Age-related hormonal changes in the female body cause the development of menopause. This condition is characterized by the absence of ovulation, the disappearance of menstrual bleeding, and the inability to conceive and bear a child. The occurrence of endometrial hyperplasia during menopause poses a danger to a woman’s health, since this pathology is highly likely to cause the appearance of malignant uterine tumors.
What is menopause and when does it occur?
Menopause is the 12-month period after the last natural periodic discharge in women, occurring between the ages of 45 and 55 years. It is caused by depletion of the follicle supply. If menopause occurs before the age of 40, then this process is called ovarian wasting syndrome. Some women experience late menopause - after 55 years.
There are cases when the pause is caused artificially. In this case, a woman stops menstruating due to surgical removal of the ovaries, chemotherapy, or medication.
During menopause, the female body changes. The changes are caused by a lack of hormones and changes in the functioning of the ovaries. It is at this time that the risk of developing many gynecological pathologies, such as uterine cancer and endometrial hyperplasia, increases.
General information about the disease
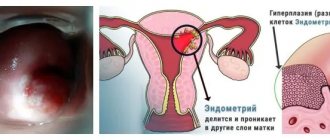
By the term “hyperplasia,” doctors mean tissue proliferation. It occurs due to excess cell production. The endometrium is the inner lining of the uterus. It provides the fetus with optimal conditions for full development. Each menstrual cycle, the thickness of the endometrium changes. The thinnest layer occurs immediately after the end of menstruation. During ovulation, the endometrium thickens up to 8 mm under the influence of the hormone estrogen. If conception does not occur, the level of hormones decreases due to the production of progesterone, the internal mucous membranes of the organ are depleted, the egg leaves the body - menstruation begins.
During menopause, hormonal levels are disrupted. Under the influence of increased levels of estrogen, the endometrium increases in volume. Due to the reduced level of progesterone, this process does not stop. In most cases, endometrial growth is characterized by premenopause. Indeed, despite the presence of monthly discharge, age-related changes occur in a woman’s body, accompanied by changes in hormonal levels.
Manifestation of hyperplastic processes in the postmenopausal period
With the onset of the postmenopausal period, the level of sensitivity to hormonal changes in the female body increases in the endometrium. Along with increased sensitivity, in the female body there is a noticeable decrease in the immune system of protection against the occurrence and development of various pathological processes. Moreover, by this period the woman had already suffered many different diseases and had more than one chronic disease.
Therefore, it is during the postmenopausal period in the female body that the likelihood of degeneration of hyperplastic processes in the endometrium into a cancerous tumor increases to a critical level.
As mentioned above, the main symptom of hyperplasia in the endometrium during the postmenopausal period is the occurrence of hemorrhages that are not typical for this period.
The highest risk of developing a pathology such as GPE in the endometrium is observed among the female half of humanity with the following conditions:
- the presence of a large number of extra pounds;
- development of mastopathy or uterine fibroids;
- hypertensive processes;
- development of diabetes mellitus;
- use of hormonal monopreparations containing only estrogens;
- hereditary factor;
- liver dysfunction;
- early or late onset of menopause;
- early onset of the menstrual cycle (up to 14 years).
It is worth noting that taking oral contraceptives, which include equal concentrations of estrogen and progesterone, have a positive effect on the functioning of the female reproductive system and do not cause the development of hyperplastic processes in the endometrium.
Endometrial norms
During menopause, the endometrium becomes thinner. Its thickness varies within 5 mm. Doctors consider this indicator to be normal. Sometimes the growth of the endometrium during menopause reaches 7-8 millimeters. This indicator indicates the possible onset of a pathological process, but is not yet classified as hyperplasia. For some patients, tissue thickness of 7-8 millimeters is the norm. But doctors recommend periodically undergoing ultrasound (every 3-6 months) in order to exercise dynamic control over tissue proliferation.
If the endometrial thickness reaches more than 8 mm, gynecologists recommend that the patient undergo a curettage procedure. It is necessary to confirm the development of the pathological process, study the tissue structure and prescribe treatment.
Classification of the disease
There are several types of endometrial hyperplasia. They differ in the direction of tissue growth:
- Glandular hyperplasia of the endometrium is diagnosed if the layer of the inner lining of the uterus increases due to modification of the glands located in it. The increase in volume occurs in the direction of the muscles of the organ.
- Cystic form. Cystic formations begin to form in the cavity of the membrane. This type of pathology is dangerous, since cells produced by excess hormones can degenerate into malignant ones.
- Basal hyperplasia. During menopause, this form of the disease is rarely diagnosed. During its development, an increase in the thickness of the basal layer of the uterus is observed.
- Focal form. The thickness of the membrane increases unevenly, forming growths (polyps) on the walls of the uterus.
- Atypical hyperplasia. During menopause, this type of pathology is rare. It is the most dangerous of all types of manifestations of the disease, as it quickly turns into uterine cancer. If an atypical form of endometrial hyperplasia is confirmed, doctors remove the organ.
Most often, glandular and cystic forms of the disease are diagnosed during menopause. The main reasons for the development of these types of pathology is hormonal imbalance.
What types of hyperplasia are there?
The types of endometrial hyperplasia in menopause depend on which mucosal cells predominate in the abnormal formation.
Classification.
Experts identify the following types of disease:
- Glandular - the mucous membrane grows towards the tissues of the uterus due to an increase in the size of the glands located in it. In this case, their shape is disrupted.
- Cystic - due to the fact that the cells of the mucous membrane overlap the glands, they begin to swell and form cysts. The likelihood of this type of disease degenerating into oncology is very high.
- Focal (polypoid) - polyps (growths on a thin stalk) grow from gland cells, around which separate areas (foci) of endometrial growth appear.
- Atypical (adenomatous) - due to the rapid change in the shape and size of the cells of the mucous membrane, the endometrium very actively grows into the tissues of other organs. This form of the disease is very dangerous because it turns into cancer in a short period of time. During menopause and postmenopause it is quite rare, since hormonal changes lead to a slowdown in all processes occurring in the body.
- Basal is a very rare type of disease in which cells of the basal layer of the endometrium grow deep into the tissues of the uterus.
A woman may develop a combined type of disease. For example, glandular cystic hyperplasia. In this case, in addition to the growths of the mucous membrane, which consist of glandular tissue, cysts and nodules are formed.
Causes of hyperplasia during menopause
There are several factors that cause endometrial hyperplasia to develop during menopause. In most cases, they begin to form even before the onset of menopause (premenopause).
- Hormonal disbalance. This is the most common cause of the development of pathology. In women over 45 years of age, there is a decrease in progesterone production and increased estrogen levels. This imbalance provokes modification of the lining of the uterus.
- Metabolic disease. With age, most women develop the problem of excess weight. Fatty layers of tissue provoke the production of estrogen, thereby exacerbating the hormonal imbalance that manifests itself during menopause.
- Failure of the endocrine system. For this reason, endometrial hyperplasia is often observed in postmenopausal women.
- Frequent invasions of the uterine cavity (gynecological operations). Due to frequent mechanical stress, the membrane receptors stop responding to progesterone levels. The more abortions and curettages a woman had to endure, the higher the likelihood of developing GGE in the climatic period.
- Predisposition to pathology at the genetic level. Doctors confirm that this disease is more often diagnosed in patients whose relatives have encountered the same problem.
Also, proliferation of mucous membranes is observed against the background of fibroids and mastopathy. In some cases, pathology can be caused by a malfunction of the immune system.
Treatment of endometrial hyperplasia in menopause
During menopause, endometrial hyperplasia is not treated without curettage. At the first stage of treatment, hysteroscopy and separate diagnostic curettage are necessary. Then they move on to choosing a hormonal drug, but before prescribing it is necessary to make sure that there are no contraindications, which include:
- thrombophlebitis and thromboembolic complications;
- malignant formations of the mammary gland, thyroid gland;
- history of myocardial infarction and angina pectoris;
- cerebrovascular accidents;
- hepatitis and chronic calculous cholecystitis.
Treatment differs depending on the type, form of hyperplasia and period.
During the perimenopause period (premenopause, menopause and the first year after), for the treatment of glandular endometrial hyperplasia without atypia and polyps, drugs are prescribed for 6 months, with ultrasound monitoring after six months and a year:
- progestogens (medroxyprogesterone, desogestrel, dydrogesterone);
- antigonadotropic drugs (danazol, gestrinone);
- GNRH agonists (goserelin, buserelin).
But it is difficult to choose a drug at this age due to the presence of common extragenital diseases.
When atypical endometrial hyperplasia is detected in menopause, preference is given to surgical intervention, but if there are contraindications, hormonal treatment is used, but in higher dosages:
- gestagens;
- GNRH agonists.
After 2-3 months, an ultrasound is performed and an aspirate is taken from the uterine cavity with a cytological examination. After 6 months, diagnostic curettage is indicated under hysteroscopy control. The woman has been under clinical observation for at least 2 years.
Note!
Each group of drugs has a number of side effects, so the duration of therapy is determined only by the doctor.
Curettage in menopause with endometrial hyperplasia
The most common manipulation for hyperplasia is curettage of the uterine cavity and cervical canal of the cervix for diagnostic and therapeutic purposes. Thanks to histological examination of the taken material, cancer cells can be detected in the early stages, which increases the effectiveness of treatment and prognosis.
If curettage is carried out without endoscopic observation, then there is a possibility of incomplete removal of the polyp, so hysteroscopy is the most successful option.
If the endometrium is thickened, the contours of the uterine cavity are uneven, and inclusions are detected, hysteroscopy and separate diagnostic curettage with mandatory histological examination of scrapings are indicated.
If, during a postmenopausal period lasting more than 5 years, a thickening of up to 6-7 mm is detected, an endometrial biopsy and ultrasound are indicated once every 3-6 months.
Unfortunately, surgical treatment is often resorted to; the extent of the operation depends on the type of hyperplasia and the presence of atypia.
In perimenopause, with recurrent endometrial hyperplasia without atypia in combination with adenomyosis or uterine fibroids, surgical intervention is performed. If a relapse is detected in postmenopause, then endometrial ablation is performed or the uterus and appendages are removed.
In case of atypical hyperplasia in postmenopause, the uterus and appendages are removed. In the presence of severe concomitant pathology and a high risk of surgical treatment, gestagens are prescribed continuously for a long time in combination with anticoagulants, antiplatelet agents and hepatoprotectors in usual dosages. Treatment is carried out under ultrasound control and aspiration biopsy after 6-12 months. Dispensary observation for life.
Folk remedies for endometrial hyperplasia in menopause
Alternative medicine has also found its admirers, although doctors do not use such methods as the main treatment - they can only be used as an addition to therapy.
During menopause, with endometrial hyperplasia, various herbal infusions are recommended:
- nettle;
- aloe;
- celandine;
- hog uterus;
- burdock;
- vegetable juices (for example, carrot, beetroot) and many others.
Herbs are easy to use - they are either poured with boiling water or prepared as decoctions and tinctures over a fire.
To treat glandular endometrial hyperplasia in menopause, some people practice clay in the form of compresses on the lower abdomen. This procedure is ineffective and even harmful due to the pronounced thermal effect.
Note!
Before any procedure, you should consult your doctor.
Vladlena Razmeritsa, obstetrician-gynecologist, especially for Mirmam.pro
Signs
Symptoms of endometrial hyperplasia in postmenopause manifest themselves individually. The main sign of a hyperplastic pathological process is bleeding. But they are not observed in all patients. Sometimes thickening of the membrane occurs without discharge. Other manifestations of the disease include:
- Very painful menstruation. In this case, the pain is spastic in nature.
- Irregular menstrual cycle. Sometimes spotting appears twice in a month.
- Heavy and prolonged periods (10-14 days).
Sometimes symptoms of uterine endometrial hyperplasia are accompanied by general malaise, insomnia, migraine, decreased performance, and irritability. The woman feels very thirsty.
How does the disease manifest itself?
Often, hyperplasia does not manifest itself during menopause. This is the main danger of the pathological process. For a long time, a woman may not even be aware of the progress of a precancerous disease.
If menopause has already arrived, but bleeding has resumed, this is an alarming symptom.
The deviation has no characteristic symptoms. Sometimes signs may appear that are similar to other gynecological diseases. In premenopause, the condition may manifest itself as disruptions in the menstrual cycle. Unscheduled bleeding may also occur periodically.
How to diagnose
In most cases, suspicion of endometrial hyperplasia is diagnosed by a gynecologist, to whom a woman approaches with complaints of painful or irregular menstruation. There are several methods for diagnosing the disease:
- Ultrasound. If during this diagnostic study it is discovered that the thickness of the endometrial layer is 7-8 mm, the gynecologist will prescribe an additional examination.
- Hysteroscopy. During the procedure, the doctor makes a visual examination of the uterine cavity using endoscopic equipment. The examination is carried out under general anesthesia. In most cases, a tissue biopsy is performed simultaneously with the examination of the membrane.
- Curettage (diagnostic curettage of the endometrium). The procedure is prescribed in cases where the thickness of the growing tissue exceeds 8 mm. Curettage is performed to further examine the endometrium and exclude the appearance of cancer cells.
If the thickening exceeds 10 mm, gynecologists recommend undergoing a separate curettage procedure, followed by irradiation of the organ cavity with radioactive phosphorus. The reagent is injected into the patient’s vein, migrates throughout the body and accumulates in pathogenic areas of the membrane. The doctor takes biological material from these areas for histological examination.
How is prevention carried out?
To prevent hyperplasia, you need to regularly visit a gynecologist for preventive examinations. In addition, doctors recommend:
- lead a healthy lifestyle;
Food should be healthy
- eat well;
- give preference to moderate physical activity;
- exclude any physical activity.
Menopause is a difficult period for every woman. That is why it is important to carefully monitor your health at this time.
Drug treatment
It is recommended to treat endometrial hyperplasia with medications if the tissue thickness does not exceed 6-7 mm. Therapy is based on taking hormonal medications that provoke an increase in progesterone levels. The patient must undergo a routine ultrasound throughout the entire treatment period (6-8 months of constant medication use), during which the doctor constantly monitors changes in tissue growth indicators.
Drug treatment does not give 100% results. The likelihood of relapse of the disease on hormonal drugs is high.
Causes
Menopause is characterized by the fact that various factors lead to endometrial hyperplasia, but the main cause of pathological tissue proliferation in the uterus is hormonal imbalance - an increased concentration of estrogens that stimulate the endometrium against the background of progesterone deficiency (the hormone of the second half of the monthly cycle).
The causes of hormonal imbalance are the following factors.
- Overweight . Fat cells have the ability to produce estrogens, that is, increase their level in the blood. At the same time, the concentration of progesterone decreases.
- Transition from reproductive function to menopause. During this period, natural hormonal changes occur.
- Incorrect use of hormonal drugs . Pathology may occur due to the use of drugs for the treatment of breast cancer or other diseases.
- The presence of polycystic ovaries is a hyperplastic transformation of organs with the replacement of their cells with connective tissue that synthesizes atypical estrogens. The proliferation of ovarian tissue causes a lack or excess of hormones produced.
- Thyroid diseases . Endocrine diseases such as diabetes mellitus, thyrotoxicosis, and thyroiditis do not directly affect the increase in estrogen production.
- Genetic predisposition . Scientists have proven that there is a connection between genetics and the characteristics of menopause.
- Mechanical injury to the uterus . Frequent abortions, surgical interventions, and cleansing help reduce the body's perception of progesterone and accelerate the growth of endometrial tissue.
- Pathologies of the adrenal glands . Problems with organs lead to metabolic disturbances.
- The presence of tumor formations in the uterus . Fibriomas and fibroids disrupt the normal nutrition of the organ.
- Liver disorders . Decreased production of sex hormone binding globulin leads to the appearance of free estrogen cells.
Surgical
If drug therapy does not produce the expected results, surgical treatment of the pathology is performed. Depending on the results of preliminary tests, one of the surgical intervention methods is used:
- Curettage of the uterine cavity. Recommended if the thickness of the modified tissue exceeds 10 mm. The procedure lasts 30-40 minutes under local anesthesia.
- Cauterization. This method of surgical intervention is used for focal hyperplasia. During the procedure, the doctor acts on the foci of modified tissue with cold, laser or electrical impulses.
- If there is an increased risk of developing malignant tumors, doctors recommend removing the uterus. During the hysterectomy procedure, the organ is completely removed. And if a woman’s ovaries are damaged during menopause, they are also removed during surgery.
Which type of surgical intervention to use is determined by the attending physician individually. Hormone therapy is sometimes used in preparation for surgery. It promotes rapid recovery of the body after intervention.
What treatment is used
Endometrial hyperplasia in menopause requires treatment using traditional medicine. Since the disease can degenerate into cancer, women should not try to treat it only with folk remedies. They can be taken as an addition to the main treatment, but only after consultation with your doctor.
Popular TV show host Elena Malysheva, in a program dedicated to the treatment of endometrial hyperplasia, emphasized that if you suspect the disease, you must immediately consult a doctor and undergo a comprehensive examination.
The optimal treatment method is chosen only by the doctor, depending on the stage of the disease and the general health of the patient. Treatment with traditional recipes will only take up precious time and lead to excessive growth of the endometrium.
Medication method
And another classification.
This method involves treatment with hormonal drugs that contain progesterone. Taking medications can last about six months.
During the course of treatment, women constantly undergo ultrasound to determine the thickness of the endometrium. Based on the results of the examination, the attending physician adjusts the dose of medications.
It is strictly forbidden to self-medicate. When a woman independently increases or decreases the dosage of the drug, she can provoke a relapse of the disease.
To alleviate the lady’s condition, the doctor may prescribe additional herbal medicine. After completing treatment, a woman needs to undergo an ultrasound scan every 3-6 months to monitor the condition of the endometrium.
Operative method
If a woman experiences a relapse of the disease after taking a course of drugs, then a surgical method is used to treat endometrial hyperplasia. In postmenopause, the disease is treated using both methods.
The following surgical options are possible:
- Curettage (curettage) is prescribed to patients whose endometrial thickness exceeds 10 mm. The operation is performed under local anesthesia and lasts approximately half an hour. Fragments of the removed endometrium are necessarily sent for histological examination in order to identify cancer cells. If the result is positive, a decision is made to remove the uterus.
- Cauterization – gives maximum effect when there are separate foci of the disease. I perform cauterization in several ways: cold (cryodestruction), electric current (diathermocoagulation) or a laser beam (laser destruction).
- Hysterectomy – involves amputation of the uterus. If the ovaries are also affected by the disease, they are removed along with the uterus. This method is used when the uterine tissue is very deeply affected or adenomatous endometrial hyperplasia is detected, which can lead to the development of cancer.
Surgical treatment of endometrial hyperplasia in postmenopause is used when a woman has polyps or atypical cells that are highly likely to develop into cancer.
This disease can develop into cancer.
Additional therapy with folk remedies
Most patients are in no hurry to use traditional treatment for pathology, preferring to use traditional medicine recipes. Gynecologists advise not to regard herbs as the main therapy, but to use them in combination with medications. The most common traditional medicine recipes that have proven effective in treating HPE are:
- Fresh juice from burdock root and golden mustache. These liquids are mixed in equal proportions and taken twice a day, 1 tablespoon. A significant drawback of this recipe is the possibility of carrying out therapy only in the warm season.
- Alcohol tincture of nettle (prepared independently). 200 gr. 500 ml of medicinal raw materials (fresh leaves and sprouts) is poured. alcohol (strong moonshine). Keep for three weeks in a warm, dark place, periodically shaking the container with liquid. The finished infusion is filtered and taken 1 teaspoon twice a day.
Treatment with folk remedies should be accompanied by regular examination by a doctor. This will make it possible to monitor the dynamics of the disease.
Price
The cost directly depends on the treatment regimen, drugs and methods used. Additionally, the price will be affected by the survey. For example, a biopsy will cost 5,000 rubles, curettage of the uterus – 6,000 rubles, ultrasound – up to 1,000 rubles. If laser treatment or cryodestruction is planned, the overall price will increase significantly, since these are expensive technologies. To alleviate the condition of endometriosis, folk remedies are used, for example, flaxseed oil, infusion of boron uterus or nettle. The price of herbs is low.
Is relapse possible during menopause?
The possibility of recurrence of endometrial hyperplasia during menopause increases. Depending on the type of treatment chosen by the doctor, after which the tissue proliferation continued, further actions are determined:
- If the disease recurs after drug therapy, and the thickness of the layer increases by more than 8 mm, it is recommended to undergo a curettage procedure.
- If the situation repeats after curettage, the uterus is completely removed.
The percentage of recurrent cases of pathology with initially well-chosen treatment is low. To prevent the possibility of relapse, the patient must undergo regular follow-up examinations.
Diagnostics
Diagnosis of pathology during premenopause is carried out by a gynecologist. The specialist examines the patient on a gynecological chair, after which he decides on further examination.
To carry out a complete diagnosis, the following methods can be used:
- Ultrasound of the genital organs, as well as transvaginal ultrasound. Using a special sensor that is placed inside the vagina or on the abdomen, the specialist measures the size of the endometrium and examines the uterine cavity for the presence of other formations (fibroids, fibroids, cysts).
- Hysteroscopy. The procedure involves collecting a small amount of epithelium for histological analysis. Prescribed only when the thickness of the endometrium is more than 6 mm.
- Conducting a hormonal study. Venous blood is donated and the content of important hormones for the functioning of the female reproductive system is determined.
Only an experienced specialist can detect endometrial hyperplasia in premenopause. It is impossible to independently determine the type of disease and the stage of its development.