pathology of the reproductive system organs in the main and control groups.
Clinical and laboratory signs of hyperandrogenism were detected in 13 (20.9%) patients of the main group and 9 (15%) of the control group.
Among women in the main group, during primary treatment, only surgical destruction of the pathological focus (knife surgery, radio wave surgery, diathermocoagulation) was used in 30 (48.4%), a combination of destruction with stimulation of antiviral immunity - in 32 (51.6%), additional treatment methods at the rehabilitation stage - in 16 (25.8%) patients, photodynamic therapy - in 1 (1.6%), hormonal treatment for concomitant pathology was prescribed to 12 (19.3%) women. In the control group, stimulation of antiviral immunity after excision was carried out more often: in 42 (70%) women ( p
<0.05), including photodynamic therapy - in 26 (43.3%) (
p
<0.001), targeted drugs were prescribed in 28 (46.7%) (
p
<0.05), correction for identified combined hormonal disorders (polyps, menstrual dysfunction, hyperandrogenism) - in 16 (26.7%;
p
>0.05) women.
Combined pathology of the vagina and vulva was more often diagnosed in the study group compared to the control group - 52 (83.8%) and 32 (53.3%), respectively ( p
≤0,01).
A positive PCR test 8 weeks after excision was observed in 20 (32.3%) patients of the main group and only in 5 (8.3%) of the control group ( p
≤0.001). Examination and treatment of the sexual partner in 49 (70.9%) patients of the main group was not carried out.
Thus, the risk factors for recurrence of CIN II-III are: the presence of a large number of sexual partners and the lack of treatment for them, smoking, disturbance of the vaginal microbiocenosis, repeated destructive effects due to underlying diseases of the cervix, leading to deformation of the organ, endocervical localization of the dysplastic process, the presence of concomitant pathologies of the organs of the reproductive system, repeated surgical interventions due to an inadequate diagnostic volume of the primary biopsy, limitation of treatment to destruction of the pathological focus, the presence of an HPV-positive resection margin after excision.
The results obtained confirm the literature data on the influence of smoking, a large number of sexual partners and alkalization of the vaginal environment on the processes of carcinogenesis [1, 7, 25, 28], as well as on similar processes in the pathogenesis of hyperplastic and dysplastic processes in the organs of the reproductive system [2].
The time of relapse ranged from 6 months to 6 years. In 27 (43.6%) patients of the main group, relapse was diagnosed during the 1st year of observation, in 20 (32.3%) - during the first 3 years, in 15 (24.2%) - more than 3 years after treatment.
An assessment of the complex treatment regimen carried out in patients with recurrent severe dysplasia showed that with the preoperative use of a complex domestic drug containing interferon alpha-2b, fluconazole, metronidazole and boric acid, in the form of suppositories, the preparation time for excision was in 87.5% of patients less than 20 days, including 40.3% less than 10 days, 46.8% from 10 to 20 days. Only 8 (12.9%) women required more than 20 days for vaginal sanitation. Thus, essentially pre-excision preparation was completed within one menstrual cycle, allowing LEEP or LLETZ to be performed in the first week after menstruation; this is the prevention of bleeding and post-excision endometriosis of the cervix.
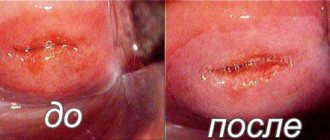
Correction of the vaginal microbiome at the preoperative stage in combination with the use of radio wave excision techniques had a beneficial effect on subsequent repair of cervical tissue. Epithelization periods of less than 4 weeks were observed in 21 (33.8%) patients, in 29 (46.8%) women healing was completed within 4 to 6 weeks, complete epithelization of the excision zone within 6-8 weeks was noted in 12 (19 .4%) women.
Vaginal pH 6 months after treatment remained below 4.5 in 31 (96.7%) of those examined in the 2nd main group. According to the FEMOFLOR test, moderate and severe vaginal dysbiosis in the 2nd main group was diagnosed somewhat less frequently than in the 2nd control group (9.3% versus 23.3% and 6.2% versus 13.3%, respectively). A decrease in the amount of lactoflora and vaginal candidiasis in the 2nd control group were diagnosed after completion of therapy somewhat more often compared to these indicators in the 2nd main group (10.8% versus 5.8% and 18.1% versus 9.8%, respectively ; R
>0,05).
After completion of the course of therapy and rehabilitation, there was a decrease in the number of smoking patients and those with excess body weight compared to the initial data in the 2nd main group: from 22 (69.4%) to 12 (38.7%) and from 11 (34. 3%) to 8 (25%) respectively. In our opinion, the patient’s conscious participation in the treatment process is an important component of therapy, helping to increase motivation for treatment and increase its effectiveness.
In patients of the 2nd main group after treatment, colposcopic pictures corresponding to the norm were noted more often than in the 2nd control group (93.7% versus 70%; p
≤0.05), abnormal HSIL type - only in the control group - 1 (3.3%) observation, signs of inflammation were somewhat more common in the control group - 20 (6.2%) (
p
>0.05).
A normal cytogram was more often recorded in the main group compared to the control group (81.3 and 53.3%; p
≤0.05), koilocytes and ASCUS type cells were slightly more often observed in the control group (16.7 versus 6.3% and 13 .3% versus 3.1%, respectively).
A positive test for HPV of high carcinogenic risk after therapy was observed in 6 (19.2%) patients of the 2nd main group (before treatment, the test was positive in 96.8%). In 50% of them, virus reactivation was noted during the first 1.5 years of observation, the other 50% - later.
Recurrence of dysplasia after treatment was diagnosed in 5 (15.6%) patients of the 2nd main group, including CIN I - in 2 (6.2%), CIN II - in 1 (3.1%), CIN III - in 2 (6.2%). Recurrence of CIN III in both cases was noted when localized in the cervical canal. There was no progression of the process.
In the control group, recurrence was noted in 6 (20%) cases. Recurrence of CIN III was detected in 3 (10%) patients, including 2 with CIN localized in the cervical canal. Progression of the process was noted in 1 (3.3%) patient. All of them underwent radical surgery - hysterectomy with appendages. CIN II was detected in 2 (6.6%) patients 1.5 years after treatment.
Positive dynamics of the condition of the mammary glands clinically and according to ultrasound data after treatment was found in 20 (63.2%) patients of the 2nd main group.
Combined endometrial hyperplasia was detected at the stage of inclusion in the study in 17.1% of patients of the 2nd main group; after treatment, a control endometrial biopsy did not reveal any pathology.
Thirteen patients were determined to achieve reproductive function after therapy. Pregnancy occurred within 3 years in 9 (69.2%) of them and ended in childbirth in 4 women, early spontaneous abortion in 3, and pregnancy continued in 2. In the control group, among 12 women who were determined to bear children, pregnancy occurred in 6, and within the first year after treatment in 2 patients. Both of these patients resorted to early medical abortion. In 1 patient, pregnancy ended with timely surgical delivery, in 1 - premature birth at 25 weeks, and in 2 there was a spontaneous miscarriage at up to 12 weeks.
Thus, carrying out staged complex therapy in patients with recurrent cervical dysplasia, including lifestyle correction, pre- and post-excision normalization of the vaginal microbiome, stimulation of repair and antiviral immunity, administration of hormonal and additional therapy, made it possible to increase the effectiveness of treatment, prevent the progression of CIN, and preserve reproductive function of patients.
Methodology
Conization of the mucous layer of the cervix can be performed in different ways:
- knife involves surgical cutting out pathological areas;
- laser is carried out using a laser beam and is more gentle;
- Electroconization involves the use of a radio wave device.
The method of cervical treatment is selected according to the individual characteristics of the patient. The realization of the reproductive function is of no small importance.
If the patient wishes to have children in the future, preference is given to the most gentle method. Based on the volume of surgical intervention, one can distinguish economical conization, in which the removed area is no more than one and a half centimeters, and high conization, in which 2/3 of the cervical canal is excised.
Knife
About 40 years ago this technique was the only one. Removal of pathological areas was carried out with a conventional scalpel. The procedure is quite painful, despite the absence of nerve endings on the cervical mucosa, so it is performed under general anesthesia.
Currently, the knife method remains the preferred method for patients with confirmed cancer. The main advantage of this procedure is that it allows one to obtain more complete material for histological examination than modern conization methods.
Disadvantages of knife therapy include: a high risk of complications, the likelihood of bleeding, the possibility of infection, the formation of large scar areas and loss of cervical functionality.
Laser
This technique is considered more preferable than a radical method of treatment. Laser conization is carried out by treating the cervix with a special beam. The operation is performed without bleeding and is practically painless. However, not all medical institutions can do it.
Statistics data: pathological outcome
The prognosis for the patient depends on the stage of detection of the pathology, as well as on the timeliness of the treatment. With mild damage, the probability of spontaneous recovery of the mucous membranes is quite high and is about 50%. The risk of developing cervical cancer does not exceed 1%, so there is no need to panic.
If a lesion is detected early, a wait-and-see approach is adopted. Doctors are monitoring the woman's condition. Colposcopy is indicated at intervals of 1-2 times every 6 months. If progress is detected, the lesion is removed.
If moderate dysplasia is detected, there is no point in postponing treatment, because there is a risk of the disease progressing to the 3rd (advanced) stage. Severe dysplasia, in the absence of therapy, will certainly transform into cancer and require treatment according to a different protocol.
It is worth paying attention to the following statistics:
- a latent course is observed in 10% of patients, so regular gynecological examinations should not be abandoned;
- per 1000 patients aged 25 to 35 years, there are 1.5 cases of detection of cervical dysplasia;
- relapse of the disease when treated at stages 2-3 is 10%;
- with timely detection, complete recovery is observed in 98% of cases;
- In 50% of cases, untreated dysplasia transforms into cancer and ends in death.
Attention! The main danger of cervical dysplasia is squamous cell carcinoma. It progresses rapidly and is asymptomatic. That is why gynecologists do not recommend ignoring such a serious pathology.
Why the disease is so widespread in Russia is difficult to say. Most likely, the reason lies in the negligent attitude of women of childbearing age towards their own health. Mild symptoms are often ignored, and the need to visit a doctor is considered only after the pathology has reached a late stage.
Rehabilitation
As a result of electroconization of the cervix for dysplasia, the postoperative period will be the shortest and will be no more than a month. With the radical knife method, the healing time of the mucous membrane can increase by 3-6 times.
Immediately after the operation, the patient remains under medical supervision for at least two hours. If there are no complications, she is discharged for further outpatient treatment. It is important to follow the recommendations throughout the recovery period:
- exclude intimate relationships;
- do not take a bath or swim in public bodies of water;
- exclude thermal procedures, do not sunbathe and do not visit the bathhouse;
- stop using tampons and vaginal products;
- douche and use vaginal suppositories only as prescribed by a doctor;
- Minimize physical activity, do not lift more than 3 kg.
2 weeks after the treatment, it is recommended to see a gynecologist to assess the quality of the result of the manipulation performed. During the entire recovery period, a woman may experience heavy vaginal discharge. In the first weeks they will be bloody, and later they will become transparent. It is important that they do not have purulent impurities or unpleasant odor. By the 10th day after surgery, a scab will form on the treated area.
Complications
The main complication of surgical treatment is considered to be recurrence of dysplasia after conization. In this case, the issue of the need to remove the entire cervix is decided. In order to promptly detect recurrent pathology, it is necessary to regularly visit a gynecologist for a preventive examination. You should consult a doctor immediately after conization if you have the following symptoms:
- heavy bleeding;
- absence of regular menstruation (as a rule, conization does not affect the cycle);
- increased body temperature;
- purulent vaginal discharge, unpleasant odor;
- abdominal pain that lasts more than a week or gets worse.
As a result of the operation, infection of the cervix and uterus may occur. If this complication occurs, treatment is prescribed, which includes the use of local and systemic antibiotics.
Pregnancy
Reviews from doctors indicate that electroconization of the cervix for dysplasia is the best treatment option if pregnancy is planned in the future. The operation does not prevent conception, but reduces the chances of its early occurrence. The fact is that after conization, the cervical canal partially loses the ability to produce mucus, which is necessary for the transport of sperm.
Reviews from women say that problems can begin when carrying a child. Due to partial removal of the cervix, the threat of premature birth remains throughout pregnancy. If a recurrence of grade 3 dysplasia occurs during gestation, treatment is carried out after childbirth. In this case, delivery is carried out by caesarean section.
Treatment of dysplasia: modern techniques
Cauterization is the main method of modern medicine designed to treat erosion. The action is achieved through exposure to liquid nitrogen, laser or electrocoagulation. In severe cases, the electroconization technique is used. A prerequisite for recovery is the cessation of casual sex, getting rid of sexually transmitted diseases, and cessation of nicotine addiction.
The greatest risk of degeneration of dysplasia into cancer is in patients infected with oncogenic strains of the human papillomavirus. In this case, it is necessary to ensure proper antiviral effects and stop the patient’s attention on the need to take immune drugs.
Detection of dysplasia is always an indication for cauterization, despite the fact that first-degree lesions can be successfully treated with various medications. It has been proven that the effectiveness of radical methods is somewhat higher and this can reduce the risk of developing a malignant process in the patient.
There is a limited list of contraindications for cauterization:
- severe deformities of the cervix;
- rough scars on the surface of the mucous membranes;
- suspicion of the development of a benign or malignant tumor process localized in the ovaries or uterus;
- period of menstrual bleeding;
- pregnancy and breastfeeding.
A temporary contraindication to surgery is the presence of infectious or inflammatory processes localized in the organs of the reproductive system. In this case, cauterization is carried out immediately after the elimination of the diseases.
Attention! For grade 3 dysplasia, the cryodestruction technique is not used because it does not show its own effectiveness.
Electrocoagulation of cervical dysplasia
This technique is simple, but has both advantages and disadvantages. Due to the occurrence of adverse reactions in the early postoperative period and the painful healing process, it is considered outdated. The principle of operation is that a high frequency current passes through damaged areas of the cervix affected by dysplasia. Under this influence, partial necrosis of the affected cells is ensured. The electrocoagulation technique ensures the destruction of massive tissue fragments, which is why the recovery process is delayed.
The main advantage of this technique is its availability and low cost of service. The equipment necessary for cauterization is available in every municipal clinic, therefore the treatment is carried out under a health insurance policy. The process takes no more than 30 minutes.
Modern medical centers are gradually abandoning the use of this method of therapy, because it has a lot of negative aspects. For example, the recovery process is complex and lengthy, and there is a risk of complications due to infection.
Laser cauterization of cervical dysplasia
Laser cauterization has many advantages in comparison with other methods of treating dysplasia, and therefore is actively used in the treatment of various gynecological pathologies. Using the action of the equipment, the doctor acts precisely but precisely on the affected tissues, provoking their evaporation. A significant disadvantage of this popular method is that there is no possibility of collecting samples for histological examination.
List of main advantages of the method:
- directed action;
- controlled depth of influence;
- absence of cervical deformation;
- absence of rough scars;
- the recovery period is about 5 weeks;
- intervention time is 7-10 minutes.
Such manipulation requires the use of special and expensive medical equipment, which is not available to all centers.
Radio wave cauterization of cervical dysplasia
Cauterization of erosion is ensured using a special electrode. It affects the tissue of the cervix using high frequency radio waves. The technology is seen as new, but at the same time proven. Radio wave surgery is actively used in gynecology and has already proven its effectiveness.
Due to targeted precision during the operation, the doctor can destroy even small lesions without damaging healthy tissue. Medical procedures can be carried out even on an outpatient basis. The risk of surface infection is minimized because there is no contact between the radio knife and the affected surface. After healing in the treatment area, a scar does not form, and the total procedure time is about 10 minutes.
Attention! In the first few days after the intervention, the patient begins to have bloody discharge and her body temperature rises. Such adverse reactions are normal and do not require additional intervention.
Cryodestruction of cervical dysplasia
The area with suspected dysplasia is exposed to liquid nitrogen using a special device. The product ensures freezing of cells to a depth of 4-5 mm, therefore several procedures are required to achieve a therapeutic result. Moderate dysplasia is often treated using this method.
Due to exposure to cold, pronounced anesthesia of the affected area is provided. A soft and invisible scar is formed in the area of influence; the woman does not experience difficulties with arousal during sexual intercourse. The likelihood of vaginal bleeding is minimized, as is the risk of other complications.
The postoperative period takes about 3 weeks. At this time, the affected tissues are rejected from the vagina. The appearance of purulent discharge is likely, the abundance of which depends on the volume of the treatment area.
Everything a patient should know about electronization of the cervix
Electroconization of the cervix - what is it? If the development of a malignant neoplasm is suspected, a histological examination is performed. To obtain biological material and treat pathology, doctors prescribe electroconization, which is based on excision of a part of an organ through the application of current. At the end of the operation, the resulting material is transferred to laboratory assistants for histological examination.
Electroconization of the cervix
What is electroconization
Electroconization of the cervix is the excision of a cone-shaped section of a woman’s reproductive organ through the use of electric current. During surgery, the following is removed: the cervix and the uterine canal. Loop-shaped electrodes of various sizes are used during the operation. Despite the convenience of using this method, it has a drawback - when using electrodes, the specialist cannot control the depth of organ excision. There is a risk of developing: bleeding, recurrence of a cancerous tumor, narrowing of the cervix.
Indications
Electrodiathermoconization of the cervix is prescribed when pathogenic changes, epithelial dysplasia are detected. The main indications are:
- identifying areas of change in the cervical epithelium;
- detection of pathogenic cells;
- organ dysplasia of 2–3 degrees – the patient does not feel symptoms of the disease, but if left untreated, complications may develop;
- erosive changes in the cervix;
- keratinization of the organ mucosa (leukoplakia);
- cicatricial changes in the cervix - develops due to ruptures during injury;
- formation of polyps;
- recurrent dysplasia after surgery (electrodiathermoconization of the cervix, cryodestruction, laser vaporization);
- ectropion - eversion of the organ mucosa.
The main reasons for electroconization are considered to be: obtaining biological material for histological examination, treatment of malignant neoplasms.
Contraindications
If there is an inflammatory process, electroconization is prohibited. The main contraindications include:
- invasive form of cancer;
- acute form of infectious pathologies, inflammatory processes;
- it is impossible to determine the boundaries of the affected tissues;
- the area affected by cancer cells is larger than the technical capabilities of surgical intervention;
- poor blood clotting;
- chronic pathologies (diabetes mellitus, heart failure, hypertension, liver disease, renal failure).
Purpose of the event
The main goal of surgery is to remove pathological tissues affected by cancer cells. Electrodiathermoconization of the cervix allows you to solve two main problems: detection and treatment of a cancerous tumor.
- Tissue affected by cancer cells is removed. This allows us to achieve positive dynamics in the treatment of cancer.
- Based on the received materials, the laboratory assistant conducts a histological examination of the tissues.
- For a non-invasive form of cancer, excision of a cone-shaped section of the organ is enough to completely cure the cancer.
How is surgery performed?
Electroconization is a modern method of diagnosing and treating a non-invasive form of cancer, in which the patient does not have to go to the hospital; all manipulations are performed on an outpatient basis. Immediately before setting the date for the operation, the woman will have to undergo a series of tests, which will determine the possibility of the operation.
Preparation for electroconization
Surgery is performed after the completion of the menstrual cycle, on days 1–2. This is explained by the fact that during this period, the female body has a large amount of estrogen, which promotes a speedy recovery of the patient.
Before scheduling an operation, a woman needs to prepare. A month before the planned surgical intervention, the patient must undergo: consultation with specialists, some examinations:
- consultation with a gynecologist, immunologist;
- smear to determine vaginal microflora;
- Ultrasound of the pelvic organs, lymph nodes;
- biopsy.
If pathologies are detected, the time for surgical intervention is postponed until the inflammatory process is completely relieved. Two weeks before the operation, the woman will have to undergo several examinations and tests.
- UAC, OAM.
- Blood for syphilis, antibodies to HIV and viral forms of hepatitis.
- Hemostasiogram.
- Examination, consultation with a gynecologist.
- Blood type, Rh factor.
- Fluorography for the last year.
- ECG.
- Consultation with a therapist.
Features of surgical procedures
When performing electroconization, equipment for electrowave surgery “Surgitron” is used. This is an electric generator complete with a set of electrodes of various sizes. Excision of the required area of tissue is carried out using high-frequency current.
The affected tissue is removed with a loop electrode, the size of which is pre-selected by a specialist. When performing surgical intervention, it is important to consider that the size of the tissue area to be removed should be 3–4 mm larger than the volume of the affected area. Directly during the operation, a high-frequency current is applied to the electrode. The specialist begins to rotate the electrode in a circle, cutting tissue to a depth of 5–8 mm.
This type of surgery is the most common and has a number of advantages:
- all manipulations are performed under local anesthesia;
- For the operation, a woman does not have to go to the hospital;
- the risk of bleeding is minimized due to rapid coagulation of blood vessels;
- the temperature in the excision area does not exceed 55 °C, therefore the risk of burns is zero;
- all the material obtained has almost no damage and the laboratory assistant can make a diagnosis with maximum accuracy;
- the risk of complications is minimal.
Methods and features of the operation
Conization of the cervix is performed in a hospital setting; the degree of surgical intervention and the method of its implementation depend on the patient’s condition and the level of pathological changes. This procedure is prescribed for dysplasia of various stages, erosive lesions of the mucous surface and if a cancerous tumor is suspected.
During the examination, laboratory methods determine the presence or absence of cancer cells. If the biopsy result is positive, more in-depth studies and appropriate treatment are prescribed.
If the last stage of cervical cancer is diagnosed, the entire organ is removed to prevent further spread of metastases and their development into malignant neoplasms in neighboring areas.
If dysplasia is detected - the predominance of atypical cells in the epithelial layer, removal of the damaged area is necessary, while the organ is preserved. To prevent further progression of the pathology, during excision, part of the healthy flesh is captured (about five millimeters), which increases the size of the wound surface, but eliminates the risk of recurrent manifestations of the disease.
- Knife - conization is carried out using a scalpel. The method is considered the most traumatic, so it is used very rarely. The procedure is quite painful, which requires pain relief measures. The healing period after tissue excision using this method is quite long, and serious complications often occur in the form of bleeding and infection of the wound with pathogens. As healing progresses, a scar forms, which can become a problem during pregnancy and subsequent childbirth.
- Laser is the newest method of performing gynecological operations. Using a laser, maximum precision in removing altered layers of epithelium is achieved. During the operation, the specialist has the ability to change the depth of exposure and the size of the area to be removed. The cervical canal is excised more carefully, which reduces the risk of postoperative complications. During the recovery period, the patient may experience slight bleeding, nagging pain that persists for a short time, and a feeling of discomfort. After conization of the cervix, the functionality of the organ is preserved, and the possibility of bearing a fetus increases several times. The method is quite expensive, which is its significant drawback, since it remains inaccessible to many women.
- Loop - carried out with a special electrode loop through which alternating current passes. It is prescribed for the removal of cysts, polyps, and is also used for conization if there is a suspicion of the presence of atypical cells. The method is high-tech, allowing to minimize pain and bleeding after the procedure. Biological material taken using an electric loop is practically not damaged, which facilitates its further research.
- Radio wave is the most common and least traumatic method. Coagulation of damaged tissue occurs through exposure to high-frequency waves, and there is no pain, since soft tissues lose sensitivity due to the death of nerve endings. After conization of the cervix using the radio wave method, reproductive function is completely preserved, and after the procedure there is virtually no risk of complications.
The procedure is carried out immediately after the end of menstruation for 1-2 days (so that there is no discharge). In this case, the patient needs to prepare in advance.
At least a month before the planned date of conization, a woman must undergo a gynecologist, colposcopy, and take smears for microflora. Then the doctor may prescribe additional tests, such as ultrasound of the pelvic organs, lymph nodes, etc.
14 days before the day of surgery, the patient must donate blood for a general analysis, and also be checked for the absence of HIV, syphilis, hepatitis B and C. In addition, the following studies are necessary:
- Analysis of urine;
- PCR research;
- vaginal culture for the presence of microflora;
- hemostasiogram;
- blood test for group and Rh factor.
Indications for conization are the following conditions in women:
- internal ruptures, scars and damage to the cervical canal and cervix resulting from severe labor;
- suspected cancer for diagnosis or treatment;
- ectropion;
- dysplasia;
- polyps;
- erosion and pseudo-erosion;
- hypertrophy, etc.
It is the early diagnosis of dysplasia and conization that makes it possible to avoid the disease from turning into cancer.
Recommendations for preventing complications
After surgical removal, an open wound remains. To avoid complications, a woman needs to reduce any pressure on a weakened organ:
- abstain from sexual intercourse for a month;
- exclude the use of tampons during menstruation, it is better to give preference to gynecological pads;
- avoid stressful situations, moral stress;
- do not take a bath (especially a hot one), it is better to limit yourself to a cool shower;
- do not lift weights weighing more than 3 kg;
- normalize your daily routine, sleep at least 8 hours a day;
- take vitamin complexes that increase the functionality of the immune system;
- observe the rules of intimate hygiene;
- use intimate hygiene products without fragrances;
- eat right, include in the menu dishes rich in vitamins (fruits, vegetables, cereals);
- avoid hypothermia, overheating;
- Avoid taking medications that reduce blood clotting.
Modern methods of diagnosing and treating cancer tumors allow us to achieve the most effective results. Due to minimal tissue damage during electroconization, the risk of complications is minimal.
Electroconization of the cervix for dysplasia
Cervical dysplasia is a precancerous pathology, which is characterized by the growth of atypical cells in the epithelium. Dysplasia is one of the most commonly diagnosed diseases in women of reproductive age. The pathology is otherwise called pre-invasive oncology or in situ cancer.
The cervix is part of the reproductive system, which connects the uterine body and the vagina through the cervical canal. The cervical canal prevents infection from entering the vagina into the uterus, which is sterile. This is achieved due to the anatomical narrowness of the canal and the presence of special glands that produce protective mucus. The surface of the canal is lined with cylindrical single-layer cells.
A significant part of the cervix is inaccessible for examination. During a gynecological examination, only the vaginal part can be visualized, which is covered by flat multilayered cellular elements.
The epithelium of the cervix consists of several layers:
- basal;
- intermediate;
- superficial.
The deepest layer, called the basal layer, contains immature round cells with a large nucleus. As they mature, they rise and undergo flattening. With dysplasia, this natural process is disrupted. Cells acquire signs of atypia.
With dysplasia, structural changes occur in the cervical epithelium. The normal division into layers is also lost.
The development of dysplasia is divided into 3 degrees.
- No more than a third of the thickness of the epithelium is involved in the pathological process.
- Damage to more than a third of the cervical epithelium.
- Distribution of atypical cells over more than half the thickness of the epithelium.
Grade 3 dysplasia is considered pre-invasive cancer and differs from oncology in the absence of growth of malignant cells into the stroma. With grade 3, doctors resort to surgical treatment, for example, conization of the cervix.
How erosion degenerates into dysplasia
It is difficult to determine exactly how long it will take for erosion to transform into dysplasia. Much depends on the location of the lesion and its depth. In most cases, progress is not rapid and takes about six months.
The causes of the lesion may be the following:
- activity of oncogenic strains of human papillomavirus types 16 and 18;
- decreased immunity;
- poor nutrition, namely a lack of fresh vegetables and fruits in the diet;
- hereditary predisposition;
- overweight or obesity 2-3 degrees;
- long-term use of antibiotics and combined oral contraceptives;
- chronic fatigue.
Can pain occur with cervical dysplasia? As a rule, there is no pain because the cervix is devoid of nerve endings. This is precisely the danger of its pathologies - it is almost impossible to identify the disease in the early stages on your own.
The impact of these factors is sufficient to provoke the transition of cervical erosion to dysplasia. The main reasons that increase the risk of developing pathology in women of reproductive age include: nicotine addiction, HPV infection, and lack of vitamins in the body.
There are 3 stages of pathology development:
| Stage | Description |
| Stage 1 (mild) | Characterized by damage to 1/3 of the entire depth of the mucous membranes. |
| Stage 2 (moderate) | Captures 2/3 of the depth. |
| Stage 3 (severe) | All vaginal mucous membranes are affected, but the basement membrane is not affected. |
Doctors are also considering the fourth and final stage, but it is not included in the modern classification of the disease. At this stage, so-called precancer is diagnosed.
Causes
In modern gynecology, a direct connection has been proven between the appearance of dysplasia, in particular, grade 3, and HPV. This virus, entering a cell, causes cellular mutations. However, the development of a pathological process often requires exposure to certain negative factors:
- family history;
- chronic inflammatory and infectious processes in the pelvis;
- disorders in the immune system;
- smoking;
- hormonal imbalance;
- onset of sexual activity at a young age;
- cervical injuries;
- disorderly intimate life.
In most cases, the clinical picture of dysplasia is absent. Characteristic signs usually appear as the disease progresses to stage 3 and after the addition of infection.
Among the symptoms with the development of grade 3 dysplasia are:
- nagging pelvic pain;
- genital discomfort;
- pathological discharge, which may be accompanied by an unpleasant odor;
- contact discharge during sexual intercourse and gynecological examination.
How to detect dysplasia
The initial stage of gynecological diagnosis is examination of the woman’s cervix in the speculum. Already at this stage, disturbances indicating the development of a pathological process can be detected. The list of important diagnostic criteria includes:
- change in the shade of the vaginal walls;
- hypertrophy of the mucous membranes;
- shine in the throat area;
- uncharacteristic uniformity of the epithelium;
- the presence of whitish lesions on the mucous membrane.
When such changes are detected, other methods are used to confirm the presumptive diagnosis:
- PAP test. During the examination, a cytological examination of epithelial tissue under a microscope is performed. Tissue samples for examination are taken from different areas of the cervix to obtain an accurate diagnostic picture. This method allows you to get an accurate and informative picture and identifies markers that provoke the process. Allows detection of HPV.
- Extended colposcopy. Used as an additional diagnostic method in the case. When the accuracy of cytological examination is not enough. To confirm the diagnosis and detect atypical areas, special reagents (acetic acid solution and Lugol) are applied to the cervix.
- Biopsy. To conduct an examination using this method, the collection of biological material is required. The method allows you to determine not only the degree, but also the nature of dysplasia, eliminating the development of oncology.
- PCR diagnostics. A targeted immunological method to detect HPV. Based on its results, doctors can choose the most convenient method of medical and surgical treatment.
Attention! To determine an accurate diagnosis, a biochemical blood test and a study of hormone balance are required.
The main goal of the doctor conducting the examination is to differentiate the diagnosis. The following diseases have a similar clinical picture and manifestations:
- leukoplakia;
- cervicitis and other infectious pathologies;
- erosion and pseudo-erosion.
Particular attention to the differential diagnosis of dysplasia should be paid to the older age group. In menopausal patients, the appearance of visible changes in the cervical mucosa is often due to a natural process. It appears against the background of pronounced hormonal fluctuations (lack of estrogen).
Diagnosis and treatment
The following methods are used to detect pathology:
- gynecological examination;
- smear for oncocytology;
- PCR research;
- extended colposcopy;
- biopsy;
- blood test for tumor markers, syphilis and HIV;
- bacterial culture and general smear;
- hormonal diagnostics;
- Ultrasound of the pelvic organs.
The main research method is cytological diagnosis, which involves taking material from different parts of the cervix to identify atypical cells and the inflammatory process.
Treatment of grade 3 dysplasia is predominantly surgical, which most often consists of conization of the cervix. At the initial stage or during pregnancy, observational tactics may be used. The patient regularly visits the doctor and undergoes examination.
The progression of pathology is an indication for the use of surgical techniques.
- Conization. This intervention refers to organ-preserving tactics. The operation involves removing a cone-shaped area of the cervix that includes abnormal tissue. The amputated tissue contains fragments of the cervix and cervical canal. Manipulation is carried out for both diagnostic and therapeutic purposes.
Conization of the cervix can be performed in different ways.
1. Knife. The operation is performed with a scalpel. In modern gynecology, such conization is used infrequently due to its high morbidity. In addition, there are more effective and gentle methods.
2. Laser. Conization using a laser beam is considered the most expensive.
3. Electroconization. This intervention is otherwise called loop conization. This is the most common type of conization.
- High amputation. With this tactic, radical amputation of the cervix occurs, which is recommended for grade 3 dysplasia and oncological alertness. The high amputation method allows you to stop the progression of the malignant process.
Before conization and other surgical interventions, a woman performs the necessary examination:
- general and biochemical blood test;
- diagnosis of syphilis and hepatitis;
- general urine analysis;
- flora smear;
- PCR swab;
- colposcopy;
- biopsy.
Conization of the cervix can have negative consequences.
- With conization, the anatomy of the cervix changes. As a result, the cervical canal remains dilated, which can lead to chronic infections.
- There is a risk of relapse in case of technical difficulty in performing conization, which is caused by some anatomical features of the cervix.
- After conization, the ability of the cervix to transform into the birth canal is lost, which necessitates surgical delivery.
- Conization does not affect a woman's reproductive ability, however, it increases the risks of miscarriage and premature birth.
- During conization, it is difficult for the surgeon to calculate the depth of impact; as a result, too large areas of healthy tissue may be captured. Sometimes in nulliparous patients, the doctor amputates a small amount of the affected epithelium, which leads to relapse of dysplasia.
In order to prevent the development of the inflammatory process, the patient is given antibacterial treatment. In case of severe pain, taking painkillers is indicated.
For a month after conization, a woman is not recommended to visit a sauna or swimming pool, lift weights, or use tampons. Sexual activity is also prohibited due to the risk of infection and unnecessary trauma to the damaged cervix. Repeated colposcopy is performed no earlier than four months after conization of the cervix.
Material and methods
At the first stage, in order to identify risk factors for relapse and progression of CIN, a retrospective assessment of the management tactics of 122 patients with severe forms of cervical dysplasia - cervical intraepithelial neoplasia II-III degrees (CIN II-III) for the period from 2007 to 2015 was carried out. Of these, 60 patients (1st control group) who did not have relapses of the disease after treatment, and 62 patients (1st main group) who were diagnosed with relapse of dysplasia. At the second stage, based on data from the analysis of risk factors in patients with recurrent dysplasia, a step-by-step algorithm for the management of CIN II-III was developed, including expansion of the diagnostic spectrum of examination, lifestyle correction, pre-excision preparation followed by radio wave excision, post-excision stimulation of repair, stimulation of antiviral immunity, carrying out rehabilitation. The expanded range of examination included: cytological examination, extended colposcopy, the FEMOPLOOR test to assess the vaginal microbiome, determination of vaginal pH, a study to determine HPV types of highly oncogenic types (14) with the establishment of a quantitative load, ultrasound of the pelvic organs and mammary glands (in women over 40 years of age) - mammography), study of hormonal status, endometrial biopsy. Pre-excision preparation was carried out using a complex domestic preparation containing interferon alpha-2b, fluconazole, metronidazole and boric acid in the form of suppositories vaginally at night for 10 days, excision type LEEP/LLETZ (loop electrosurgical excision procedure - loop electroconization of the cervix/large loop excision of transformation zone - wide loop excision of the transformation zone) was carried out using FOTEK 140 or Surgitron devices, post-excision stimulation of reparation was carried out with a vaginal gel containing dihydroquercetin (0.4%), lecithin (3%), glycine (5%), an antiseptic of plant origin (0.01%) within 10 days. Stimulation of the antiviral response after excision of the pathological focus was carried out with a domestic preparation of plant origin, which is a biologically active polysaccharide obtained from the Solanum tuberosum
(tuberiferous nightshade) and belonging to the class of high molecular weight hexose glycosides of complex structure (panavir). This drug has a direct effect on the virus and also provides an additional immunocorrective effect. The drug was prescribed according to a regimen consisting of 5 intravenous injections given at intervals of 48-72 hours. Rehabilitation included the correction of hormonal disorders and the prescription of additional therapy with a dietary supplement for 6 months. In patients planning a pregnancy, after completing a rehabilitation course for 6 months, the drug dydrogesterone was prescribed at a dose of 20 mg/day from the 16th to the 25th day of the menstrual cycle; in women who did not plan to become fertile, combined oral contraceptives or a vaginal system containing etonogestrel 11.7 mg, ethinyl estradiol 2.7 mg were used; in prolonged mode 42+7. Additional therapy was carried out with a dietary supplement - a source of flavonoids, containing 45 mg of epigallocatechin-3-gallate and 90 mg of indole-3-carbinol in a dose of 2 capsules 2 times a day for 6 months. In the presence of vaginal prolapse, patients underwent a 6-month course of training to strengthen the pelvic floor muscles (PFM) with vaginal cones (5 patients) or minimally invasive perineoplasty (3) in combination with a course of PFMT.
At the third stage, the 2nd main group of patients was formed (32 women, including 13 who planned pregnancy after completion of therapy), treated according to the developed management algorithm. The effectiveness of treatment was compared with the generally accepted treatment regimen, which included excision with stimulation of antiviral immunity with a herbal preparation, which is a biologically active polysaccharide obtained from the Solanum tuberosum
(2nd control group - 30 patients, including 12 who planned to have children after treatment).