Anomalies of the uterus and vagina are observed in 4.3-6.7% of all women of childbearing age. They cause infertility in every eighth case, and in 12.6-18.2% they cause recurrent miscarriage, placental abruption, abnormal fetal position and other complications.
One of the most common anomalies of the uterus is its infantility (also called hypoplasia) - a defect associated with the small size of the main reproductive organ. With a slight decrease in the size of the uterus, the anomaly does not manifest itself with any symptoms, but a significant degree of hypoplasia can be suspected even in adolescence - by the late appearance and extreme pain of menstruation.
Classification of uterine hypoplasia
The uterus is considered underdeveloped if, by a certain age of the patient, its size is smaller than it should be, according to normal physiology.
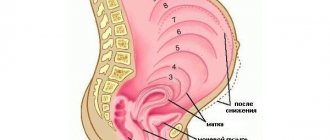
Depending on when the organ stopped developing, 3 degrees of uterine hypoplasia are considered:
- Hypoplasia of the uterus 1 degree. The organ is called "embryo" or "vestigial". In this case, the size of the uterus is no more than three and a half centimeters. Moreover, most of the length with hypoplasia is the cervix. This anomaly is formed during the intrauterine development of the embryo.
- Hypoplasia of the uterus 2 degrees. The size of the organ can reach five and a half centimeters, and the proportions of the cervix and body are three to one. The organ is called infantile or childish.
- Hypoplasia of the uterus 3 degrees. The “teenage” uterus reaches seven centimeters, having a normal ratio of the cervix to the body of the organ.
Based on the degree of underdevelopment of the organ, the manifestations of the pathology also differ. Hypoplasia of the endometrium of the uterus is also found - in this case, the mucous layer of the organ becomes thinner (normally it is 7 mm). This type of underdevelopment is the easiest to treat.
Degrees of the disease
In gynecology, there are 3 degrees of this pathology.
First
Hypoplasia of the uterus of the 1st degree is also called germinal, fetal or rudimentary. The dimensions of the female organ do not exceed 3 cm and the cervix makes up most of it. A girl with this problem does not have menstruation and is unlikely to become pregnant.
But if the appendages function normally, then you can resort to IVF and further carrying the baby by a surrogate mother.
Second
Gynecologists place grade 2 when the length of the uterus is from 3 to 5.5 cm. This pathology is called childish or infantile. In girls with this problem, menstruation begins late, is painful, and the cycle is long.
Third
This degree of the disease is considered mild. The length of the uterus is 5-7 cm. This pathology can disappear with age or be easily cured. After this, the woman can become pregnant, carry and give birth to a child.
Causes of uterine hypoplasia
There are many reasons that contribute to the underdevelopment of the organ.
Congenital pathology can result from a negative impact on the maternal body during the intrauterine formation of the fetus. A hereditary factor can also cause pathology. Chromosomal and genetic abnormalities, bad habits of the expectant mother while carrying a child, delayed development inside the womb and infections that the mother carries during gestation - all this can negatively affect the child, contributing to the weak formation of the uterus. Also, the uterus may develop poorly due to taking medications that are not recommended during pregnancy.
The pathology may be acquired and occur due to:
- disorders in the hypothalamic-pituitary system (due to trauma to the body, exposure to toxic substances or infectious agents);
- tumors of the pituitary gland or hypothalamus;
- frequent, severe infectious and viral diseases;
- chronic pathologies of vital organs and systems;
- endocrine and autoimmune pathological processes;
- hormonal disorders after illness;
- insufficient formation of the ovaries (in this case, hypoplasia of the uterus and ovaries is diagnosed);
- underweight (due to malnutrition and weight loss diets);
- hypo- and vitamin deficiency (acute lack of vitamins);
- frequent stressful situations, nervous disorders and depression;
- surgical interventions on the ovaries (their removal or damage);
- bad habits (alcoholism, smoking, drug use);
- increased sports and mental stress on the body;
- frequent colds.
Causes and degrees of uterine hypoplasia
Congenital uterine hypoplasia is a manifestation of genital or general infantilism due to a damaging effect on the embryo in the antenatal period or hereditary factors. More often, the causes of uterine hypoplasia lie in violations of the “hypothalamus-uterus” regulatory system or ovarian failure with increased gonadotropic activity of the pituitary gland. Such regulatory failures occur in girls in childhood or puberty and can develop due to hypovitaminosis, intoxication (drug, nicotine), nervous disorders, increased educational and sports loads on the child’s body, anorexia, frequent infections (tonsillitis, ARVI, influenza), etc. etc. In this case, there is a delay in the development of the initially correctly formed uterus.
The main characteristic of uterine hypoplasia is a decrease in its size. Normally, in sexually mature nulliparous women, the uterus has a cavity length of at least 7 cm, in women who have given birth - 8 cm, the length of the cervix is 2.5 cm. Depending on the time of arrest of development, gynecology distinguishes three degrees of uterine hypoplasia: embryonic, formed in utero; infantile and adolescent, formed after birth. The embryonic (fetal) uterus is characterized by a length of up to 3 cm, the cavity is practically not formed, the entire size falls on the cervix. The infantile (children's) uterus has a length from 3 cm to 5.5 cm with a ratio of the length of the cervix to its cavity of 3:1. The teenage uterus with hypoplasia has a length from 5.5 cm to 7 cm, with a less pronounced predominance of the cervix - 1:3.
Symptoms of uterine hypoplasia
Girls with pathology are characterized by menstrual cycle disorders. The presence of pathology can be suspected even in adolescence, due to the late onset of menarche (after sixteen years) or its complete absence. In patients with grade 1 uterine hypoplasia, there are no periods at all, or menstrual flow is very slight and infrequent. With grades 2 and 3 of uterine hypoplasia, irregular time intervals are observed between menstruation; the amount of menstrual blood released can be either very abundant or completely insignificant.
Often, menstruation is accompanied by severe pain in the lower abdomen, nausea, headache and weakness, including loss of consciousness.
The pathology is characterized by signs of insufficient physical development:
- short stature;
- excessive thinness;
- narrow pelvis;
- poorly formed breasts.
Uterine hypoplasia and pregnancy
After a girl hears the “diagnosis of hypoplasia” of the uterus, “is it possible to get pregnant with such a disease” is her first question.
The development and presence of consequences of the disease are associated with the degree of development of the disease, the time of contacting the doctor and the correctness of treatment. The second and third stages of the disease are reversible. With the right approach, stage 3 treatment does not take much time. After reaching the normal size of the uterus, it becomes possible to conceive, as well as the happy birth of a child. Treatment of the disease in the second stage is a more complex process that takes a lot of time and effort. Even despite long-term treatment, pregnancy may not occur. Hypoplasia of the uterus of the 1st degree almost always excludes conception and bearing a child. With the right approach to treatment, in vitro fertilization is possible, that is, the use of the services of a surrogate mother.
Diagnosis of uterine hypoplasia
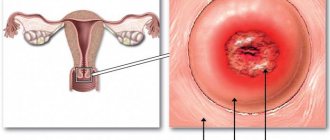
To diagnose pathology, it is first necessary to interview the patient and examine her in a gynecological chair. The doctor may notice weak hair growth in the pubic area, poorly developed labia, and the clitoris may protrude beyond the vulva. The vagina, in comparison with a normally developed one, is narrow and short, the body of the uterus is small, dense and very strongly tilted forward.
To find out the degree of uterine hypoplasia, an ultrasound is prescribed. Hysterosalpingoscopy using X-ray or ultrasound confirms uterine underdevelopment, weak formation of the ovaries and fallopian tubes.
The level of sex and thyroid hormones in the patient’s body is analyzed. The following types of research are periodically used:
- probing of the uterine cavity;
- determination of bone age using an x-ray of the hand;
- magnetic resonance imaging of the brain;
- X-ray of the skull;
- measurement of the pelvic area.
Diagnosis of uterine hypoplasia
A gynecological examination of patients with uterine hypoplasia reveals signs of genital infantilism: insufficient hair growth, underdeveloped labia, and the head of the clitoris protruding beyond the vulva. Vaginal examination reveals a short, narrow vagina with weakly defined vaults, elongation and conical shape of the cervix, reduction and flattening of the uterine body, hyperanteflexia. During a pelvic ultrasound, the dimensions of the body and cervix are examined, which allows us to judge the degree of uterine hypoplasia.
X-ray or ultrasound hysterosalpingoscopy confirms the reduced size of the uterus, tortuosity of the fallopian tubes, and ovarian hypoplasia. If uterine hypoplasia is suspected, a laboratory study of the level of sex hormones (FSH, progesterone, prolactin, LH, estradiol, testosterone), as well as thyroid hormones (TSH, T4), is performed. Additionally, if uterine hypoplasia is suspected, they resort to probing of the uterine cavity, determining the patient’s bone age, radiography of the sella turcica, and MRI of the brain.
Treatment of uterine hypoplasia
Therapy for pathology directly depends on when and for what reasons the pathological process began. It is necessary to adjust the diet; the patient’s food must contain the required amount of vitamins and minerals, be rich in carbohydrates, proteins and fats. It is important to minimize stressful situations and avoid depression.
Hormone therapy (both replacement and stimulating) is the basis for the treatment of pathology. Properly selected medications (selected individually by a specialist based on the general clinical picture and test results) and their correct administration (following the dosage regimen and dosages of medications) can not only restore the menstrual cycle, but also enlarge the uterus to normal size. Hypoplasia of the endometrium of the uterus is easier to treat than underdevelopment of the uterine body.
Physiotherapy will help restore uterine circulation:
- reflexology (acupuncture);
- treatment with ozokerite and paraffin;
- ultra-high frequency electric field treatment;
- application of high-frequency magnetic field;
- laser therapy;
- mud therapy;
- gynecological massage;
- Healing Fitness.
Visiting resorts is also useful - sea swimming and baths with sea water.
Causes
Normal, physiological sizes of the uterus are considered to be those at which:
- The length is 70 millimeters.
- The width is 40 millimeters.
- The length is 20-30 millimeters.
Doctors allow slight errors in sizes, as they depend on many factors. For example, the number of pregnancies, the outcome of childbirth and the method of delivery. With a significantly reduced size, we can talk about the underdevelopment of the uterus, its infantilism. Increased size may indicate pregnancy, the presence of neoplasms and inflammatory processes.
Reduced size of the uterus may be due to congenital pathology. Its occurrence was influenced by the lifestyle and health status of the mother at that time. More likely it is:
- Bad habits.
- Use of medications.
- Neuroses and psychological disorders.
- Endocrine and hormonal disorders.
- Lack of vitamins and macro-, microelements.
- Genetic factor in the mother.
Similar reasons may explain acquired underdevelopment of the uterus. These may also include:
- Heavy physical activity.
- Prolonged neuroses and depression.
- Anorexia and poor diet.
- Infectious diseases and stable colds.
Moreover, uterine hypoplasia develops precisely in childhood and adolescence. It is not acquired after the body's systems have stopped growing. Therefore, gynecologists recommend monitoring the health of girls in order to take timely measures if complications arise.
Is it possible to get pregnant with uterine hypoplasia?
With the germinal type of pathology, pregnancy is excluded, and becoming a mother is possible only with the help of assisted reproductive technologies. If it is impossible to get pregnant on your own, but the ovaries are functioning normally, then they resort to IVF (in vitro fertilization), using the patient’s egg. If a woman develops miscarriage syndrome, they resort to surrogacy. With uterine hypoplasia, you can get pregnant if the ovaries are fully formed and functioning normally, and the degree of uterine underdevelopment is small. It should be understood that pregnancy and labor with uterine hypoplasia can be difficult, with a high risk of abortion.
Treatment
Before prescribing a certain type of treatment, it is necessary to undergo a series of examinations. They allow you to determine the cause of the diagnosis, make it correctly and select adequate treatment.
Diagnostic methods include:
Gynecological examination.
The main method of treatment to enlarge the reproductive organ to normal size and restore the menstrual cycle is hormonal therapy. Other treatment methods can improve metabolism and blood circulation in the pelvic organs.
Additionally assigned:
- Vitamin therapy,
- Laser, magnetic therapy.
- Treatment with mud and paraffin.
- UHF therapy.
- Gynecological massage.
- Physiotherapy.
It is important to understand that with a diagnosis of stage 1 uterine hypoplasia, there is absolutely no chance of conceiving and carrying a child. The only option for women with this diagnosis is surrogacy. Especially if the ovaries produce eggs. With the other two types of pathology, the probability of conception and pregnancy is quite high.
However, the onset and carrying of pregnancy with a small uterus is always associated with great risk. It is caused by possible termination of pregnancy, complicated childbirth and its early onset. Therefore, experts strongly recommend planning a pregnancy with such a diagnosis, not remaining indifferent to their advice, attending routine examinations and promptly notifying about the presence of any alarming signs.
Prevention of uterine hypoplasia
In order to avoid pathology, it is necessary to eliminate the impact of negative factors on the mother’s body so that problems do not arise in the intrauterine development of the embryo. Negative effects on the body should be excluded even in adolescence. Exhausting diets should be excluded, as they contribute to acute hypovitaminosis and dysfunction of many organs and systems. Good nutrition, absence of stressful situations, normal physical activity and timely treatment of infectious diseases are the best preventive measures to prevent uterine hyperplasia. Regular (twice a year) gynecological examinations and prevention of the development of various diseases are the key to the health of mother and child.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: Date of publication: 09/29/2018
Gynecologists - search service and appointment with gynecologists in Moscow