Cervical ectopia of the cervix: what is it?
Modern medicine uses such definitions as pseudo-erosion, endocervicosis, false erosion to designate the disease ectopia. Ectopic columnar epithelium of the cervix occurs in 40% of women, while more than 11% of all cases are congenital anomalies. Patients of childbearing age are at risk (up to 50% of all cases). A history of ectopia in women increases the risk of the formation of malignant tumors, as well as the development of various inflammations of the vulva.
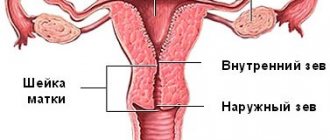
During a gynecological examination without the presence of ectopia, the cervix is covered with squamous epithelium in several layers. Using mirrors and internal examination, the cervical canal, which is covered with columnar epithelium, is revealed. In the presence of cervical ectopia, the photo demonstrates that the line between the epithelia is deformed and moves closer to the outer cavity of the vagina, being located either locally or in a circle, the picture is completely different.
Anatomy
The cervix is located in the upper zone of the vagina, has a length of about 3-4 cm and a normal cylindrical shape. This is an organ consisting of smooth muscle fibers, connective tissue and penetrated by blood vessels. Thanks to this, it has the ability to strongly contract, stretch, and change shape.
The cervical region performs several important functions in a woman’s body:
- protects the genital tract from the penetration of pathogenic microorganisms: bacteria and viruses;
- the closure of the external and internal pharynx during pregnancy ensures retention and gestation of the fetus;
- the inner lining produces special mucus, which has an important immunological function and provides a reliable barrier that protects the uterus from inflammation;
- smoothing and shortening the cervix makes it part of the birth canal, and therefore ensures reproductive function.
The cervical canal, located inside the cervix, is a “corridor” between the external and internal environment of the body. This means that it is through it that the sperm move to the egg for fertilization, as well as the secretion of mucus, the passage of the plug and the release of blood during menstruation.
Between the cervix and the body of the uterus there is an internal os. Its discovery is associated with certain periods of the menstrual cycle. The external os, which opens into the vagina, plays an important role in protecting the internal organs and the fetus from possible infection or contact with pathogens.
The shape of the cervix, conical or cylindrical, is one of the signs by which a gynecologist can determine whether a woman has given birth.
Conventionally, two zones can be distinguished: supravaginal (upper) and vaginal (lower). The entire vaginal part is covered with stratified squamous epithelium, under which there is a network of blood and lymphatic vessels, as well as nerve plexuses. The main importance of this type of epithelium is the secretion of keratin and glycogen. Keratin makes the mucous membrane stronger, and glycogen provides the necessary acid-base balance.
In turn, the supravaginal area is the cervical canal, which is lined from the inside with columnar epithelial cells. The main function of the channel is to secrete mucus, which has protective properties. The border between the upper and lower parts of the uterus is the zone of the internal os, which opens into the vagina.
Classification of cervical ectopia of the cervix
Modern medicine defines several forms of ectopia, both by origin and localization, and by the course of the disease. Ectopia can be either a congenital disease (about 11% of all cases) or acquired. Signs of ectopia may be uncomplicated, which is the norm on an individual basis and does not require treatment; complicated ectopia is often caused by inflammation inside the genital organs, which also involves diseases such as colpitis and cervicitis. These diseases are infectious, their complete cure is necessary first of all. In the future, the prognosis of ectopia may not have any signs and a relapse may occur.
- When the structural and skin elements of the cervix change, as well as when their relationship is dysfunctional, cervical ectopia is ectropion.
- Based on histological characteristics, they are distinguished:
- pseudo-erosion;
- papillary - structural formations of the cylindrical epithelium of the uterus;
- glandular - ectopia with inflammation, abscess of glands with branching is noted.
Scarring during ectopia is accompanied by the transformation and renovation of the epithelium from cylindrical to flat. The process involves additional cells, which, through division, turn into an immature form, and then acquire a mature stage.
With colposcopy, it is possible to differentiate changes in the skin. Under negative conditions, cellular transformation may not have a logical conclusion. In this case, a relapse of ectopia occurs. It is also possible for a retention cyst of the cervix to appear if the pharynx has a skin growth of a metaplastic type.
Changes after childbirth and during pregnancy
After childbirth, the shape of the cervix and the opening of the cervical canal change. This means that the conical shape is replaced by a cylindrical one, and the rounded opening of the external pharynx is replaced by a slit-like one. But these are not the only changes. Examination of the cervix in the early stages of pregnancy is necessary to identify any abnormalities or abnormalities.
Once fertilization has occurred and the embryo has successfully implanted, the cervix begins to change its color and consistency. It takes on a bluish tint and a loose, soft texture, but still remains conical in shape.
All these changes are explained by the emergence of new life, which means there is a need to increase blood circulation, supply of nutrients and oxygen to the fetus. As a result, the conical neck becomes softer and changes color.
In later stages of pregnancy, the conical cervix begins to shorten. If in a normal position its length can reach 3-4 cm, then before childbirth it is only 0.5-1 cm. This means that by the degree of opening of the cervical canal the doctor can judge how soon the birth process will begin.
As the baby moves along the birth canal, full dilation of the cervical canal can reach about 10 cm. In some cases, due to weak labor or, conversely, too rapid labor, rupture of the walls may occur. To avoid this, it is necessary to follow breathing techniques, and doctors carry out a set of measures aimed at protecting the cervix from ruptures and maintaining its normal shape. After the birth of a child, the cervix changes its shape, which means that instead of conical it becomes cylindrical.
Causes of cervical ectopia of the cervix
Cervical ectopia can develop in conditions of changes in the functional systems of the body, including:
- hormonal disorders;
- inflammatory processes;
- presence of injuries and damage to the genital organs;
- general decrease in immunity due to chronic diseases.
The causes of ectopia of the uterus are diseases of the reproductive system that occur in the patient’s history and which have relapsed. Such diseases include chlamydia, mycoplasmosis, vaginitis, endocervitis. Changes in the microflora of the vagina, a quantitative increase in opportunistic flora due to bacteria such as streptococcus, staphylococcus, E. coli, etc. - all this can lead to the development of ectopia. In addition, vaginal discharge provokes changes in the squamous epithelium of the cervix, where erosion forms. In the future, erosion is differentiated as ectopia.
Injuries and mechanical damage can cause ectopia. Difficult childbirth, surgical termination of pregnancy, douching, insertion of an IUD also increases the risk of pseudo-erosion and the development of the inflammatory process.
Hormonal imbalance in the body is also one of the causes of ectopia. Very often it is a concomitant disease with ovarian dysfunction, endometriosis, fibroma.
A decrease in the immune system and protective properties of the body can develop as a result of diseases such as diabetes and obesity.
The following conditions play an important role:
- early sexual life;
- frequent change of partners;
- unprotected sex;
- multiple births;
- multiple abortions.
All this is fertile ground for the occurrence of pseudo-erosion.
Causes of heterogeneous uterine structure
Various processes can cause changes in the structure of the uterus so that it appears heterogeneous on ultrasound. These include:
- hormonal imbalance, for example, thyroid dysfunction;
- inflammatory process, including an infectious one;
- tissue hyperplasia, leading to the development of benign and malignant tumors;
- injuries due to gynecological operations, difficult childbirth.
These processes lead to the development of diseases leading to structural changes. On ultrasound, they can be focal, located only in one area, or spread along all the tissues of the uterus. Among these diseases are the following:
- endometriosis or adenomyosis , when the inner layer grows into the myometrium in the form of branches or cystic formations;
- benign tumors, polyps that form both in the organ cavity and in the cervical canal;
- malignant neoplasms of the uterus and cervix;
- endometrial hyperplasia;
- fibroids (diffuse), small, multiple;
- myometritis or an inflammatory process in the myometrium, causing tissue sclerosis and the formation of adhesions (synechias).
Symptoms of cervical ectopia
Symptoms and manifestation of ectopia are observed in a complicated form. As a rule, it is accompanied by diseases such as dysplasia, leukoplakia, and polyps. There may be a discharge that is whitish or mixed with blood in the presence of colpitis or endocirvicitis.
At the initial stage of a complicated form of ectopia, the patient may complain of changes in the nature and timing of the menstrual cycle, as well as the inability to become pregnant for a long time (1 year).
The uncomplicated form of cervical ectopia of the cervix does not have any special signs. During a gynecological examination, it is easily detected by a specialist.
Shape Features
Pathological changes often occur on the vaginal surface of the cervix, in the “transition zone” of one epithelium to another. When the localization of this zone changes, background diseases arise: ectopia (pseudo-erosion), ectropion, leukoplakia, erythroplakia, polyps and, as a consequence, malignant neoplasms of the cervix.
Ectopic cervix
Ectopia (pseudo-erosion) is a disease of the cervix, characterized by the emergence of columnar epithelium on the vaginal surface of the cervix. Women with irregular menstrual cycles are predisposed to developing this disease.
The clinical picture is somewhat blurred. Such women may complain of the release of blood clots after intercourse and the pain of the process of intercourse itself. The disease can be recognized during a medical examination of the cervix in the mirror: the surface of the organ will not be pale pink, but a bright red hue.
Ectropion is an eversion of the mucous membrane of the cervical canal into the vagina, with the formation of scars and ectopia on the cervix. This disease occurs as a result of unsuccessful diagnostic or surgical intervention on the uterus, as well as after labor or abortion.
Leukoplakia is a disease associated with the appearance of keratinized areas on non-keratinized epithelium. Leukoplakia can be simple or proliferative. The proliferative form is a precancerous condition and when biological material is taken from this area (biopsy), atypical cells are found.
With erythroplakia, the cervix is affected locally, closer to the external os. The pathogenesis of the disease is the thinning of the stratified squamous epithelium and, as a result, tissue atrophy. The etiology of erythroplakia has not yet been studied. The photo clearly shows red spots in the ectocervix area.
Cervical polyps
Polyps are growths of various sizes on the mucous membrane of the cervical canal. According to their structure, polyps are epidermal and glandular. When examined in a speculum, the polyps are oblong and leaf-shaped. It is possible to diagnose and differentiate such polyps only with an ultrasound examination of the pelvic area.
Cervical endometriosis is a disease in which tissue similar in structure to the endometrium is located on the vaginal surface of the cervix. Normally, such tissue should be located in the uterine cavity.
The main reasons for the development of this disease:
- cervical injuries due to violence, childbirth or abortion, as well as medical interventions;
- genetic predisposition;
- hormonal disbalance.
Patients with cervical endometriosis usually do not present characteristic complaints. There is discomfort during sexual intercourse, bleeding after intercourse, as well as before and after menstruation.
Cervical cancer
Cervical cancer (CC) is a malignant neoplasm of the cervix. The location and form of cancer is varied. The main component of the disease is atypical cells that can divide uncontrollably and replace healthy cells. In 90% of all cases, the cause of cervical cancer is the human papillomavirus. The main route of transmission of the pathogen is sexual intercourse.
Factors that increase the risk of developing the disease:
- early onset of sexual activity (before 17 years of age);
- failure to comply with hand and body hygiene rules;
- the presence of precancerous conditions (proliferative leukoplakia, polyps);
- frequent change of sexual partners;
- bad habits;
- infection with the papilloma virus in another way (during medical interventions, transmission from mother to fetus).
With progression, when the malignant disease moves to the next stage and grows, bleeding and nagging pain may appear in the lower abdomen. CC can be suspected only by performing a biopsy of the affected tissue for the presence of atypical cells.
The shape of the cervix and the diameter of the pharynx may differ in a girl who has already become a mother and in one who has not yet given birth. The reason for this is the strong stretching of the organ during pregnancy and during childbirth.
In women who have not yet given birth, the cervix has a conical shape. What does it mean? Since there was no movement of the child along the birth canal and no strong opening of the external pharynx, the lower region is significantly narrower than the upper. In this case, the opening of the cervical canal has the shape of a point. In such cases, during a gynecological examination, the doctor observes a conical shape, which means we can talk about the absence of pregnancy and childbirth.
In women who have given birth, the cervix has the appearance of a cylinder with a slit-like opening of the external pharynx. This means that based on these signs, the doctor can determine whether a woman has given birth.
Diseases of this organ are divided into the following types:
- Background – not associated with malignant processes.
- Precancerous (dysplasia) - there are areas with damaged cell structure (atypical cells), but without malignant changes.
- Cancer is a malignant change in cellular structure.
Most cervical diseases occur without symptoms. In some cases, they may be accompanied by increased discharge, discomfort during sexual intercourse, and bloody discharge. But even cervical cancer can cause severe symptoms only at a late stage, when the disease is difficult to cure.
Pathology of the cervix can only be detected by specialized methods during a gynecological examination.
These methods include:
- Cytology smear (PAP test). Allows you to suspect the presence of atypical cells and the degree of their damage, to identify the inflammatory process in the cervix. Based on the results of the PAP test, further examination of the patient is performed.
- Colposcopy. Visual examination of the mucous membrane of the organ using an optical device - a colposcope. During colposcopy, various tests can be performed to identify damaged areas, and a piece of tissue can be taken (biopsy) for histological examination.
- Histological analysis. Study of the cellular structure of the selected biomaterial under a microscope. The diagnosis of “dysplasia” and “cervical cancer” can only be made based on the results of histology.
- Flora smear. It is performed to identify pathogenic flora and determine its sensitivity to antibiotics and antifungals (antifungal drugs). The analysis is necessary to organize the treatment of inflammatory processes.
Your doctor may also order blood tests for sexually transmitted diseases (STDs) and human papillomavirus (HPV). Some strains of HPV are oncogenic and cause dysplasia and cervical cancer.
Oncological processes of the cervix develop rather slowly, going through three stages of dysplasia - mild, moderate and severe. And even the third degree of dysplasia can be treated with complete preservation of the woman’s reproductive function.
Early stage cervical cancer also has a favorable prognosis for the patient if treatment is started on time. Whether the organ will be preserved is decided by the doctor according to the indications.
At later stages, radical hysterectomy is practiced - removal of the uterus with appendages, pelvic lymph nodes and the upper vaginal area.
Let us repeat that dysplasia and subsequently cervical cancer develop slowly, practically asymptomatically, but are easily diagnosed during a medical examination. Whether a woman gets this type of cancer or not is largely a matter of her personal responsibility. An annual visit to a gynecologist for preventive examinations will protect you from this serious illness and preserve your reproductive health.
Diagnosis of ectopic columnar epithelium of the cervix
Diagnosis of pseudo-erosion at the initial stage includes a primary gynecological examination by a specialist, thanks to which it is possible to identify the nature of ectopia - congenital or acquired. If the form is congenital and there are no complaints from the patient, further diagnosis and special treatment are not required. In the acquired form, it is necessary to evaluate the previous nature of the columnar epithelium of the cervix and compare it with changes in the vagina at the time of diagnosis.
Diagnostics using gynecological speculum and instruments reveals a violation of the epithelial line, the presence of a red inflammatory focus of the uterus, which can bleed when pressed.
Colposcopy and Schiller tests are mandatory measures to identify ectopia of the columnar epithelium of the cervix. These methods reveal the following indicators of the disease:
- transformation of uterine tissue into new structural compounds;
- the presence of a cylindrical zone of skin and a displacement of the connection line closer to the exit of the uterus;
- leukoplakia;
- punctuation;
- mosaic.
With the listed signs of ectopia, further diagnosis consists of:
- bacteriological culture;
- PCR diagnostics;
- microscopy;
- cytological examination;
- in some cases, a biopsy is indicated.
Additionally, studies of the ovaries are carried out, their functionality and the presence of possible hormonal disorders are determined. If any violations are detected, consultation with a gynecologist-endocrinologist is mandatory.
Ultrasound diagnosis of heterogeneous uterine structure
Ultrasound examination is performed using the transvaginal or transabdominal method. In children and virgins, perineal ultrasound or transrectal technique is used. The doctor examines the location, size of the uterus, the thickness of the individual layers and their uniformity.
The thickness of the myometrium increases from the cervix to the fundus; in pregnant women it is normally greater, in older women it is less. Pathological growths (fibroids, cancer) affect the thickness of the walls and deform the uterus.
The thickness of the inner layer changes throughout the menstrual cycle, its maximum value in the second half is 16–22 mm. During menopause, the borderline normal value is considered to be a thickness of 6–7 mm.
The myometrium has an average echogenicity, which corresponds to the density of parenchymal organs (liver, renal cortex). Heterogeneity manifests itself with the appearance of anechoic areas, for example cysts in adenomyosis, or inclusions of increased density, areas of proliferation of connective tissue.
Treatment of cervical ectopia
The complicated form of pseudo-erosion has several treatment options, depending on the nature of the identified disorders. Anti-inflammatory drugs must be prescribed. An individual contraceptive program is selected together with a gynecologist-endocrinologist. Hormonal imbalances in the body are also treated.
Treatment of cervical ectopia involves the possibility of undergoing various therapies:
- laser therapy;
- cryotherapy;
- radiosurgery;
- diathermocoagulation, thanks to which the internal inflammatory process of the cervix stops and ectopia recurs.
When diagnosing diseases of the genital organs, further treatment occurs on an individual basis, depending on the specific disease, nature and location.
Uncomplicated ectopia does not require treatment. A patient with a history of this disease should simply be under the supervision of a doctor and follow his recommendations, which should contribute to the regression of the disease. If signs of ectopia are detected, the woman needs to undergo an examination as soon as possible to identify pseudo-erosion of a complicated form.
Details about the female body. All about the cervix
Tuesday, April 30, 2013 – 12:37
For most of our lives, we women don't think about the cervix. How it works, what it is needed for, how it changes during pregnancy. And only when the birth is approaching do we rush to the computer and start loading the search engine with queries like: “What is the cervix?”
However, the rest of the genital organs are given the same honor. We begin to think about her more often as the birth gets closer. Experienced women often give nulliparous women shock therapy, telling them that this part of our body should open as much as 10 or even 12 cm. They probably take pleasure in watching the poor thing turn pale.
If you are about to give birth, read this article. This will help you prepare for childbirth without shock therapy, I will tell you more about your body.
And yet, what is the cervix?
The cervix is the lower part of the uterus that connects to the vagina. It has a cylindrical shape in women who have given birth, and conical in women who have not given birth. The neck consists of muscle fibers. The cervical canal of the cervix passes through the center.
The cervical canal is widened in the middle, which is why it has a spindle-shaped shape; it is on average 3-4 cm long. It opens with an internal pharynx into the uterus, and an external one into the vagina. The cervical canal communicates with the uterus and vagina.
The cervical canal is lined with a mucous membrane, which in medical language is called epithelium. It contains many small glands that produce mucus into the cervical canal. This epithelium is cylindrical. In the vagina it is flat. The transition zone between squamous epithelium and cylindrical epithelium is located on the external os of the cervix.
With frequent inflammatory processes in this area, a process called dysplasia may begin. Dysplasia is considered a precancerous condition and requires mandatory treatment.
An analysis called cytology of a smear from the cervical canal helps to make an accurate diagnosis of dysplasia.
Normally, cytology of the cervical canal and cervix shows that the epithelium does not have atypical cells.
The mucus produced by the epithelium of the cervical canal consists of water, protein, glucose, amino acids and other substances. The amount of water in mucus depends on the level of estrogen (female sex hormones).
After the end of menstruation, mucus contains little water, which is why it is viscous and highly acidic.
Due to the high viscosity and acidity of the mucus, the external pharynx becomes an insurmountable barrier to pathogenic microbes and sperm.
As the egg matures or ovulates, levels of female sex hormones increase. The mucus produced by the epithelium of the cervical canal contains much more water, its acidity decreases. This allows sperm to penetrate through the cervical canal into the uterine cavity. Pregnancy may occur.
How the cervix changes during pregnancy
If pregnancy occurs, high levels of the hormone progesterone contribute to changes: the cervical canal is closed, at 5 weeks of pregnancy, viscous mucus forms a plug that seals the external os. No microbes should have the slightest opportunity to enter the uterus.
The uterus, cervix, cervical canal, urethra, bladder and kidneys with ureters are greatly changed under the influence of progesterone. The cervix and cervical canal become bluish during pregnancy. The volume of urine increases, and the urge to urinate frequently appears. A growing uterus can interfere with the flow of urine.
This makes urinary tract infections easier to occur.
The cervical canal is of utmost importance during pregnancy. The length of the cervical canal should be at least 3 cm. A short neck contributes to the development of isthmic-cervical insufficiency. This condition can cause premature birth and spontaneous abortion.
The growing baby and uterus gain weight.
This increases the load on the cervix and cervical canal during pregnancy. The norm is when the cervix is able to support this weight without dilating. If the length of the cervical canal during pregnancy is less than 3 cm, the cervix may not hold up and open. The pressure of the amniotic fluid will push the membranes into the open canal and they may rupture.
This is how premature labor begins.
Prevention and prognosis of cervical ectopia
Cervical ectopia of the cervix has a positive prognosis when the disease is detected. The disease is monitored through colposcopy every six months, even in the absence of complaints about health.
Carrying out preventive measures consists of timely diagnosis and further treatment of any diseases that the patient has. Women who have endocrine disorders are at risk; they need constant monitoring by a gynecologist-endocrinologist to monitor the condition of the body and timely identify disorders.
Also, to prevent ectopia, constant examination by a gynecologist is necessary to detect infectious diseases of the genital organs.
Proper management of intimate life, properly selected contraception, avoidance of unwanted pregnancy - all these are the main preventive measures that must be observed.
Possible pathologies
In case of infection and inflammation of the organs of the reproductive system, hormonal disorders in the body, as well as in the case of mechanical damage, pathological processes can develop. This is typical for both conical and cylindrical shapes.
Symptoms of cervical canal diseases are usually:
- discomfort or even pain in the lower abdomen or lower back;
- atypical discharge, manifested in the form of bloody, brownish or greenish discharge with a pronounced unpleasant odor;
- disruption of the urinary system, for example, cystitis;
- burning and itching in the vaginal area.
The cervical region of the uterus is susceptible to various pathologies, and their symptoms are nonspecific. This means that infectious-inflammatory or oncological diseases can manifest themselves in the same way. Difficult childbirth, which led to severe deformation of the cylindrical neck, should be a reason for more careful monitoring of the organ.
There are several main types of diseases that affect the cylindrical shape of the neck with the presence of deformations. First of all, this is erosion or ectopia, characterized by a violation of the integrity and structure of the mucous membrane. Precancerous conditions are also identified, in which atypical cells appear in the epithelium. If such pathologies are not treated in a timely manner, it means they can develop into malignant tumors. The extreme stage of the disease is when the tumor has spread to other vital organs.
The cervix is an important functional part of a woman's reproductive system. Its conical or cylindrical shape, as well as the degree of opening of the cervical canal, are important signs for clarifying the duration of pregnancy, as well as determining whether a woman has given birth or not. This means that it is by the condition of this organ that the gynecologist can determine the general condition of the genital organs and detect pathological processes.