Pathological changes in the cervix can occur in benign and malignant scenarios. Non-tumor processes include erosions, polyps, ectropion, simple leukoplakia, ectopia. Cervical cancer is malignant in nature. An intermediate position is occupied by precancerous changes - dysplasia, which is also called cervical intraepithelial neoplasia CIN (Cervical Intraepithelial Neoplasia-CIN).
A synonym for the disease is squamous intraepithelial lesion PIP (SIL). The frequency of the pathology is steadily increasing, affecting young women, and negatively affecting the reproductive process. What leads to lesions of the cervix, how do they manifest, what modern methods of therapy exist?
Causes
What are the causes of Lsil development of the cervix? Quite often, the disease is associated with damage to the cervix by the HPV virus.
Today, doctors know more than 100 subtypes of HPV. At the same time, a separate group of viruses has been identified that can infect the cervical mucosa. HPV is transmitted through sexual contact. In most cases, self-healing occurs. If this does not happen, then the virus goes into a dormant state and becomes active when favorable conditions arise. These include:
- weakening of immune defense;
- advanced age;
- infection with specific HPV subtypes.
It is HPV, according to numerous medical studies, that causes the formation of genital warts and Lsil of the cervix.
But the development of dysplasia is not diagnosed in all infected women. This requires a combined effect on the female body of several provoking factors at once. In particular, active smoking in combination with any immunodeficiency state increases the risk of cervical Lsil formation several times.
Prevention
To prevent pathology, factors contributing to its development are eliminated. They conduct educational work among schoolgirls, promote a healthy lifestyle, and preventive examinations using the PAP test in the form of screening.
HPV is detected during examinations, its serotype and potential danger are determined, and preventive vaccinations against the human papillomavirus are given to uninfected people and children. Treat inflammatory diseases of the female genital organs.
Intraepithelial lesions of the cervix are a preventable process. The presence of pathology is a reason for timely, adequate therapy. If the optimal timing of treatment is observed and there is a sufficient amount of therapy, the prognosis for recovery is favorable.
Symptoms
Lsil of the cervix occurs, as a rule, without any pathological symptoms that help to suspect the development of the disease. For this reason, gynecologists strongly recommend that all women over 21 years of age and who have regular sex life undergo periodic screenings.
The basic method is the PAP test, which allows one to obtain the necessary biological material for cytological examination. Liquid-based cytology is considered a more effective technique. But this technique is practiced quite rarely, since not all medical institutions are equipped with the necessary equipment.
The first test is recommended to be performed 3 years after the start of sexual activity. And then every 2 years until the age of 30. Then a Pap test is performed once every 3 years. But such a “schedule” must be followed if tests show complete health. If deviations are detected, testing should be carried out much more often.
After reaching the age of 65, taking smears to identify atypical cells stops in the following cases:
- the previously obtained results had no deviations;
- the cervix was surgically removed, in particular, when a large myomatous node of the uterine body was diagnosed.
It is important to remember that if 9 studies showed negative results, then Lsil cervical cancer is 99% excluded.
Gynecologists recommend undergoing a full medical examination if the following symptoms appear:
- pain in the pelvic area;
- the appearance of intermenstrual bleeding;
- cloudy leucorrhoea with an unpleasant specific odor;
- too heavy menstruation;
- blood after sexual contact;
- chronic constipation that does not “respond” to the use of laxatives;
- regular swelling of the lower extremities.
Diagnostics
The development of cervical Lsil requires a certain period: sometimes it takes several years for the disease to form. That is why regularly visiting a gynecologist and conducting an intimate examination is an extremely important measure that allows you to diagnose precancerous changes in the cervix, and also acts as a preventive measure for the disease.
In order to diagnose Lsil of the cervix, doctors practice the Papanicolaou test (PAP test) - a smear obtained from the mucous membrane of the vaginal segment of the cervix. It is used as screening or primary detection of Lsil. The principle of testing is not complicated, which makes it most popular when it comes to choosing a screening technique.
The sampling scheme for material research is quite simple:
- gynecological speculum is inserted into the vaginal cavity;
- Using a special brush, a smear is taken from the cervix;
- the resulting cells are distributed over the surface of a glass slide for subsequent examination under a microscope.
Modern medicine offers more advanced technologies. The cells obtained using a smear are placed in a liquid medium and used for microscopic or cytological examination.
Additional diagnostic techniques
If the Papanicolaou smear used for primary diagnosis could not accurately indicate Lsil of the cervix, then additional research methods can be used.
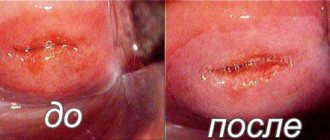
Colposcopy
The technique is a gynecological examination, during which the doctor examines the mucous surfaces of the vagina and cervical mucosa using a specialized microscope (colposcope). Modern devices are often equipped with video screens, which allow the doctor to see tissue on the screen. The colposcope provides multiple magnification, down to the cellular level. The technique allows you to determine all existing anomalies on the surface of the cervix and vagina.
Biopsy
The technique is one of the most informative ways to diagnose Lsil of the cervix. The biopsy is based on the collection of living material from the problematic part of the cervix and subsequent examination of the cells under multiple magnification. The reliability of the results obtained during the biopsy reaches 99%, which makes it possible to diagnose Lsil.
HPV test
To identify the relationship between the development of cervical Lsil and the presence of human papillomavirus (HPV) in the patient’s body, a special test is performed. It will be necessary if the Pap test reveals the presence of atypical cells.
In recent years, the HPV test has been quite often practiced as an isolated method for detecting Lsil of the cervix without the use of a Papanicolaou test. The diagnosis can be considered confirmed with a high degree of probability with the combined detection of changes in the mucous membrane of the cervix and determination of HPV in the woman’s blood.
Squamous interepithelial lesion of the cervix: low and high grade
Cervical neoplasia is a lesion of the cervix that develops in the presence of an oncogenic human papillomavirus infection in the body. A pathological change occurs in the squamous epithelium into deeper layers of tissue, with some of the epithelial cells being replaced by atypical cells with an altered nucleus.
Cells' life resources are significantly reduced; they cease to perform such important functions as:
The basal layer of squamous epithelium is involved in cell reproduction, but when immunity is impaired, their uncontrolled reproduction is typical.
Intraepithelial neoplasia is typical for women of reproductive age - from 20 to 30 years. This period is characterized by increased sexual activity and the risk of contracting the human papillomavirus.
What is squamous intraepithelial lesion of the cervix?
There are two abnormalities of cells that develop atypically:
- SIL is a squamous intraepithelial lesion, which in turn has two stages (low and high grade);
- squamous cell carcinoma.
With a low (LSIL) degree of damage, there is a possibility that treatment will not be required, since this type is not cancer. With this pathology, HPV cells can be damaged; if a woman has a strong immune system, then the affected cells will never degenerate into cancer.
The result will be more favorable if proper treatment and support of the body is carried out. In addition, doctors recommend getting rid of bad habits.
With a high (HSIL) degree of damage, if treatment is not followed, the cells are more likely to malignize into cancer.
Squamous cell carcinoma is an invasive cancer that affects other tissues of the cervix in addition to squamous epithelial cells.
The name “intraepithelial lesion” is more typical of Western medicine. Domestic doctors prefer the term “dysplasia”, which has three stages:
- CIN1 is a low-grade dysplasia, in which changes in the epithelium are minor and cover less than a third of the depth. Most often, dysplasia is indicated by keratosis and koilocytosis (cell changes characteristic of the papilloma virus). Diagnosis and testing for oncology is difficult because the biopsy material is small.
- CIN2 is a more pronounced process of changes in the epithelial layer. The depth of the lesion is half the layer. If second-degree dysplasia is detected and treated in time, a favorable outcome of the disease is possible.
- CIN3 – almost the entire epithelium is affected, the area of distribution is more than 2/3. This type of cancer is called in situ, that is, cancer without penetration through the basal layer.
All of these types of dysplasia are characterized by pathological changes at the cellular level. Once the diagnosis of CIN3 is confirmed, immediate treatment begins. Most often, surgical removal of the cervix is proposed, followed by prophylactic treatment to prevent recurrence.
Low risk
Low-grade intraepithelial lesions of the cervix occur due to infection with the human papillomavirus (HPV), which is sexually transmitted. The virus penetrates the cells and disrupts the functioning of the entire cellular mechanism of a woman; they are exposed to the waste products of the virus - proteins. In 90% of cases, HPV strains 16, 18 and 45 are detected.
If low-grade tissue damage is detected, then the obligatory condition is the observation of a gynecologist who, after conducting tests, will prescribe proper treatment.
Mandatory tests include a DNA test for the presence of papillomavirus.
If the result is negative, the examination is repeated after a year, since the virus develops over a long period of time: sometimes from the moment of infection to external visible manifestations on the cervix it takes 10 to 20 years.
If the result is positive, it is recommended to scrape the cervical canal to take an analysis for oncocytology, if changes are not visible from the vagina, but they are concentrated in the cervical canal. Based on the test results, the doctor plans further actions to manage the patient with a precancerous condition.
High risk
High-grade squamous cell lesions of the cervix are classified as emergencies. When visually examining damaged tissues, colposcopy is prescribed with the simultaneous removal of a piece of tissue for examination.
A biopsy is not performed during pregnancy due to the risk of miscarriage. During this period, a cytological examination - Pap test - is indicated. Subsequent treatment is carried out in the postpartum period. It happens that the disease develops without treatment, so you should wait for recovery after childbirth and conduct a re-examination.
Loop excision is prescribed when biopsy results show unsatisfactory or unreliable results. After conization, the material is sent to the laboratory for further histological examination.
Symptoms of intraepithelial lesions
Damage to the cervix may occur without visible symptoms. If a woman notices spotting after intercourse, minor pain in the lower abdomen or lower back, then she should be examined by a gynecologist to rule out squamous cell neoplasia (tumor). In addition, the manifestations described above are characteristic of severe dysplasia.
Diagnosis of cervical neoplasia
The first analysis, a Pap test, allows you to determine the presence of dysplasia as such. During the examination, the doctor takes a smear from the surface of the cervix and sends it for examination.
Next, to determine the extent of intraepithelial damage, a biopsy is recommended. Under the control of a colposcope, a piece of tissue is taken from one or two areas of the cervix. You should not reject such a doctor’s offer, since cell changes can occur directly in the cervical canal.
During an instrumental examination, it is not always possible to see the beginning changes in the tissue; cells for analysis will have to be removed from the cervical canal. A piece of tissue is taken from the most suspicious loose areas; based on the results of the biopsy, the depth of tissue damage and the degree of cell changes can be determined.
An analysis for tumor markers is done if cancer is suspected. The essence of the method is to introduce the reagent into the blood; if the concentration of the tumor marker is high, the analysis will be positive. This method is used after treatment or surgery to remove a malignant tumor; it is aimed at preventing relapse.
Why do diagnostic errors occur when cytology shows the presence of severe pathological changes, but a biopsy does not confirm cancer? The fact is that during a cytological examination, the doctor uses a special brush to capture a wider, moist surface of the affected tissue, and during a biopsy, a pinch is made in one or two places. Therefore, several types of tests should be used to get an accurate picture of the disease.
Treatment of intraepithelial squamous cell lesions of the cervix
If test results indicate cancerous changes, then only surgical treatment is indicated. For nulliparous women, this can result in infertility, since during pregnancy the cervix performs a supporting function. Currently, the method of implanting a locking element made of titanium nickelide is used; it allows women with an amputated cervix to bear a child.
Gentle methods for low-grade lesions are therapy with immunostimulating drugs and local agents. In more severe situations, methods of radio wave, laser, and ultrasound tissue destruction are used. For postmenopausal women, cheaper methods are recommended - electrocoagulation, cryodestruction or conization with a scalpel.
conclusions
Nulliparous women need to choose more gentle methods for the treatment of cervical dysplasia in order to preserve reproductive function and reduce the risk of developing cancer.
: Mild and severe intraepithelial lesions of the cervix: diagnosis and management tactics
Source: //sheika-matka.ru/zabolevaniya/rak/ploskokletochnoe-intraepitelialnoe-porazhenie-shejki-matki/
Degrees of dysplasia
It is customary to distinguish several degrees of Lsil of the cervix.
- The first degree (CIN I) corresponds to mild dysplasia. At this stage of the disease, a small number of atypical cells are detected in the upper layers of the mucosa. The condition does not pose a particular danger to the patient’s health and in some cases it heals on its own, but it all depends on the strength of the immune system.
- The second degree of CIN II is considered moderate and is accompanied by damage to the mucous layer by approximately 50% in depth. Dysplasia is represented by cells that are changed in shape and size.
- Third degree CIN III. In this case, approximately 70–90% of the entire thickness of the epithelial layer is involved in the pathological process. The condition is recognized as a severe form of dysplasia and is defined as a precancerous condition. If a woman does not receive specialized treatment, the pathology will spread to neighboring tissues. According to data, the process of degeneration occurs in 20–30% of all diagnosed cases, which leads to the development of squamous cell carcinoma.
- Stage four is considered invasive cancer. Previously, gynecologists believed that Lsil cervix should go through all stages. But today it is reliably known that invasive cancer develops in approximately 1% of cases in the first stage, in 5% in the second stage and in 12% in the case of the third stage.
Spontaneous regression of the disease during the first year is observed in approximately 70% of all women diagnosed with the first degree of cervical Lsil, and in 90% during the first two years.
Self-healing in the second degree of dysplasia occurs in approximately 50% of patients.
Classification
There is an international classification according to which CIN is divided into three degrees - mild, moderate and severe.
- Mild CIN1 - pathological changes occur in the lower third of the epithelial layer, these include proliferation, mitoses while maintaining the normal ratio of cytoplasm and nuclei.
- Average CIN2 - changes in the lower and middle third of the epithelial layer.
- Severe CIN3 - damage to the entire thickness of the epithelium. It is characterized by significant proliferation, nuclear hyperchromatosis, disruption of the nuclear-cytoplasmic ratio in favor of the nucleus, and numerous normal mitoses.
Source: dermatologvenerolog.ru
Severe degrees are usually called CIS or carcinoma in situ, this is justified due to the complexity of their cellular differentiation. The more severe the degree of dysplasia, the higher the likelihood of developing a malignant process. In the new classification, mild squamous intraepithelial damage is designated as LSIL, and moderate and severe stages are combined into one group HSIL.
In the literature, the term CGIN low grade is found - mild cervical glandular intraepithelial neoplasia, implying a combination of grade 1 and 2 dysplasia. The term high grade refers to severe CIN or adenocarcinoma in situ. These are epithelial changes that precede cervical cancer.
Treatment
Lsil treatment for first stage cervix is not complicated. As a rule, the disease is a consequence of an untreated inflammatory process – colpitis. In the presence of HPV and established Lsil (dysplasia), therapy takes longer. When a pathology is diagnosed, a woman is prescribed conservative therapy, which involves taking medications.
Treatment in the presence of papillomavirus is accompanied by immunomodulation and antiviral agents, which are prescribed before and after conization to prevent relapse. The course of therapy is long and lasts 4–8 months.
If the microflora smear results are poor, indicating current inflammation, the patient is prescribed local antibiotics and antiseptics. The following medications with a wide spectrum of action are most often prescribed:
- Terzhinan;
- Hexicon;
- Klion D;
- Metronidazole;
- Clindamycin.
Duration of therapy – 5 – 10 days.
In order to restore the normal balance of vaginal microflora, the following may be prescribed:
- Acylact;
- Lactonorm.
Six months after treatment, it is necessary to take a smear again to completely exclude the presence of an inflammatory process. A cytological examination will also be required.
The cause of mild dysplasia is most often caused by HPV of various strains. The most frequently detected varieties are 16, 18, 31 and 45. It is they that cause the development of Lsil of the cervix and its degeneration into cancer.
The prognosis with correct therapy is favorable. Approximately half of women diagnosed with cervical damage caused by the HPV virus experience spontaneous recovery within the first two years from the onset of the disease.
Moderate and severe dysplasia requires not only medication, but also surgical treatment. If damage to a significant layer of cells is diagnosed - more than 2/3 - then relieving the inflammatory process alone is not enough.
If a PAP test or other analysis shows a second or third degree, the patient requires urgent consultation with an oncologist.
It is worth remembering that it is impossible to determine the current form of Lsil of the cervix from just one smear. As a rule, in this case, the painful procedure of conization (excision) of the cervix or complete resection in the case of diagnosing third degree dysplasia is prescribed. The operation simultaneously serves as a diagnostic and therapeutic measure.
In addition to conization, other techniques can be used for mild dysplasia:
- Diathermocoagulation. During the procedure, pathological cells are destroyed using high-frequency electric current. A painful scab forms in the treatment area. The technique is practiced in rare cases, since it is characterized by low efficiency in combination with frequent complications.
- Cryodestruction. The doctor treats the affected area with liquid nitrogen, which causes complete destruction of the atypical cells. The method can be used in nulliparous women, but the wound takes a long time to heal and there is a risk of inflammation.
- Laser vaporization. The affected area is treated with laser beams. During the procedure, all fluid is completely removed from the affected cells and they are destroyed.
In a situation where Lsil of the cervix is mild, and the woman plans to have a child in the future, the doctor tries to preserve the functional abilities of the cervix. Then it will be possible to achieve gestation naturally.
In such cases, the patient is prescribed a conization procedure. It is a cone-shaped removal of the cervix. The operation is performed in two ways:
- knife conization - using a surgical scalpel;
- radio wave conization - performed with the Surgitron apparatus.
The removed tissue is sent for cytological examination. If the doctor diagnoses the absence of atypical cells along the edges of the cone, this means complete removal of pathologically altered tissues.
If atypia is detected, re-treatment is prescribed.
In the absence of Lsil of the cervix - after complete restoration of the organ - the woman is allowed to plan gestation.
If a severe degree of dysplasia is diagnosed and it is not possible to carry out conization adequate in volume, the patient is prescribed amputation of the vaginal segment of the cervix. After the operation is completed, the woman retains only a small part of the cervical canal - no more than 1 - 2 cm. For a full pregnancy without the constant threat of miscarriage, this distance is not enough.
The danger of third stage Lsil cervical cancer is that it can develop into invasive cervical cancer at any time. And then the entire cervical canal, body of the uterus, tubes, ovaries, etc. will be involved in the pathological process.
Treatment of cervical dysplasia
Remember: how, with what and when to treat - only a doctor can answer this question. You cannot introduce any folk remedies into the vagina, otherwise you will provoke complications.
Principles of treatment depending on the degree of disease
1) Mild treatment. It is carried out with general strengthening drugs. That is, drugs are used, including folk remedies, that increase immunity. According to modern recommendations, a mild degree does not require specific treatment, since in 90% of cases it goes away on its own.
2) Moderate treatment. Drug treatment is necessary, although in some cases you can also get by with restorative drugs.
Moderate degrees heal on their own in 70% of affected women. If human papillomavirus is detected in the tests, then treatment should be started immediately.
3) Severe treatment. Drug treatment is mandatory, otherwise there is a very high risk of neoplasia degenerating into cervical cancer.
Treatment regimen for cervical dysplasia
Treatment methods
Therapeutic treatment
1) Antiviral drugs locally - in the form of douches, suppositories, tampons
2) General antiviral agents - to suppress the virus in the body as a whole:
- isoprinosine (or groprinosine) - detailed instructions
- allokin-alpha - detailed article about allokin
- epigen intimate - more about epigen
- Panavir - instructions for the drug
3) immune drugs (polyoxidonium, roncoleukin, immunal, viferon, genferon and other interferon drugs).
Surgery
1) electrocoagulation, or electroconization, or loop electroexcision of the cervix. Conducted by a gynecologist. A special metal loop under the influence of electric current influences the epithelium of the cervix.
2) laser vaporization, laser conization of the cervix. The mechanism of action is the same, only a different factor of influence is not electric current, but a laser.
3) treatment with radio waves using the Surgitron device. The method of exposure is similar to laser, but the main factor is radio waves. Read the article about radio wave treatment
4) cryodestruction, or cauterization with liquid nitrogen. Thermal destruction of the affected epithelium occurs, it dies and a new, unaffected epithelium grows in its place. Read the article about liquid nitrogen
5) ultrasonic destruction. The mechanism is similar to the effect of a radio wave or laser, only the active factor is ultrasound.
6) conization with a scalpel. Classic surgery using a scalpel. Currently rarely used, as the above methods are more effective.
7) amputation of the cervix. This is already an extended operation. Used for cervical cancer.
Onset of pregnancy
About the possibility of planning pregnancy after complete resection of the cervix for Lsil, a woman should consult with her oncologist. If he gives permission, then it is necessary to contact a gynecologist to put stitches on the remains of the cervix before pregnancy occurs. The procedure is performed using laparoscopy, since the vaginal segment of the cervix is completely absent.
If pregnancy occurs before suturing, the procedure is performed in the early stages by access through the vaginal tube or during laparoscopy. The use of cerclage with mersilene tape has worked well.
If suturing is not possible, but the woman has preserved the vaginal part of the cervix, she will be recommended to install a pessary. In addition, it is necessary to completely eliminate any physical activity for the entire period of bearing a child.
Summary
It is worth noting that a recurrence of Lsil cervix cannot be ruled out and none of the modern methods can guarantee a complete cure. In particular, the development of dysplasia can be resumed by the absence of a course of antiviral therapy after destruction of the pathological focus.
Most often, the re-development of Lsil of the cervix is due to the presence of the HPV virus in the female body. To exclude a recurrence of the pathology, it is necessary to get rid of all provoking factors - HPV, sexually transmitted infections and correct existing hormonal imbalances.