Postpartum endometritis
As you know, endometritis (inflammation of the mucous membranes of the uterus) is one of the most common complications that most women have to face during the postpartum period. 7% of women in labor experience this disease, mostly women who have had a cesarean section.
After childbirth, the uterus is a large wound. There are two stages of its healing : inflammation and restoration of the mucous membrane.
Thanks to these stages, the uterus is cleansed inside. But if any pathogenic microorganisms are present, the inflammation can develop into chronic inflammation.
How to recognize?
There are severe endometritis , which can appear on the second to fourth day after birth, and mild endometritis , which can occur a little later.
In this case , the temperature rises to 38°C, the pulse quickens, the body shudders, pain occurs in the lower abdomen and lower back, which can intensify during breastfeeding.
Unpleasant brown discharge appears, which soon becomes purulent. With this disease, the uterus contracts more slowly than usual.
But elevated temperature (for example, 37.5°C) and weakness in the first days can be explained by the arrival of milk, and not by inflammation.
Prevention and treatment
Before giving birth (and preferably before pregnancy), it is imperative to identify and try to get rid of any infectious diseases.
In cases of high risk of endometritis and only as prescribed by a gynecologist, antibiotics may be taken for prevention purposes.
Treatment
Treatment of uterine inflammation after cesarean section presents some difficulties. This is due to the fact that in normal cases it should be performed with antibiotics. This is a fast and effective method of treating the inflammatory process. However, during pregnancy, the use of antibiotics may be limited due to the fact that the woman is breastfeeding. For this reason, doctors may try certain immune medications designed to boost immunity enough for the body to fight off infection on its own.
These are drugs such as Likopid, Interferon and others. However, the difficulty is that such drugs are not effective enough, and also that they may also have a contraindication such as breastfeeding. Some of these products can be used topically, for example, Viferon suppositories. But their activity is often not enough.
In this case, it is necessary to resolve the issue of stopping or interrupting breastfeeding for treatment, since the patient’s condition with such inflammation can be dangerous not only for her reproductive system, but also for life.
After stopping breastfeeding, broad-spectrum antibiotics, such as Amoxiclav, Tsiprolet, Ceftriaxone, Metronidazole, Doxycycline, can be freely prescribed. They are prescribed for a period of five days, and the dosage is calculated based on the patient’s weight. In parallel, non-steroidal anti-inflammatory drugs (Diclofenac) are prescribed, which help relieve inflammation and pain. Attention is paid to vitamin therapy, vitamin A, E, C and group B preparations are taken.
Pathological bleeding after childbirth
In fact, bleeding after childbirth cannot be called a symptom of pathology; this phenomenon is completely natural for this period.
After childbirth, the uterus spontaneously returns to its previous size. With such contractions of the uterus, blood is released from the vagina. This process of contraction is similar to heavy periods.
During the normal course, in the first week after birth they are abundant, have a thick consistency and a bright red color. After some time, they turn pale, become scarce and completely stop after one and a half to two months. When breastfeeding, such bleeding stops earlier, and for those who have had a cesarean section , on the contrary, it lasts a little longer.
But it also happens that the discharge becomes pathological.
How to recognize?
If the bleeding two weeks after birth is just as heavy, has a bright red color, has also acquired an unpleasant odor, and even worse has turned purulent, you should be wary.
All of the above may be the beginning of a developing complication that requires the help of a doctor.
Delayed postpartum bleeding is also dangerous This indicates a bending of the uterus or its slow contraction. In this case, there is an increase in temperature, heaviness in the abdomen, chills, and a significant decrease in discharge.
Preventive measures
Firstly , it is necessary to observe the following rules of genital hygiene: during bleeding and when there are stitches after childbirth, it is recommended to wash with cool, clean water every time after going to the toilet.
Secondly , sanitary pads should be changed preferably every four hours and not allowed to fit tightly during the first week.
The inflammatory process can be caused by microbes coming from the vagina or from the origin of a chronic infection inside the body.
Here are some useful tips to prevent abnormal bleeding:
- promptly cure all possible infections, in particular gynecological ones;
- do not use sanitary tampons;
- To make the uterus contract faster after childbirth, try to lie on your stomach more;
- go to the toilet on time;
- If the birth was successful, without complications, try to start moving as soon as possible.
Do I need a bandage after childbirth? Read here.
This section contains a lot of useful information that you need to know when planning a pregnancy.
Causes
In order to understand why, after childbirth, a woman’s reproductive system is most susceptible to various inflammatory and infectious processes, it is important to understand the very mechanics of the development of such a pathological phenomenon. Most inflammatory processes are bacterial in nature - that is, they are caused by pathological bacteria, less often by microorganisms. And very rarely - viruses and fungi. Moreover, any such process occurs in several stages:
- An infectious bacterial agent or microorganism enters the vagina;
- With insufficient tissue immunity, with insufficient density of the mucus plug and under some other circumstances, it penetrates from the vagina into the cervical canal, and from there into the uterine cavity;
- In most cases, the activity of such a pathological organism is suppressed by local tissue immunity, microflora and those beneficial bacteria that live on it;
- With weakened immunity (or with a large amount of infectious agent), such suppression is impossible;
- As a result, the pathological organism begins active activity, spreading both into the depths of the tissues and occupying larger and larger areas;
- Sooner or later, this causes negative symptoms characteristic of a particular disease;
- If the activity of bacteria is partially suppressed by general or local tissue immunity, then a chronic process is formed; if it is not suppressed, then it is acute.
Why is the risk of developing such a pathology especially high after pregnancy? This is due to several factors. First of all, because pregnancy is a huge stress for the body, which leads to a significant decrease in overall immunity. In addition, during childbirth, the uterine tissues are injured and their microflora is disrupted, as a result of which tissue immunity also drops significantly. Moreover, there are microtraumas that lead to the fact that the infectious agent is able to enter the blood immediately, which significantly complicates its suppression even with strong immunity.
During the birth process, there is a possibility of introducing bacteria into the reproductive system. And, taking into account all of the above, it becomes clear that in this case this will almost always lead to a pathological process. Moreover, the likelihood that inflammation of the uterus will develop after childbirth using cesarean section is higher than during natural birth. Since such surgical intervention leads to an even more significant decrease in immunity.
Abortions and miscarriages also have an impact on the likelihood of developing an inflammatory process in the uterus, since they also affect local tissue and general organic immunity. Therapeutic surgical and diagnostic interventions (curettage, hysteroscopy, etc.) can also reduce tissue immunity and lead to an increased likelihood of developing a pathological process. But it is childbirth in this sense that has the maximum negative effect.
There are different types of inflammation, and a variety of things can occur. However, after childbirth, the most common processes are those affecting the uterine cavity, and not the ovaries, fallopian tubes, etc. Since it is this area that is exposed to the most intense impact during childbirth. Pathological processes in the cervix and cervical canal are also very likely for the same reasons.
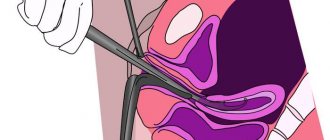
Chorioamnionitis (inflammation of the membranes of the fetus and uterus)
This complication occurs in the case of premature rupture of the membranes of the fetus.
And the longer the waterless period lasts, the greater the likelihood of infection of the fetus while it is still in the womb.
How to recognize?
Due to the long anhydrous period, which is from 6 to 12 hours, the woman in labor experiences: elevated temperature, rapid heartbeat, chills, and purulent discharge from the vagina.
Statistics show that in every fifth woman after childbirth, chorioamnionitis can develop into endometritis.
Treatment of chorioamnionitis
If chorioamnionitis occurs, urgent stimulation of labor is performed (in case of lack of strength during childbirth, a caesarean section) using antibacterial and infusion therapy.
Postpartum mastitis (inflammation of the mammary glands) and lactostasis (milk stagnation)
This disease can only affect nursing mothers. The causative agent is Staphylococcus aureus.
It can be infected through cracks in the nipples (unlike mastitis, lactostasis progresses without the presence of cracks).
Basically, mastitis appears in those who give birth for the first time (in 2-5% of cases); it can begin either in the third week after birth or a month later.
How to recognize?
Postpartum mastitis occurs with elevated temperature (up to 38.5°C and above), headache, weakness, chills, characteristic pain in the mammary gland, breast swelling and redness.
Manual examination reveals painful lumps. Feeding or pumping with developed mastitis is accompanied by acute pain, while with lactostasis, on the contrary, relief is felt.
Lactostasis must be distinguished from mastitis. With lactostasis , milk is expressed freely and becomes easier, the temperature returns to normal, there is no redness or swelling, and the pain subsides.
Preventive measures
These include:
- fully express breast milk after each feeding, avoid stagnation;
- correct attachment of the baby to the breast (the nipple and areola should be completely covered);
- timely treatment of cracked nipples, lactostasis;
- compliance with the rules of hygiene and breastfeeding techniques;
- wearing a bra that is not too tight;
- carrying out air baths for the breast (10-15 minutes after feeding).
Condition of the chest and abdomen
- After giving birth, you need to monitor and carefully care for your breasts; you don’t need to wash them or “cook” them for the baby, this can only cause harm. But you must react to unexpected hardness, hot spots and redness. Immediately after childbirth, the breasts swell, become larger and even firmer. Correct latching of the baby to the breast will help here, without a regimen, and then when the baby wishes. Moreover, you need to change positions so that the baby frees all the ducts and there is no stagnation. To smooth out the initial discomfort, which will then go away when breastfeeding improves, you can apply cool compresses, or even better, a cabbage leaf.
- For some reason, many women believe that the belly will “go away” immediately after giving birth and are disappointed when this does not happen. Some women even look pregnant a year after giving birth. In this matter, you need to be patient, since the uterus has been purposefully stretched for nine months, and is not able to “tighten” in a short period of time. This happens within two months, but the stomach can remain pregnant for a long time, since fat accumulates there - this is the body’s defense mechanism. It is difficult to lose weight while breastfeeding, but as soon as a woman stops breastfeeding, weight loss occurs faster. It’s also worth doing yoga and light physical exercise three months after giving birth to restore tone to your body.
Inflammation of the urethra
It is considered normal if in the first days after childbirth, a woman experiences pain during urination, as well as a burning sensation.
But if this continues , even when the tears and stitches in the perineal area have already healed, an inflammatory process may have begun and an infection may develop.
How to recognize?
Symptoms of inflammation:
- difficult and painful urination, or the presence of desire, but without urine discharge, or scanty discharge;
- elevated temperature;
- cloudy urine color and pungent odor;
- presence of pain on both sides of the lower back.
Causes:
- use of a catheter during childbirth;
- in case of violation of the integrity of the bladder during natural childbirth;
- low bladder tone (especially after epidural anesthesia);
- injuries when using obstetric forceps.
Signs
Symptoms of the disease depend on its type, characteristics, and also on the form in which it occurs. With a chronic course, symptoms are often absent altogether, or are expressed so implicitly that they can be completely ignored by the woman. But after childbirth, especially with the use of cesarean section, such a course is almost not observed, and the phenomenon is acute in most patients. The subacute course is characterized by mild symptoms and is also uncharacteristic for women who have recently become mothers.
In an acute picture, the following symptoms form:
- Increased body temperature, depending on the type of disease and its course - from low-grade (37.2-37.3 degrees) to high (38-39 degrees);
- General signs of the inflammatory process are pallor, lethargy, drowsiness, intoxication;
- Abdominal pain, which, depending on the nature of the lesion, can be localized only on one side or on both;
- Acyclic uterine bleeding is not observed in all diseases, but they are present, for example, in endometritis, and can lead to the development of anemia and deterioration of well-being;
- Menstrual dysfunction also does not occur in all pathologies, but is sometimes observed;
- Uncharacteristic, pathological discharge of a purulent or serous nature, a significant increase in the amount of discharge, its thickening and other deviations in this area.
Signs of uterine inflammation after childbirth can be especially severe. And a woman often consults a doctor in a timely manner precisely for this reason. Therefore, treatment of such pathology is usually carried out in a timely and successful manner.