It happens that during self-examination or by chance, a woman may identify some kind of lump in the vaginal area. Such a situation will seriously alarm you and throw you out of emotional balance. Various guesses will begin to appear, most often with negative connotations. But what a formation in the vagina actually means can be found out only after consulting a doctor. Until then, it’s better not to worry in vain.
After childbirth, growths in the vagina
Growths in the vagina may turn out to be scars.
They are formed as a result of ruptures.
Ruptures are often observed in women after vaginal delivery.
If the deep layers of the mucosa are damaged, even suturing the damage can ultimately lead to scarring.
These scars can cause discomfort in the future.
Pain appears during sexual intercourse.
These growths inside the vagina can be removed surgically.
Laser, electrocoagulation, and radio wave removal are used.
The procedure is painless because infiltration anesthesia is used.
Pathology
Developmental anomalies
Aplasia—the absence of a vagina—is usually diagnosed during puberty. Treatment of V. aplasia—see Colpopoiesis. Other malformations of V. are V.’s partitions, its doubling, often combined with doubling of the uterus (see).
Damage
In case of mechanical damage (during coitus, falling on sharp objects, during labor), the integrity of its wall is disrupted.
During childbirth, the lower part of the vagina is most often damaged, the edges usually rupture simultaneously with the perineum. The middle part is damaged less frequently, ch. arr. during obstetric operations (application of forceps). The upper part of the V. can be damaged simultaneously with uterine rupture - ruptures of the vaginal vault and lower uterine segment. Separation of the V. from the uterus (colporexis) is extremely rare. When the walls of the V. are pressed against the pelvic bones for a long time by the presenting part of the fetus during childbirth, due to circulatory disorders, necrosis may occur with the formation of fistulas connecting the V. with neighboring organs (see Genitourinary fistulas). In elderly women, when wearing pessaries due to prolapse of the uterus and vagina, bedsores may form in the wall B.
Damage to the V. can occur when a foreign body is introduced into it, in particular when attempting to terminate a pregnancy (see Foreign bodies, vaginas and uteruses). Open injuries can be the result of an accident - falling on sharp objects, car and train accidents, gunshot wounds. As a result of injury to the V., a hematoma may form; the edges are usually localized in the upper half of the V. at first, and subsequently spread to the external genitalia.
Patients who have suffered vaginal trauma should be given antitetanus serum; if the walls of the V. rupture, sew up the wound. Large dense scars that are not amenable to conservative treatment, formed as a result of injury, preventing the outflow of menstrual blood, sexual intercourse, or the birth of a fetus, should be excised with extreme caution to avoid damage to neighboring organs.
Diseases
The most common diseases of the vagina are vulvovaginitis (see), colpitis (see), which can be complicated by narrowing and fusion of the vagina (see Gynatresia), especially in girls and older women. In older women, prolapse and prolapse of the vulva occur (see Prolapse of the uterus and vagina).
Surgical treatment for displacement of the genital organs - see Colpopexy, Colpoperineoplasty, Colporrhaphy.
Tumors
Benign tumors
Vaginas are rare. Of these, in first place in frequency are cysts, which are located mainly in the lateral sections, developing from the remnants of the longitudinal ducts of the epididymis, along the midline (from the paramesonephric ducts) or atypically in the thickness of the wall B. They are usually single-chamber, round or ovoid in shape, size rarely more than 7-9 cm. The contents are serous. V.'s cysts, especially small ones, are usually asymptomatic and are detected during examination of the woman; With large cysts, patients note difficulty or pain during sexual intercourse. When recognizing a cyst, it is necessary to exclude cystocele (see), rectocele (see), urethral diverticulum (see Urethral canal).
Fibroids develop from connective and muscle tissue. The tumor usually appears as a single node of varying sizes: from the size of a pea to the head of a newborn. The consistency of the node is dense. Small tumors are asymptomatic. As they grow, they protrude the wall of the V. or are located in its lumen, being connected to the wall by a wide base or a thin stalk. Large tumors, especially those located close to the entrance to the V., cause unpleasant sensations of a foreign body in the V., complicate sexual intercourse, can cause compression of neighboring organs and cause disturbances in urination and defecation. Hyaline degeneration of the tumor, its calcification, ulceration and necrosis may be observed. Recognition is based on palpation detection of the node. When the tumor is located in the upper part of the V., it is difficult to determine from which organ it develops, and this can only be clarified during surgery.
Papillomas are single or multiple nodules that, growing, have the appearance of cauliflower; they are difficult to distinguish from cancer. Polyps, especially when their surface is ulcerated, resemble cancer or sarcoma. The diagnosis is clarified using cytol. and gistol, methods.
Hemangioma is a very rare tumor - a bluish-purple tumor with a soft consistency.
Treatment of benign tumors is surgical. Cysts and fibroids are enucleated. If it is difficult to remove the cyst, it is permissible to partially leave the wall, the edges are sheathed, the remaining flat base is drained; subsequently it is covered with multilayered squamous epithelium B.
Polyps and papillomas are scraped off with a sharp spoon or cut with scissors.
Rice. 1. Vaginal cancer. Rice. 4. Cancer of the upper third of the vagina (uterus and vagina in section).
Malignant tumors
V. are primary and secondary. Primary vaginal cancer is approx. 2-3% of all malignant tumors of the genitals; it occurs predominantly between the ages of 40 and 60 years. The posterior wall of the V. in its upper third is most often affected (tsvetn. Fig. 1 and 4). The growth form is exophytic, less often endophytic. With histol. The study reveals squamous cell carcinoma, rarely adenocarcinoma (from dystopias - remnants of mesonephric and longitudinal ducts). The tumor is limited, dense, and easily vulnerable. Before the tumor ulcerates, the patient often does not notice any symptoms that force her to see a doctor. Only occasionally there are complaints of bleeding during sexual intercourse. When an ulcer forms from the V., watery, bloody, bloody discharge appears, and bleeding occurs at times; later pain occurs and the functions of neighboring organs are disrupted, anemia, general weakness, and cachexia are noted. The tumor usually spreads along the length and along the lymphatic tract. When cancer is localized in the upper or middle third of the V., the internal iliac and sacral (deep and superficial) lymph are affected. nodes, in the lower third - inguinal. Distant metastases (to the lungs, liver and other organs) are rare. It is possible for the tumor process to spread to the rectum or bladder. Division by stages of cancer spread: Stage I - tumor up to 2 cm in diameter without metastases; Stage II - large tumor with infiltration of peri-vaginal tissue, single mobile metastases in the inguinal lymph nodes; Stage III - the tumor occupies more than two-thirds of the V. with infiltration of paravaginal tissue and transition to the pelvic wall, multiple metastases to regional lymph nodes; Stage IV - the tumor has spread to the bladder, rectum, or there are distant metastases. The diagnosis is usually not difficult.
Differential diagnosis should be made with benign and other malignant tumors, with endometriosis, tuberculosis, syphilis, chancroid, colpitis and drug burns. The final diagnosis is made after a biopsy. During the clinical examination, curettage of the cervix and uterine body is indicated.
Treatment is predominantly combined radiation (external and intracavitary). Surgical treatment is a rare exception.
Secondary cancer of V. arises either along the extension from neighboring organs, or metastatically with primary localization in the body of the uterus, ovaries and other organs.
Rice. 3. Metastasis of chorionepithelioma to the vaginal wall.
Of the secondary tumors, chorionepithelioma is the most common after cancer (see Trophoblastic disease), metastases are more often localized in the lower parts of the V. (color. Fig. 3).
Sarcoma V. is observed extremely rarely; its form is completely different in children and adults.
Sarcoma V. occurs in children before three years of age. It is characterized by rapid growth and a tendency to decay, appears in the form of a small nodule, grows rapidly and takes on a polypous or grape-shaped form. The tumor bleeds moderately when touched, usually develops on the anterior wall of the uterus, and invades the bladder, urethra, and cervix early; is manifested by the appearance of dirty, later bloody discharge from the V. The diagnosis is based on the detection in the area of the entrance to the V. of polypous formations that bleed when touched, on data from a cytological examination of discharge from the V. and histol, and examination of suspicious tissue. Surgical treatment is not effective.
The prognosis is unfavorable.
Rice. 2. Sarcoma of the vagina with necrosis.
Sarcoma of the vagina in adults develops in various parts of the V. There are two forms of growth: nodular and diffuse. In the first form, a small nodule of dense consistency develops (softer than with fibromyoma). The tumor is connected to the wall by a stalk of varying width. Subsequently, the nodule ulcerates. In the diffuse form, the tumor has the appearance of a dense infiltrate, spreading along the wall of the V. and narrowing its lumen; subsequently ulceration occurs (tsvetn. fig. 2). Sarcoma in adults rarely grows into neighboring organs; metastases often form in regional lymph nodes and distant organs (for example, lungs). Clinical manifestations are scanty. With ulceration, serous-bloody and purulent leucorrhoea mixed with blood appears. As the tumor grows, the sensation of a foreign body in the V., bleeding, and urinary disorders occur.
When making a diagnosis, one should take into account the possibility of V. cancer, disintegrating fibroids, syphilitic ulcers, metastasis in V. with sarcoma and chorionepithelioma of the uterus.
Treatment is predominantly combined radiation (external and intracavitary). Patients with the nodular form of V.'s sarcoma can be recommended radical surgery (removal of the tumor within healthy tissue) followed by radiation therapy.
To create favorable conditions during intracavitary curitherapy, the tumor node is sometimes removed or the pedicle connecting it to wall B is dissected.
The prognosis is unfavorable, but better than with V.’s sarcoma in children. Cases of cure have been described.
Oncological diseases and growths in the vagina
Cancer of the vulva or vagina is one of the causes of large growths near or inside the vagina.
These formations may look different.
Some women complain of a dense, cartilaginous growth in the vagina.
In other cases, only erosion is detected.
Such erosive growths at the entrance to the vagina are very dangerous.
They may indicate that the tumor has begun to disintegrate.
At the same time, subjective sensations are noted.
This is pain, burning.
Quite pronounced swelling may form.
Research methods
Rice.
15. The first degree is the presence of epithelial cells and Dederlein rods. Rice. 16. Second degree—decrease in the number of Dederlein rods, appearance of leukocytes. Rice. 17. Third degree - few Dederlein bacilli, increase in the number of leukocytes and microflora. Rice. 18. Fourth degree - Dederlein's rods are absent, there are many leukocytes and microbes. Methods for examining the vagina: using mirrors, colposcopy (see), internal digital examination, combined rectovaginal examination using laboratory methods (important indicators of the condition of the vagina are the degree of purity, cytological picture of the vaginal contents), if necessary, one should resort to histological examination of the material. To examine the V. in virgins, you can use a vaginoscope with a lighting system, a colposcope of the A. G. Kahn system, or a thoracoscope with direct optics. X-ray examination of women with V. anomalies allows one to see the size, position of the V., and identify developmental anomalies of other organs. To judge the functional state of V., dynamic X-ray colpography can be used.
Vaginal flora. In the V. of healthy women, Dederlein's bacilli are usually present, which may not be of the same species composition. In women outside pregnancy, Lactobacillus fermenti and Lactobacillus plantarum are more common, in pregnant women - Lactobacillus acidophilus.
In accordance with the nature of the cellular contents and microflora of V., four degrees of its purity are distinguished (color fig. 15-18). At the first degree of purity, only epithelial cells and Dederlein rods are present in it; the reaction of the vaginal contents is acidic (pH 4.0-4.5). With the second degree of purity, V. contains less Dederlein bacilli; leukocytes and gram-positive diplococci appear in small quantities; there are still many epithelial cells in the smear, the reaction of the V. contents is acidic (pH 5.0-5.5). The third degree of purity is characterized by the presence of a small number of Dederlein bacilli, a significant increase in leukocytes in the smear, as well as a diverse microflora; the reaction of the contents of V. is slightly acidic or slightly alkaline (pH 6.0-7.2). At the fourth degree of purity, Dederlein bacilli are absent in V., instead of them various microbes are found in large quantities: streptococci, staphylococci, E. coli; Trichomonas vaginalis is often possible. Leukocytes predominate among the cellular elements. The reaction of vaginal contents is alkaline (pH over 7.2). The first and second degrees of purity are considered a sign of a healthy state of the plant, and the third and fourth indicate an inflammatory process.
Growths in the vagina due to mechanical damage
Mechanical irritation can cause a growth at the vaginal opening.
It may be caused by:
- administration of Betadine suppositories or any other
- too rough sexual contact
- medical procedures
- depilation
- independent use of various devices with intravaginal administration (Kegel exercisers, pessaries, etc.)
The growths themselves on the vaginal mucosa are scars.
It could also be elements of a rash.
They arise as a result of inflammatory processes in those places where damage has occurred.
Causes
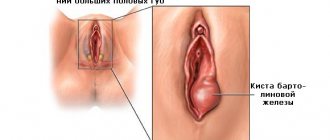
A mass formation in the area of a woman’s external genitalia can have different origins. And you need to understand all the reasons so as not to miss the really important ones. A lump in the vagina, as ordinary people call it, is the result of inflammatory, hyperplastic or other processes. The source of pathological growth can be the glands of the vulva, the vaginal wall (mucous, muscular, serous membranes) or nearby tissues. The cause of this formation is most often benign diseases:
- Bartholinitis.
- Cyst.
- Fibroma.
- Lipoma.
There are cases when the cervix is mistaken for a lump, which, due to weakness of the pelvic muscles, descends all the way to the vestibule of the vagina. But a similar situation is more often observed in old age in women who have undergone more than one childbirth and have been involved in heavy physical work in the past. But young girls are most afraid of oncology, although this is also unlikely, because malignant processes are more typical during menopause, when the activity of hormonal control decreases. Then the appearance of vaginal carcinoma is possible.
The origin of a lump in the vaginal area is most often associated with benign processes, but in certain cases, oncology cannot be ruled out.
Condylomas as growths in the vagina
Very often, the growth between the vagina and anus is a condyloma.
In another way, these formations are called anogenital warts.
Their appearance is caused by the human papillomavirus.
These viruses enter cells and damage their DNA.
As a result, their too active division begins.
The papillary layer of the dermis grows.
Characteristic growths form around and inside the vagina.
Infection occurs through sexual contact.
The incubation period can be quite long - several months.
As the wart grows, unpleasant subjective sensations may occur.
Active inflammation often occurs.
The tissues swell, itch, and sometimes cracks appear.
Then growths appear in the vagina, which gradually increase in size.
How many there will be and what size depends primarily on the state of the immune system.
The most severe lesions are observed in immunodeficiency diseases, including HIV.
In this case, the number of condylomas can reach hundreds, or they acquire enormous sizes.
But for most women these are single formations.
In the future, the virus can leave the body on its own.
Although the condylomas remain.
Their spontaneous disappearance is observed in no more than 20-30% of cases.
Moreover, this happens after several months or even years.
Therefore, most people simply have to remove them in a medical clinic.
The papilloma virus can be dangerous.
Because some types increase the risk of malignant neoplasms.
Age and functional characteristics
The vagina of newborns is juicy, the mucous membrane is well developed, the reaction of the vaginal contents is acidic. This condition of the newborn is explained by the influence of sex hormones, which are produced by the placenta (estrogens and progesterone) and transmitted to the fetus. Already by the first month of life and before the onset of puberty, the girl’s genital organs, including the vagina, are in an infantile state. The contents of V. are scanty, the reaction is alkaline or neutral. With the development of ovarian function, changes also occur in the V.: cyclic blood filling of the walls of the V. occurs, the thickness of the epithelial cover increases. Cyclic changes are also observed in V.'s epithelium.
Rice. 19. Glycogen (red at the top of the picture) in the cytoplasm of the stratified squamous epithelium of the vagina.
Age-related features in the structure of the V. epithelium: in newborns - low, single-layer epithelium; in childbearing age - tall, multi-layered; in menopausal women - multilayered, thickened in accordance with the cyclical fluctuations of the ovarian function that has not yet completely extinguished; in old age - low multi-layered. The cytoplasm of the multilayered squamous epithelium of V. contains glycogen, which is associated with the saturation of the woman’s body with estrogens. In girls and menopausal women, there is very little glycogen in the epithelial cells of V.. Its maximum amount is found in mature women in the first phase of the menstrual cycle (color fig. 19). There is a direct relationship between the thickness of the epithelial layer and the level of glycogen content in it. In the connective tissue of women during the childbearing period, there are many elastic fibers; during menopause, collagen fibers predominate.
Functionally, V. is divided into two sections. The upper, expanded part of the V. has the ability to actively contract, while the lower, narrowed part is more passive. V. can change its shape, diameter and depth with contraction of the muscles of the pelvic floor, uterus and the muscular elements of its ligamentous apparatus.
V. plays an active role in the process of fertilization. During the period of sexual arousal, a sharp filling of its veins occurs, transudation into the lumen of the V. increases, the pH of its contents slightly increases, and the upper two-thirds of the V. elongate. The mucous membrane of the V. is capable of absorbing sperm plasma after coitus, prostaglandins E and F, produced by the seminal vesicles.
During childbirth, the vagina is greatly stretched; a week after birth, due to the elasticity of the walls, the vaginal tube contracts, although its lumen remains wider than before birth.
Genital herpes near the vagina
Genital herpes is an infection that is sexually transmitted.
It causes the appearance of growths in the vagina, the causes of which are viral infections of the skin and mucous membranes.
Bubbles containing clear liquid appear.
The pathology is accompanied by burning and other unpleasant sensations in the problem area.
General intoxication symptoms often occur.
A woman's body temperature increases.
Symptoms of genital herpes go away even without treatment.
Although this takes one and a half to two times longer than when receiving adequate antiviral therapy.
Such growths in the vagina are especially dangerous during pregnancy.
Because herpes is one of the most unfavorable viruses for the fetus.
It often causes spontaneous abortions or congenital deformities.
If herpes is detected during pregnancy, the woman must be treated.
This is necessary to prevent infection of the fetus.
Vaginal contents
The lumen of the V. contains 0.5-1.5 ml of liquid formed due to transudate from blood and lymphatic vessels, and mucus, which is produced by the epithelial cells of the endometrial glands and the mucous membrane of the cervical canal. The contents of the vagina have a whitish color, which is caused by an admixture of cells of the vaginal stratified squamous epithelium, and a specific odor associated with the presence of trimethylamine; the acidic reaction is caused by lactic acid, which is formed from glycogen under the influence of Dederlein's rods. Lactic acid destroys pathogenic microbes, promoting the process of self-cleaning B. The content of lactic acid is 0.5% of vaginal discharge.
Growths in the vagina due to sexually transmitted infections
With STDs (chlamydia, gonorrhea, syphilis), inflammatory foci may also appear.
Some women call them growths.
The cause of infection is unprotected sexual contact with the source of infection.
The vaginal mucosa swells.
She is red and painful.
Symptoms of these infections appear after an incubation period.
With gonorrhea it lasts 5-7 days.
With chlamydia, it can last 2-4 weeks.
Without adequate treatment, these infections become chronic.
In the future, they can lead to complications, including infertility.
Therapy
Once the cause that provokes the appearance of a lump in the vagina has been established, as well as whether it belongs to the group of benign or malignant neoplasms, the doctor chooses appropriate therapy that will help get rid of the problem as quickly as possible.
Basically, all benign neoplasms occur without the occurrence of any symptoms, so they are constantly monitored. If growth prospects appear, surgical therapy is used and the tumor is excised. If the lump is located directly on the mucous layer of the vagina, it is simply removed from it.
In the presence of a malignant tumor formation, the main methods of treatment are surgery followed by radiation.
In addition, a woman may be prescribed drugs belonging to the group of antibiotics, which will help eliminate infectious and inflammatory processes, as well as prevent the development of complications. In combination with medicinal drugs, the use of antibacterial baths is recommended.
Tests for growths in the vagina
The doctor can identify some types of growths in the vagina after just one examination.
But in any case, tests are necessary.
They allow:
- establish the exact reason why a growth appeared in the vagina
- carry out differential diagnosis
- confirm the diagnosis, even if it was established after examination
- clarify the diagnosis (for example, determine the type of HPV when condylomas appear)
The tests allow you to choose the optimal therapeutic tactics and assess the risk of possible complications.
In addition, they give the doctor 100% confidence in the diagnosis.
What tests will be ordered depends on the clinical examination data.
Different pathologies are diagnosed in different ways.
To diagnose molluscum contagiosum, skin scraping with microscopic examination is used.
The doctor sees mollusc bodies in the sample.
They are inclusions in the cytoplasm of cells.
If condylomas are suspected, a test with acetic acid is first performed.
It allows you to differentiate condyloma from other formations.
Then PCR is performed.
The material used is skin scraping.
PCR allows you to find out which type of HPV caused growths in the vagina.
This is important for determining prognosis and therapeutic tactics.
Because some types of viruses are not dangerous.
While others can cause cancer.
If highly oncogenic types of HPV are detected, the woman is placed under dynamic observation.
She comes to the doctor for examination every six months as long as the papillomavirus is in her body.
If sexually transmitted infections are suspected, PCR is performed.
Smears from the urethra and vagina are used as clinical material.
Thanks to PCR, it is possible to identify any pathogens, including herpes, chlamydia, and gonorrhea.
In the case of a nonspecific infectious process, a tank is cultured.
Antibiotic sensitivity is determined.
Antibacterial treatment may be prescribed even before test results are received.
But in the future the doctor may change the regimen.
Cytological picture of the vagina
Rice.
11. The first type - basal cells and leukocytes in the smear, characterizing severe estrogen deficiency. Rice. 12. The second type - in the smear there are basal and intermediate cells, as well as leukocytes - significant estrogen deficiency. Rice. 13. The third type - intermediate cells predominate in the smear, a small number of superficial non-keratinizing cells - moderate estrogen deficiency. Rice. 14. The fourth type - only keratinizing cells in the smear - high estrogen content. V.'s epithelium undergoes changes depending on the phases of the menstrual cycle. The cellular composition of vaginal contents is biol, a test of the hormonal influence of the gonads. In the contents of the V. there are three main types of epithelial cells: superficial, intermediate and basal. Superficial cells are divided into keratinizing and non-keratinizing. In addition to basal cells, parabasal cells are also isolated. The cells of the surface layer of the epithelium have relatively large sizes, weakly stained cytoplasm, and a pyknotic nucleus. The detection of these cells indicates the follicular phase of the menstrual cycle. Intermediate cells from the superficial part of the spinous layer are smaller in size, have a larger nucleus, and can be present in smears in all phases of the menstrual cycle, but mainly in the luteal phase. Basal cells, the source of which is the inner section of the stratum spinosum, are small in size with relatively large nuclei. They occur with ovarian hypofunction, in menopause. With polychrome staining of smears, it is possible to determine the ratio between the number of acidophilic and basophilic cells. Estrogens increase the number of acidophilic cells in vaginal smears, progesterone causes an increase in the number of cells with basophilic cytoplasm. To determine cytol. V.'s pictures are subjected to cytological examination (see). In practice, it is customary to distinguish four types of vaginal smears (cytol. reactions), characterizing the content of estrogen in the body. (color fig. 11-14). The first type is characterized by the presence of basal cells and leukocytes; it is a manifestation of a severe estrogen deficiency in the body. In the second type, basal and intermediate cells and leukocytes are found in the smear. Such a cytol. the picture indicates significant estrogen deficiency. The third type is characterized by a predominance of intermediate cells in the smear and a small number of superficial, non-keratinizing cells, which indicates moderate estrogen deficiency. In the fourth type, keratinizing cells are found in the smear; parabasal cells and leukocytes are absent. This reaction is characteristic of a high estrogen content in a woman’s body. See also Gynecological examination, Rectal examination (in gynecology).
Growths in the vagina: drugs and treatment regimens
For different pathologies, different treatments are used.
In most cases, growths in the vagina can be removed using conservative therapy.
For herpes, acyclovir is prescribed.
For nonspecific inflammations or bacterial STDs - antibiotics.
For pediculosis pubis, treatment with permethrin is prescribed.
For some viral diseases, such as molluscum contagiosum and condylomas, there are no specific drugs.
Therefore, treatment regimens consisting of immunomodulators and general antiviral drugs are used.
They help reduce the viral load.
As a result, there is a possibility that the growths will disappear.
Although in most cases they have to be removed by laser or electrocoagulation.
Then immunomodulators are prescribed only to prevent the re-formation of rash elements.
Should my partner be treated?
Most growths in the vagina appear as a result of infectious causes.
It could be herpes, papillomavirus, molluscum contagiosum, etc.
Therefore, in such cases, the sexual partner most likely has the same disease.
He needs to be treated at the same time as the woman.
Otherwise, re-infection will likely occur in the future.
And then all the results of treatment will go down the drain.
In some cases, there is no need to treat your partner.
After all, growths can be caused by mechanical injuries, allergies, burns, and nonspecific inflammations.
Such pathologies are not contagious.
Similar diseases are unlikely to be detected in a partner.
Malignant formations: varieties
There are several classifications of vaginal cancer. Malignant tumors of the vagina differ in histological structure, growth pattern, and stage. Depending on the type of cancer, the prognosis and treatment tactics are determined. According to histology, malignant tumors in the vagina are divided into the following options:
- Squamous formations. This type of cancer occurs in 95% of cases. Often it develops gradually against the background of precancerous processes. Most often, cancer is localized at the junction of the vagina and the cervix.
- Melanoma. This formation belongs to pigmented tumors. It is characterized by pronounced aggressiveness, rapid development and a tendency to metastasize. Often, melanoma grows into the vagina from the vulva. Less commonly, it is a primary tumor.
- Clear cell adenocarcinoma. Occurs in young women. Refers to DES-dependent tumors.
- Secondary adenocarcinomas. These neoplasms are metastases of tumors from other organs.
- Sarcoma. Often, this is a tumor of the vaginal wall. It can develop from smooth or striated muscles (found in young children).
- Germ cell tumor of the vagina. This histological variant of cancer is characterized by the fact that atypical cells are formed in the embryonic period from the gonads. It can occur at any age, most often in children.
Depending on the nature of growth, endo- and exophytic neoplasms are distinguished. The first ones develop in the wall of the organ. Exophytic cancer grows outward, that is, into the vaginal cavity. This variant is thought to be less likely to spread by hematogenous transmission (metastasize).
Complications with growths in the vagina
If left untreated, complications may occur.
Papillomavirus can cause cervical dysplasia.
In the future, it can develop into cancer.
With nonspecific inflammatory diseases, local and general complications are possible.
Local ones include the formation of an abscess or phlegmon.
Sometimes the abscess breaks into the blood, and then bacterial damage to other organs occurs.
With sexually transmitted infections, cases of infertility are common.
Reactive arthritis – inflammation of large joints – may develop.
To protect yourself from complications, consult a doctor in a timely manner and undergo a course of therapy.
Additional diagnostics
To establish the nature of the lump in the vaginal area, additional methods are required. The diagnostic process may include various techniques that help the doctor determine the cause of the formation. These include:
- General blood and urine tests.
- Blood biochemistry (antibodies to infections, tumor markers).
- Analysis of vaginal discharge (microscopy, bacterial culture, PCR).
- Smear for oncocytology.
- Colposcopy.
- Biopsy with histology.
Having received all the results, the specialist makes a final conclusion and can definitely say whether the woman should have worried. And taking into account the nature of the pathological process and the clinical situation, therapeutic measures will be taken and recommendations will be given that the patient must adhere to.
Diagnosis of benign vaginal neoplasms
Diagnosis is usually not difficult. Vaginal tumors are detected during a gynecological examination. During bimanual examination, tumors are palpated with clear boundaries, dense consistency, and limited mobility. Examination with a mirror allows you to examine the nodes located in the area of the anterior wall of the uterus. Vaginal tumors can grow to the size of a chicken egg. In this case, they can not only cause discomfort, but also lead to more serious consequences for the patient’s health.
Next, a transvaginal ultrasound is performed, which visualizes the structure of the tumor and determines its echogenicity.
To determine whether a tumor is malignant or benign, the patient is sent for histological examination. Additionally, a number of tests are carried out: tumor biopsy, colposcopy, PCR - diagnosis of oncogenic and non-oncogenic strains, cytological examination of a smear.
Early symptoms of vaginal cancer
At the beginning of its development, a cancerous tumor does not cause any alarming sensations, does not hurt, and is not visualized.
The earliest symptoms of vaginal cancer that a woman may notice are:
leucorrhoea;
- bloody discharge, possibly with signs of pus.
Among the first symptoms of vulvar cancer:
- itching and burning;
- the appearance of unpleasant-smelling discharge;
- pain in the perineum, sacrum, lower back;
- the formation of palpable seals and ulcers on the labia majora, as well as in the area of the vestibule of the vagina.
As the tumor grows, the clinical picture worsens and the signs become cancer-specific. For vaginal cancer, disturbances in the menstrual cycle are not typical. Cancer treatment abroad at this stage will be the most effective and gentle.