What is hysteroscopy
Hysteroscopy is a type of endoscopic examination used in gynecology. Using a special device (hysteroscope), the doctor examines the uterine cavity and, if necessary, performs some medical manipulations.
The image is transmitted to the screen, so several specialists can monitor the manipulation at once. The procedure is painful, so it must be performed under general anesthesia.
The procedure allows you to examine the uterine cavity and its appendages
Indications for use
Hysteroscopy is used to diagnose and treat many diseases of the reproductive system.
- Dysfunctional uterine bleeding, which may be associated with hyperplastic processes.
- Myomatous nodes in the uterus.
- The presence of synechiae in the uterine cavity after inflammatory processes and operations.
- Diagnosis of polyps and endometrial cancer.
- The presence of intrauterine septa leading to infertility.
- Pathology of the development of the uterus and its appendages.
- The presence of a dead fertilized egg or its remains in the uterine cavity - after an abortion or frozen pregnancy.
- Foreign body in the uterine cavity.
- Impossibility of removing the intrauterine device due to its adherence to the walls of the uterus.
- Diagnosis of uterine infertility.
- Therapeutic manipulations for hyperplastic processes of the endometrium.
There are many indications for hysteroscopy, so this procedure is performed quite often. Despite the fact that hysteroscopy is used to treat infertility, the manipulation itself is traumatic. After it, time is needed to restore a normally functioning endometrium, which will be able to accept the fertilized egg and securely attach it.
Material and methods
The work was carried out on the basis of the gynecological department of the Moscow Regional Research Institute of Obstetrics and Gynecology (MONIAG). For 2016—2019 We examined and operated on 19 women with ectopic pregnancy in the area of the uterine scar after cesarean section.
All patients underwent a complete clinical and laboratory examination.
Ultrasound examination was carried out on a VOLUSONE 10 GE and WS80A SAMSUNG MEDISON using a convex and vaginal sensor (transabdominal and transvaginal scanning) in the “gray scale” mode. To control the localization of the chorionic vasculature - using the color Doppler mapping mode. The tasks of ultrasound in the presence of pregnancy in the scar included its confirmation, clarification of the gestational age according to the coccygeal-parietal size of the embryo, determination of the presence of residual (residual) myometrium in the scar area, determination of signs of chorion ingrowth (the presence of a uterine hernia and bulging of chorionic tissue towards the bladder, changes in chorionic tissue in the form of lacunae), tentative determination of the degree of destructive changes in the myometrium, bladder wall and cervix.
Statistical processing of the research results was carried out using Microsoft Excel and Statistica programs.
How the procedure can help
Infertility can occur due to many reasons. They can be hormonal - when a woman’s body does not have enough hormones that are necessary to maintain pregnancy and preserve the fertilized egg. Infertility can also be caused by uterine factors:
- anomalies in the structure of the uterus itself - infantile, bicornuate, the presence of septa in its cavity;
- obstruction of the fallopian tubes - due to adhesions, fusion of their cavity or entrance to the tube;
- the presence of adhesions in the cavity of the uterus itself - the fertilized egg cannot penetrate it and gain a foothold in the endometrium;
- hyperplastic changes in the endometrium - the fertilized egg cannot attach to such mucosa.
Hysteroscopy can help remove these barriers to pregnancy. With an infantile or bicornuate uterus, the procedure can only help establish the diagnosis, but treatment is not possible. If there are partitions, they can be destroyed using a hysteroscope. The same applies to adhesive processes - any, even the densest synechiae can be destroyed and removed during this procedure.
The hysteroscope allows you to remove adhesions and endometrial polyps
You can also clean the cavity of the fallopian tubes. To eliminate their infection, pneumohysteroscopy is used - when the fallopian tubes are inflated with air and the adhesions are broken. For endometrial hyperplasia, complete curettage of the uterine cavity is performed, removing all the mucous membrane. After this, the woman is prescribed a course of hormonal therapy to restore normal endometrium.
Many women who have had the procedure note that it helped them get pregnant. Although before this, other methods of treating infertility were ineffective.
Currently, a significant increase in the frequency of surgical delivery both abroad and in Russia is alarming, since the desire to solve all obstetric issues through surgery has proven untenable. According to world literature [6], every fourth woman gives birth by cesarean section, and every fifth of them has complications in the postoperative period. The number of cases of caesarean section at the Moscow Regional Research Institute of Obstetrics and Gynecology (MONIIAG), which also concentrates patients with an operated uterus, was 23.7% in 2008, 24.9% in 2009 and 24.3% in 2010 The number of cesarean sections in the Moscow region varies from 17.7 to 20.6%, while there is a clear tendency to increase the number of surgical births both in the Moscow region as a whole and in certain areas, which accordingly entails an increase in the number postoperative complications.
According to MONIIAG [4], in the structure of complicated forms of purulent inflammation, postpartum complications consistently occupy second place, second only to complications arising from the use of intrauterine contraceptives; at the same time, complications after surgical delivery dominate in a ratio of 9:1. Postpartum purulent-inflammatory diseases are still one of the main causes of maternal morbidity and mortality. The most common manifestation of postpartum infection is endomyometritis, the number of cases of which after cesarean section reaches 20%. Postpartum endomyometritis is the leading cause of the formation of an incompetent scar on the uterus and the generalization of infection, and the basis for the formation of a successful scar is the adequacy of reparative processes in the area of the wound on the uterus. The course of healing processes is determined by a large number of factors. In case of inadequate perfusion of the wound zone, an area of critical tissue hypoxia is created with disruption of the vital activity of myometrial cells [1]. In such a situation, the first target for infection is the sutures on the uterus.
On the basis of the gynecological department of MONIIAG for 2006-2011. 104 patients with an incompetent uterine scar were examined and operated on: 83 postpartum women on various days after cesarean section against the background of endomyometritis of varying severity and 21 patients at the stage of pregravid preparation for subsequent pregnancy.
All patients underwent a comprehensive examination and intensive treatment with a mandatory surgical component. Treatment options varied depending on the severity of the disease:
Option 1 - conservative surgical treatment, in which the surgical component was hysteroscopy (removal of the pathological substrate and ligatures, washing of the uterine cavity with antiseptic solutions, active aspiration and drainage of the uterine cavity) - 24 (23.1%) patients;
2nd option - organ-saving surgical treatment - metroplasty was performed in 41 (39.4%) patients with an unfavorable obstetric history (loss of children during childbirth or their severe trauma), when, when the inflammatory process was stopped after conservative surgical treatment, a significant defect in the uterine wall remained, posing a real threat to its rupture during a subsequent pregnancy. The technical features of this operation were the following:
— careful mobilization of the anterior wall of the uterus and the posterior wall of the bladder;
— excision of all necrotic and destructive tissues of the lower uterine segment until reaching the unchanged areas of the myometrium, complete removal of the remnants of the old suture material;
- application of a single-row secondary suture to the uterus (muscular-muscular);
- the needle was injected, retreating 1-1.5 cm from the edge of the wound, the optimal distance between the sutures was 1-1.5 cm;
— subsequent closure of the area of secondary sutures was carried out using the posterior wall of the bladder or the vesicouterine fold, which were fixed to the serous cover of the uterus above the suture line on it with separate ligatures;
— only absorbable synthetic threads (vicryl, monocryl, polysorb) were used as suture material;
Option 3 - radical surgical treatment was undertaken by us in 18 (17.3%) postpartum women with progression or generalization of the inflammatory process [3].
Delayed metroplasty was performed in 21 (20.2%) patients when an incompetent scar on the uterus was identified at the stage of planning the next pregnancy (cesarean section in this group of patients was performed from 1 to 7 years ago, both as planned and for emergency indications ).
Treatment results: there were no deaths or complications. In 7 patients who underwent plastic surgery of the lower segment of the uterus, pregnancy occurred after 1-2.5 years, which ended in the birth of live, full-term children.
Based on the authors’ own experience in examining and treating patients with incompetent sutures or a scar on the uterus after cesarean section, the most significant risk factors for disruption of its formation are identified and the features of the clinical course of endomyometritis in modern conditions are presented.
Risk factors for the formation of an incompetent scar on the uterus after cesarean section
The most significant risk factors for the development of purulent-septic complications after cesarean section are the following:
- history of infectious and inflammatory obstetric and gynecological diseases - 100%;
— previous infertility — 22.6%;
- past or existing chronic diseases of the bronchopulmonary system - 30%;
— placenta previa in the incision during caesarean section — 40%;
— performing surgery in conditions of sharp thinning of the lower uterine segment — 23.6%;
— the presence of technical errors during the operation: the use of Gusakov’s technique, the use of rough manual techniques for removing the head, the use of a continuous suture for suturing the uterus, the use of reactogenic material, inadequate hemostasis; the duration of the operation is more than 2 hours, pathological blood loss.
Etiology of postpartum endomyometritis
Currently, the nature of pathogens causing postpartum complications has changed significantly - the proportion of microbial associations has increased, which significantly aggravates the course and complicates the treatment of postoperative purulent-septic complications. The leading role in the etiology of postpartum endomyometritis belongs to opportunistic microflora, in 80-90% of cases associations of aerobic and anaerobic non-spore-forming microorganisms that make up the normal microflora of the genital tract in women [8]. Potential pathogens include gram-positive (enterococci, Staphylococcus aureus and Staphylococcus epidermidis, streptococci of groups A, B, etc.) and gram-negative (Escherichia coli, Klebsiella, Proteus, Enterobacteriaceae, Pseudomonas aeruginosa) aerobic bacteria. Among anaerobic bacteria there are bacteroides, peptococci, and peptostreptococci. It has been established that the pathogenicity of anaerobes increases in the presence of facultative aerobic microorganisms, in particular Escherichia coli [1]. In mild forms of the disease, associations were identified in 29.1%, in severe forms - in 62.5% of patients.
Clinical course of postpartum endomyometritis
In typical cases, on the 3-5th day of the postpartum period, pain in the lower abdomen, hyperthermia appear, the size of the uterus significantly exceeds those corresponding to normal involution periods, the uterus is painful on palpation. Lochia is cloudy, sometimes bloody-purulent, with an odor. Signs of intoxication are either absent or moderate. In severe forms, general intoxication is pronounced. This is characterized by headache, weakness, tachycardia, chills, sleep disturbances, appetite disturbances, dry mouth, and intestinal paresis. In such patients, the uterus is enlarged, sharply painful on palpation, lochia is purulent, with an ichorous odor. Leukocytosis and increased ESR are characteristic.
However, in recent decades there have been significant changes in the clinical course of postpartum endomyometritis, associated, among other things, with a significant change in the contingent of pregnant women - the predominance of patients with various extragenital diseases, infertility, mixed viral-bacterial infection, those who have undergone IVF, patients with miscarriage, elderly primiparas. The irrational use of antibiotic prophylaxis and antibiotic therapy during pregnancy, childbirth and the postpartum period also plays a negative role.
Features of the clinical course of endomyometritis in modern conditions are:
— late clinical (sometimes after discharge from the hospital) manifestation of the disease;
- initially chronic course of the disease or the presence of a short “acute” phase of manifestation with a further “erased” clinical course;
— “erased” course of postpartum endomyometritis, often diagnosed as hemato- and lochiometra, uterine subinvolution [2];
— the predominance of infiltrative and necrotic forms of inflammation in the absence of typical clinical and laboratory signs of infection.
It should be noted that against the background of adequate treatment of postpartum endomyometritis, all symptoms of the disease should stop within 5-10 days, and the patient is discharged from the hospital, while the rehabilitation stage plays a huge role in preventing the process from becoming chronic in the future.
Prognostically unfavorable clinical symptoms indicating the progression of endomyometritis are:
- repeated increase in body temperature above 38 ° C after discontinuation of antibacterial therapy;
- lack of tendency to form the cervix;
- presence of hematomas or infiltrates in the retrovesical space, parametriums; abscesses in the abdominal cavity and pelvis;
- presence of transient symptoms of intestinal paresis;
- progression of sluggish endomyometritis, which does not stop even with adequate therapy, against the background of which the formation of partial or complete failure of the suture on the uterus occurs - the leading, and sometimes the only clinical symptom of septic postpartum complications;
- undulating course of the process (acute stage - remission), with each stage of exacerbation (in which further complications occur) in clinical manifestations and consequences more severe than the previous one, each stage of remission is shorter and shorter;
— leukocytosis as the main marker of the purulent process is observed only in 1/3 of patients. More typical are a sharp increase in ESR (up to 60 mm/h and above), a decrease in hemoglobin levels (up to 80 g/l and below) and lymphopenia. Leukopenia is a poor prognostic sign, indicating the generalization of the inflammatory process.
The presence of such a symptom complex indicates various options for the progression or even generalization of the infection and the vital need for surgical treatment (see figure).
Figure 1. Variants of the course and outcomes of postpartum endomyometritis.
Methods for examining the uterus after cesarean section
Ultrasonography
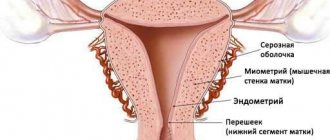
The complex ultrasound algorithm includes two-dimensional echography of the uterus, color Doppler mapping, pulsed Doppler ultrasound of the arcuate arteries of the uterus, three-dimensional echography of the uterus with determination of the volumes of its body, cavity and cervix [7].
Doppler indicators of blood flow in the area of sutures on the uterus during the normal course of puerperia:
— 3rd day — color loci are not determined during energy mapping (minimum blood flow speed in the device settings);
- 3-5 days - there are single color loci along the periphery and in the structure of the myometrium between the ligatures;
- 5-7 days - vascularization in the suture area exceeds vascularization in the surrounding myometrium.
The most significant indicators of the normal state of sutures on the uterus after cesarean section are the volume of the myometrium in the area of sutures on the uterus and the vascularization index (VI) [9].
Subinvolution of the uterus, regardless of the method of delivery, is characterized by arterial hyperemia of the uterus - an early manifestation of vascular disorders in response to inflammation. Postpartum women with uterine subinvolution are at risk of developing hematolochiometra due to decreased myometrial contractility and insufficient thrombosis of the spiral arteries after separation of the placenta.
Hematolochiometra, regardless of the method of delivery, is characterized by an increase in the volume of the uterine cavity by 2.3-3.3 times and quantitative indicators of three-dimensional power Dopplerography (VI, filtration index - FI) by 61 and 48% relative to similar indicators in the physiological course of puerperia.
Subclinical and early forms of postpartum endomyometritis are characterized by a significant increase in vascular resistance indices - systolic-diastolic ratio (S/D) and resistance index (IR) both on the side of the placental bed and on the opposite side of the uterus after spontaneous birth by 33 and 20%, after cesarean sections - by 29 and 40%, respectively, in combination with a decrease in three-dimensional quantitative indicators of blood flow (VI, FI) by 1.9-2.2 and 1.6-1.7 times, respectively. The identified changes reflect the presence of pronounced discoordinated disorders of the vascular network of the uterus during the complicated course of the postpartum period.
Changes in three-dimensional power Doppler ultrasonography in the area of sutures on the uterus after cesarean section during a complicated course of the postpartum period (subinvolution of the uterus, hematolochiometra, endomyometritis) are significantly more pronounced than in the entire vascular network of the uterus, i.e. the suture area on the uterus is the primary link in the development of the inflammatory process [9].
The main ultrasound signs indicating the presence of endomyometritis and disruption of repair processes in the area of sutures or scar on the uterus:
- subinvolution of the uterus;
- enlargement and expansion of the uterine cavity;
- the presence in the uterine cavity of inclusions of various sizes and echogenicity (intracavitary serous fluid, pus); the presence on the walls of the uterus of linear echo-positive structures (in the form of an intermittent or continuous contour), reflecting the application of fibrin;
— heterogeneity of the myometrium in the area of sutures or scars, the anterior and posterior walls of the uterus;
- local change in the structure of the myometrium in the area of sutures in the form of areas of reduced echogenicity in the form of a “butterfly” or “cone” (infiltration zone);
- local circulatory disorder in the scar area, expressed in a decrease in volumetric blood flow and an increase in vascular resistance indices.
The main ultrasound criteria characteristic of patients with failed sutures or a scar on the uterus are deformation of the uterine cavity in the area of the sutures, the presence of local retraction, and visualization of a “niche” in the area of the postoperative scar.
Hysteroscopy
If clinical and/or ultrasound signs of postpartum endomyometritis or incompetent sutures on the uterus are detected, therapeutic and diagnostic hysteroscopy is indicated [5, 10]. It must be performed on all obstetric patients with endomyometritis, and the earlier this intervention is undertaken (for diagnostic or therapeutic purposes), the better the outcome of the disease and prognosis.
The hysteroscopic picture of endomyometritis is characterized by expansion of the uterine cavity; an increase in the length of the uterine cavity that does not correspond to that during normal postpartum involution; presence of turbid wash waters; the presence of fibrinous deposits not only in the placental area, but also in other parts of the uterus, including in the area of sutures; the presence of synechiae in the uterine cavity.
Hysteroscopy makes it possible to identify and differentially treat patients with different forms of postpartum endomyometritis.
Forms of endomyometritis detected during hysteroscopy:
— fibrinous endomyometritis: the hysteroscopic picture is characterized by the presence of a whitish coating on the walls of the uterus, most pronounced in the area of the placental site and the area of sutures on the uterus, as well as fibrin flakes in the washing waters (the “blizzard” picture);
- purulent endomyometritis: the uterine cavity contains pus, the endometrium is loose, pale in color, looks like a honeycomb, from which pus “oozes”; rinsing water is cloudy and has an odor;
- endomyometritis with necrosis of decidual tissue: the presence of a small amount of hemorrhagic “ichorous” fluid in the uterine cavity is typical; dark or black areas of the endometrium are identified, sharply contrasting with the rest of the endometrial surface; necrotic forms of endomyometritis are especially difficult for clinical and ultrasound diagnostics and are detected only during hysteroscopy;
— endomyometritis with retained placental tissue differs from those described above by the presence in the area of the placental site of a bluish-colored, spongy-looking mass formation hanging into the uterine cavity.
The following signs indicate the failure of the sutures on the uterus during hysteroscopy against the background of endomyometritis:
- swelling and bending of the uterus in the area of the sutures and, as a consequence, lochio- or pyometra;
— presence of gas bubbles in the area of the seam defect;
- sagging ligatures, hanging knots into the uterine cavity, free presence of threads in the uterine cavity and lavage waters;
- identification of dark or black areas of the endometrium in the area of sutures on the uterus, sharply contrasting with the rest of the endometrial surface (a poor prognostic sign, indicating irreversible purulent-necrotic changes in the lower uterine segment, resulting from necrobiotic inflammation - anaerobic or putrefactive flora;
— visualization of the defect of postoperative sutures in the form of a “niche”, i.e. funnel-shaped “retraction” of various sizes and depths. As a rule, the defect area is always “covered”, i.e. delimited from the free abdominal cavity by the posterior wall of the bladder and the vesicouterine fold;
— determination of the formed fistula tract (with uterovesical fistulas).
Diagnosis of uterine scar failure in the delayed period
In recent years, the problem of identifying an incompetent scar on the uterus in the delayed period has increasingly arisen, more often at the stage of planning the next pregnancy.
Ultrasound criteria for uterine scar failure:
- atypical location of the scar;
- deformation of the outer contour of the uterus at the level of the isthmus or in another place in the scar zone;
- retraction of the serous membrane;
— the presence of destructive changes in the scar zone with the formation of cavities in the myometrium;
— thinning of the myometrium, visualization of niches and deformations in the projection of the scar with thinning of the myometrium up to 4-5 mm;
- the presence of a “niche” or “niches” on the side of the uterine cavity, a sharp thinning of the myometrium in the scar zone up to 2-3 mm (critical values) or the absence of myometrium in the scar zone - complete failure of the scar;
- retraction of echogenic tissue from the side of the serous membrane in the form of strands and vague fields of irregular shape without clear boundaries;
— lack of convincing vascularization of the myometrium in the scar zone during energy mapping.
In some cases, it is advisable to use hydrosonography to clarify the diagnosis [1]. The quality of visual assessment of pathology is improved by creating the effect of an “acoustic window” in the uterine cavity. With hydrosonography, the localization of the scar relative to the internal os and uterine angles is more clearly determined, and the thickness of the myometrium to the serous cover of the uterus is assessed. The sensitivity of hydrosonography in diagnosing an incompetent uterine scar at the stage of pregnancy planning reaches 100%.
It is advisable to use office hysteroscopy to clarify the diagnosis of an incompetent scar on the uterus at the stage of pregnancy planning.
It should be noted that the diagnosis of an incompetent scar on the uterus is always complex and ambiguous, especially in the delayed period, at the stage of pregnancy planning. It is advisable to verify the diagnosis in all cases during a consultative examination, using ultrasound, hydrosonography and hysteroscopy.
Thus, the outcome of severe forms of endomyometritis after cesarean section is influenced by the timeliness and quality (adequacy) of diagnostic measures and drug treatment (the average duration of the disease in patients after childbirth before the onset of severe complications is 15 days), as well as the timeliness of the use of surgical aids (hysteroscopy, metroplasty , hysterectomy).
Timely diagnosis of postpartum endomyometritis and failure of sutures or scar on the uterus after cesarean section and early use of modern diagnostic and surgical measures make it possible in most cases to preserve reproductive function even in the most difficult clinical situations.
Complications and consequences
This procedure refers to surgical interventions. Its implementation is fraught with a number of complications. They can depend on the surgeons and on the woman’s body. What are the possible complications of hysteroscopy:
- perforation of the uterine wall;
- development of uterine bleeding - in some cases it is not possible to stop it and the uterus has to be removed;
- ingress of microbial flora and development of suppurative processes;
- Trauma to the mucosa can lead to the formation of adhesions.
Such consequences are quite rare. To prevent them, the following measures are taken:
- use of antibacterial drugs during and immediately after the procedure;
- visual control of the procedure;
- the presence of an anesthesiologist and surgeon in case of bleeding or perforation of the uterine wall;
- hormonal and resorption therapy to prevent adhesions and restore normal mucosa.
results
The average age of the patients was 31.2 years. When analyzing gynecological diseases in patients of the main group, endometriosis of various localizations was most often encountered (31.6%) (hereinafter the % is calculated arbitrarily, since the number of observations is less than 20), in 10.5% of cases - diseases of the cervix, in 5. 3% - uterine fibroids. A history of artificial abortion was observed in every fourth woman, non-developing pregnancy in every fifth, spontaneous miscarriages in 10.6% of patients. Including curettage of the walls of the uterine cavity for the above conditions was performed in 21.1% of patients in the period from 2 to 5 years after abdominal delivery.
5 (26.3%) patients had a history of abdominal delivery performed in a planned manner, and 14 (73.7%) patients had an emergency delivery at an average gestational age of 38 weeks. One operative delivery was observed in less than 1/2 of the observations, while two or more - in more than half of the observations. Indications for abdominal delivery in 36.8% of cases were an incompetent scar on the uterus, in 26.4% of patients - indications from the fetus, in 15.8% - a clinically narrow pelvis, in 5.3% of patients - anomalies of labor. Complications of the postpartum period followed by hospitalization in gynecological hospitals occurred in 10.5% of patients.
When contacting the outpatient department of the State Budgetary Healthcare Institution MO MONIIAG, the time frame for diagnosing ectopic pregnancy in the rumen was as follows: 6-7 weeks - in 7 (36.84%) pregnant women; 9-10 weeks - in 10 (52.63%); 13 weeks - in 2 (10.53%) patients. Progressive pregnancy was observed in 13 (68.4%) women, non-developing pregnancy - in 6 observations (31.6%). In 2 (10.5%) patients with a gestation period of up to 7 weeks, a typical localization of the ovum in the “niche” projection, isthmocele, was detected; there were no signs of uterine scar failure; the thickness of the residual myometrium ranged from 3 to 5 mm (Fig. 1) .
Rice. 1. Pregnancy in a scar without signs of its failure.
The arrows indicate: 1 - fertilized egg; 2 - preserved myometrium.
Taking into account the technical capabilities, the patients were planned to undergo vacuum aspiration of the fetal egg under the control of an ultrasound examination with a decision on the need for metroplasty in the long-term period.
In 14 (73.7%) patients with a typical localization of the ovum in the projection of the scar after cesarean section, thinning of the myometrium of the anterior wall with a residual myometrial thickness of less than 2 mm, deformation of the anterior wall of the uterus, and “bulging” of the ovum towards the bladder were revealed (Fig. 2) . In two cases there were signs of chorion invasion into the myometrium (Fig. 3) . Taking into account the high risk of gestational complications such as placenta accreta, bleeding, and uterine rupture, pregnant women were offered termination of pregnancy with simultaneous metroplasty.
Rice. 2 Pregnancy in a scar with signs of its incompetence, thinning of the myometrium.
1 - fertilized egg; arrows indicate residual myometrium.
Rice. 3. Pregnancy in a scar with signs of its incompetence, invasion of the chorion into the myometrium, high risk of placenta accreta.
1 - chorion; arrows indicate residual myometrium.
In 3 (15.8%) patients during initial treatment at 10 weeks of pregnancy (1 pregnant woman) and 13 weeks (2 patients) with a non-developing pregnancy, signs of chorion ingrowth with total destruction of the lower third of the anterior wall of the uterus, the isthmus and partly the upper third of the anterior wall were noted. lips of the cervix with signs of chorion invasion into the bladder wall (Fig. 4) . Attempts at metroplasty in this situation were intraoperatively complicated by bleeding; for health reasons, the scope of the operation was expanded to hysterectomy.
Rice. 4. Total destruction of the anterior wall of the uterus in the scar area, partial destruction of the anterior lip of the cervix during pregnancy in the scar.
1 - posterior lip of the cervix; 2 - anterior lip of the cervix; between the arrows is the destruction zone.
All patients underwent surgical treatment. The priority in choosing surgical correction was the possibility of performing organ-preserving surgery with restoration of fertility. Metroplasty with simultaneous termination of pregnancy by vacuum aspiration of the fetal egg during surgery (see table) was performed in 14 (73.7%) patients; in two (10.5%) cases, vacuum aspiration of the fetal egg was performed under ultrasound control without metroplasty. And three (15.8%) patients underwent radical surgery due to the lack of technical capabilities to preserve the uterus.
Table. Scope of surgical treatment of examined patients
| Surgical intervention | Quantity | Gestation period, weeks | |
| abs. | % | ||
| Metroplasty with simultaneous termination of pregnancy | 14 | 73,7 | from 6 to 10 |
| Vacuum aspiration under ultrasound control | 2 | 10,5 | 6—7 |
| Radical operation | 3 | 15,8 | 13 and 10 |
When can you plan a pregnancy?
So, when can you get pregnant after hysteroscopy? This question worries all women who have undergone such a procedure.
The period when you can plan a pregnancy depends on the indication for which the procedure was performed. If it was done to clarify the diagnosis or exclude other diseases, no traumatic manipulations were performed - pregnancy occurs almost immediately and no special preparation is required for it. The optimal period for pregnancy after diagnostic hysteroscopy is considered to be an interval of 3–5 months.
If adhesions were removed or the endometrium was scraped, pregnancy cannot occur quickly. Getting pregnant becomes possible only after a full-fledged endometrium is formed. How long this will take depends on the woman’s body. On average, with hormonal therapy, the endometrium grows within six months. If after the procedure adhesions form again, the period increases for several more months until they are removed again.
Pregnancy can be planned when a normal endometrium is formed
There is no point in trying to get pregnant quickly after such a procedure. It is necessary to wait for a complete recovery and carefully prepare for pregnancy so that it proceeds physiologically and is not complicated in any way.
Reviews
Irina, 24 years old. I couldn't get pregnant for two years. Doctors discovered multiple polyps in the uterus. They recommended performing a hysteroscopy and removing polyps. After the operation I had to take hormonal medications for some time. But six months later the long-awaited pregnancy came.
Anna, 36 years old. After several ectopic pregnancies, adhesions formed in the tubes. Doctors recommended doing a hysteroscopy to try to remove them. The operation was performed under general anesthesia. Removal of adhesions was successful, and the endometrium was restored for several months. After this I managed to get pregnant.