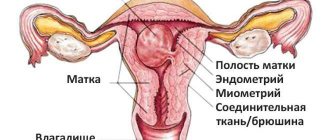
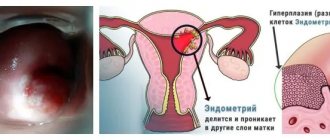
Endometrial hyperplasia (thickening of the glandular layer of the uterine epithelium) requires timely and appropriate treatment, regardless of the patient’s age, stage and form of the disease. An effective method for removing pathologically changed areas of the mucosa is diagnostic curettage. With its help, you can not only get rid of the affected endometrium, but also conduct histology of the taken material.
The operation of endometrial curettage is usually performed by a gynecologist under the control of a hysteroscope. The latter is an optical system that is equipped with a light source and has a special channel for introducing surgical instruments into the uterine cavity. The use of a hysteroscope during diagnostic curettage allows for high-quality cleaning of the endometrium with complete removal of pathologically altered areas and polyps, preventing re-growth of the glandular layer.
After surgery, the removed endometrium is sent for histological examination. Based on the test results, as well as taking into account the form of hyperplasia, the patient’s age, the presence of concomitant diseases and the desire to preserve reproductive function, the gynecologist prescribes treatment. Maintenance therapy after surgery suppresses the regrowth of the pathologically altered glandular layer and stabilizes the woman’s hormonal levels.
Diagnostic cleaning is performed under general anesthesia. The operation is prescribed on the eve of menstrual bleeding or in the first days. Diagnostic curettage under the control of hysteroscopy is an effective and, most importantly, absolutely safe manipulation.
When to expect your period after curettage: signs of complications
The female body recovers differently after intervention in the reproductive system. But menstruation after curettage must begin at a certain time. Therefore, it is necessary to know when to expect menstruation, what it will be like, and what indicates the occurrence of irregularities.
When to expect menstruation after curettage
If curettage does not produce any complications or unexpected consequences, menstruation may occur within 4–5 weeks. The beginning of the cycle is counted from the date of curettage.
But even doctors are not able to say when exactly your period will start after curettage. Everything will depend on the female body’s ability to recover and the reasons for the operation. Minor delays and premature bleeding are allowed. Normally, these deviations do not exceed 3–5 days.
The maximum permissible period of absence of menstrual flow is two weeks. The exception is abortion and miscarriage. After them, the cycle can take a long time to recover and the first menstruation after a miscarriage or abortion will be delayed by 1-2 months.
The second, third and subsequent menstrual bleeding occurs on time. If the cycle disturbance continues to bother the woman, then it is necessary to conduct additional diagnostics and tests. The following may cause a failure:
- external negative factors;
- consequences of scraping;
- new diseases;
- violation of gynecologist's instructions.
The doctor can guess when your period will start after cleaning the uterus. The specialist takes into account the nature of the pathology, the general health of the patient and the specifics of the intervention. The date is calculated approximately, since a deviation of several days is allowed for any woman, regardless of surgical intervention.
How long does the discharge last?
The duration of bleeding should remain within normal limits. Menstruation, which lasts from three to seven days, should not cause concern. But it is important to take into account the intensity of the discharge and its characteristics before surgery.
If heavy bleeding continues for a week, you should consult a doctor. The same situation occurs during short periods, when only spotting occurs, reminiscent of the end of menstruation.
Nature and quantity of discharge
The first periods after curettage come according to the usual schedule and have the same characteristics:
- natural shade;
- normal amount;
- usual duration;
- minor pain.
Modification of monthly bleeding is allowed only for the better. After all, the purpose of cleaning or scraping is aimed at eliminating disorders of the reproductive system. Therefore, women who are accustomed to heavy or long periods mistake positive changes in the cycle for pathology.
Menstrual flow as a result of curettage can:
- maintain your usual volume;
- become meager;
- increase your number;
- develop into bleeding.
In a normal situation, the change in the amount of discharge is positive due to the elimination of a negative factor (disease). You should be alarmed by spotting on the pad or heavy bleeding.
Cycle after diagnostic curettage
The easiest way is to determine when your period will come after a diagnostic curettage. Minimal tissue trauma and quick recovery times have virtually no effect on the cycle.
You need to pay attention to the reason for diagnostic curettage:
- uterine bleeding;
- failure of the menstrual cycle;
- cycle without ovulation;
- suspicion of endometrial neoplasm;
- other violations.
Problems with menstruation may arise if the following pathologies were confirmed during diagnosis:
- polyp of the endometrium or cervical canal;
- proliferation and thickening of endometrial tissue;
- cancer diseases;
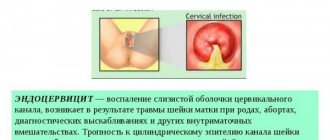
- endometritis;
- endometriosis;
- benign formation in the uterus;
- pathology of the cervix.
The best option in such circumstances is separate diagnostic curettage (SDC). The first day of the cycle in this case is the date of the procedure.
Menstruation after an abortion or frozen pregnancy
After abortive curettage, menstruation may begin within a few months. A similar situation arises when eliminating a frozen pregnancy. The female body needs more time to recover due to severe stress and hormonal imbalance.
When your period starts after an abortion depends on the method of the operation. Blind curettage is fraught with severe tissue damage or incomplete removal of the embryo. Therefore, recovery of the body may take longer. Vacuum abortion is safer for women.
Delayed menstruation or bleeding after curettage (abortion, miscarriage) can be caused by several factors:
Hormonal disbalance
The female body begins to suffer from restructuring, even if conception did not end with the birth of a child. The gynecologist may also prescribe hormonal oral contraceptives to prevent pregnancy during the recovery period.
Non-compliance with recommendations
It is necessary to take care of your health. Any violation of the doctor’s instructions can cause inflammation, infection and other negative factors that cause menstruation to be delayed.
Poor cleaning
If during the intervention the specialist left fetal particles in the uterine cavity, then severe bleeding and cycle disruption cannot be ruled out. That is why such procedures need to be carried out with modern instruments that allow you to control the entire process so that particles of the fertilized egg or placenta do not remain inside.
Menstruation after endometrial cleansing
When, after cleaning the endometrium with hyperplasia, menstruation begins, largely depends on the experience of the doctor who performed the curettage. In a normal situation, menstrual flow begins no earlier than a month after the intervention.
The delay is most often caused by:
- Deep impact. During the operation, only the functional layer of the mucosa is removed. If the doctor also touched the basal layer, there is a possibility of prolonged recovery and absence of menstruation.
- Hormonal therapy. For hyperplasia, hormones are prescribed that control the functioning of the ovaries. While taking medications that reduce estrogen synthesis, you should not expect menstrual periods. They will begin when the gynecologist cancels the therapy.
- Other factors. A delay can be caused by stress, taking antibiotics, the disease itself, or non-compliance with recommendations. Complications cannot be excluded, which will be signaled by a prolonged absence of menstrual flow.
Knowing when menstruation will begin after cleaning the uterus, and why cycle disruptions may occur, it is easier for a woman to monitor changes in the reproductive system. If the delay does not disappear after stopping hormonal pills, then you need to go to the hospital. After all, hyperplasia is an insidious disease, at the last stage of which even the uterus is removed.
Disorders after surgery
The following menstruation is a reason to go to the hospital:
- too abundant;
- scanty;
- with an unpleasant odor;
- no discharge.
Heavy periods
The appearance of heavy periods after curettage indicates complications.
Heavy bleeding (one pad is not enough for an hour) can be caused by:
- uterine atony;
- incomplete curettage;
- the remainder of parts of the placenta or fertilized egg;
- endometrial detachment;
- uterine perforation;
- uterine tear.
The main symptoms are decreased performance, fatigue, dizziness, pale skin and low blood pressure.
No discharge
When there is no menstruation after curettage, the reasons may be as follows:
- Onset of pregnancy. Even after such an intervention, conception is possible. Doctors advise avoiding sex until the body recovers and then using contraception.
- Damage to the mucous membrane. A damaged endometrial layer is one of the most dangerous complications. The uterine lining does not regenerate, which is why menstruation does not last for a very long time.
- The occurrence of inflammation. After curettage it is necessary to take antibiotics. The absence of these medications causes inflammatory processes, discharge with an unpleasant odor, high body temperature, and retention.
- Formation of hematometra. Due to cervical spasm or scarring, menstrual blood accumulates in the uterine cavity. Therefore, doctors often prescribe antispasmodics to patients to prevent such a complication.
A woman needs to know how many weeks after cleansing her period begins. A long delay is not the norm, so if alarming symptoms appear, you should consult a doctor and not self-medicate or read the forum. Only in this case will it be possible to avoid complications and serious problems with the reproductive organs.
Source: https://MesyachnyeDni.ru/menstruaciya/beremennost/mesyachnye-posle-vyskablivaniya.html
User comments
as soon as the bleeding stops, wait for your first period, drink it on the first day
Here's another read, the gynecologist writes, maybe it will be useful
» Qlaira belongs to the class of NOCs - natural oral contraceptives - and contain two types of hormones. One of them, estradiol valerate (E2B), is converted into the hormone estrogen after entering the body. And the second (progestin) has a beneficial effect on the endometrium and reduces the level of male hormones, thereby improving the condition of the skin and hair. The effect on the endometrium leads to a decrease in menstrual flow. Several studies have shown the same numbers - as a result of taking Qlaira, the volume of blood loss is reduced by more than 70%. This in itself is convenient for any initial situation, and for women suffering from heavy and prolonged periods, it is simply a salvation. In such cases, Klaira will help maintain both quality of life and performance.
The tablets are taken daily, without breaks. The wafer contains 26 active tablets and 2 “pacifiers”, which is very convenient for controlling your cycle. A dynamic dosing regimen is used: depending on the day of the cycle, the level of one hormone in the tablets gradually decreases and the level of another increases.
The contraceptive effectiveness of Qlaira is very high - pregnancy occurs in only 3.4 women out of 1000 who took the pills. The studies were conducted among women aged 18 to 50 years. The Pearl Index of 0.34 is a very good indicator of reliability.
Thus, Qlaira is a unique drug that will solve not only the issue of contraception, but will also facilitate menstruation.
source
Recommendations after uterine curettage - Human health, symptoms and treatment of diseases
The period after curettage of the uterine cavity requires a special approach on the part of the doctor and responsible implementation of all recommendations on the part of the patient. The reproductive and physical capabilities of the female body are not limitless, therefore, an important task of the gynecologist who has performed uterine cleansing is considered to be complete, careful observation and provision of a protective regime.
In the period after cleansing the uterus, experts identify three main areas of work for complete rehabilitation:
- Prevention of infections.
- Restoration of the endometrium and menstrual cycle.
- Restoring physical and mental health.
To achieve these goals, gynecologists give recommendations in terms of taking antibacterial drugs, oral contraceptives, limiting physical activity, maintaining sexual rest and performing general strengthening measures.
How you feel after cleaning
Not everyone is able to quickly get into the usual rhythm of life, resume sports and exercise. Recovery time largely depends on the individual characteristics of the body.
After curettage, moderate abdominal pain, mild anesthesia-related dizziness, and moderate bleeding are usually noted.
In the professional training of workers, fast and high-quality work, and also in the fact that the main task of our company is to create a comfortable life for clients. You can choose any air conditioner from us.
Also, you may not forget that there is a sale of air conditioners in Sevastopol at the best price! We offer a large number of brands, colors, and most importantly, with us you can choose an air conditioner design that will only be a decoration for your home.
Restoration of the uterus after curettage, both therapeutic and diagnostic, lasts one menstrual cycle, the whole body - from 2 to 6 months.
General health after curettage:
- Body temperature up to 37.2-37.3 is considered normal in the first 2-3 days.
- Moderate abdominal pain lasts up to 7 days.
- Slight dizziness is acceptable.
Discharge after cleaning procedure:
- The first few days there is discharge from the genital tract in the form of fresh blood, as during menstruation.
- A week after the curettage, the discharge takes on a sanguineous character: it becomes mucous and has a brown color due to the admixture of altered blood.
- The restoration ends with yellowish discharge, which gradually takes on a classic appearance: scanty, mucous discharge, which, when dried, takes on a yellowish tint.
- The normal duration of discharge during the recovery period is 10-12 days.
The next menstruation after curettage should begin 25-45 days later.
Normally, the first day of menstruation should occur after a period of time equal to the length of the cycle before cleaning (provided that it is regular).
What you should pay attention to and when you need to seek help from medical professionals if a woman has undergone curettage:
- Long-term (more than 20 days) bloody discharge.
- Scanty or heavy menstruation, spotting not associated with menstruation in the long term after curettage. These symptoms may indicate the development of cervical endometriosis or hormonal imbalance.
- Unpleasant smell of discharge.
- The discharge looks like “meat slop”.
- Increased discharge with light physical activity.
- Pain in the lower abdomen that lasts more than a week after curettage.
- An abrupt cessation of discharge after uterine curettage, which may indicate the accumulation of clots in the cavity of the organ (hematometer).
- Heavy bleeding.
- Increased body temperature.
- Loss of consciousness.
The above symptoms may indicate the development of endometritis.
The severity of some purulent-inflammatory diseases of the internal genital organs after curettage may not correspond to the clinical picture and laboratory parameters.
That is why it is extremely important to be under the supervision of a doctor if there are even minimal signs of infectious complications.
How dangerous is the period after the procedure?
The uterine cavity after cleaning is an extensive wound surface. The lion's share of recommendations after curettage will be aimed at preventing microorganisms from entering the cavity of the operated organ. Gynecologists are aimed at preventing the development of inflammation of the reproductive organs and its chronicity.
Experts identify two groups of risk factors for the development of infectious complications after uterine curettage:
- Main group. This category includes women with a history of endometritis, chronic recurrent chlamydia, urea and mycoplasmosis, candidiasis, human papillomavirus infection, and persistent vaginal dysbiosis. In such patients, the likelihood of developing purulent-inflammatory diseases in the gynecological area during curettage is most likely. Patients are subject to the closest attention from doctors. This also includes emergency cases of curettage.
- Additional group. Patients who had uterine cleansing due to bleeding (endometrial hyperplasia), miscarriage, curettage of placenta or ovum remnants have a lower risk of infectious complications compared to the main group.
Women who have undergone diagnostic curettage have the lowest risk of developing infectious complications. Typically, this type of study is carried out in cases of infertility of unknown origin, in preparation for IVF, suspected polyps and subserous fibroids, and menstrual irregularities.
Factors that indirectly influence the period after curettage:
- Obesity.
- Diabetes.
- Anemia.
- Hypothyroidism.
The above diseases have an indirect effect on the course of the recovery period of curettage, but their presence significantly reduces physical strength, the body's resistance to infections and slows down the healing processes of the wound surface in the uterus after curettage.
The most common infectious complication after curettage is endometritis, an inflammation of the inner layer of the uterus.
The causative factor of the disease is the opportunistic vaginal flora (staphylococci, streptococci, E. coli), as well as representatives of the pathogenic flora, if the patient before the operation had untreated sexually transmitted infections - chlamydia, ureaplasmosis, mycoplasmosis, gardnerellosis and others.
That is why, in the period after therapeutic curettage, gynecologists recommend taking antibacterial drugs without fail, regardless of the infectious history. After diagnostic cleaning, you can limit yourself to taking sulfonamides.
According to statistics, the incidence of endometritis after uterine cleansing is 20%.
Purulent-inflammatory diseases of the genital area do not always appear after curettage due to non-compliance with the doctor’s recommendations. Nosocomial infection is still relevant today. A woman should choose modern clinics with rich obstetric and gynecological experience.
Poor quality cleaning can result from the penetration of endometrial cells into the cervical tissue, which leads to endometriosis.
Doctors' recommendations
General recommendations:
- Sexual activity is excluded for 3 weeks after cleansing. The goal is to prevent infectious complications and bleeding. In addition to bacteria, semen contains prostaglandins that relax the uterus.
- It is recommended to use a condom for 6 months after curettage to prevent pregnancy.
- You should not take a bath or visit the pool for a month.
- It is not recommended to use tampons to absorb blood after curettage. This can provoke the development of inflammatory processes in the uterine cavity.
- After curettage, physical activity should be limited as much as possible.
Recommendations for taking antibiotics and other medications during curettage:
- Antibacterial medications must be taken strictly at regular intervals.
- Minimum duration of taking antimicrobial agents: 3 days for Azithromycin and 5 days for other drugs.
- The dosage of the drug should correspond to the patient’s weight.
- Drinking alcohol while taking antibiotics is not recommended.
- To relieve pain, you should take Ibuklin or Diclofenac.
- To prevent the formation of adhesions, enzyme preparations (Wobenzym, Longidaza) are usually prescribed.
If the recommendations of the gynecologist have not been announced, then the above advice must be followed.
Restoring menstrual function is an important part of the rehabilitation period after curettage. The cyclical work of the female body is very sensitive to various fluctuations and outside interference.
“Artificial” getting rid of the endometrium sends incorrect signals to the main regulators of the menstrual cycle - the hypothalamus and pituitary gland. The ovaries, as performers, will also respond to this type of influence.
After curettage, doctors’ recommendations for restoring the cycle come down to prescribing oral contraceptives.
The drugs must be taken for 2 to 6 months, depending on the diagnosis that served as the reason for cleaning the uterus.
Read also Polycystic ovary syndrome - causes, symptoms, treatment, complications
Oral contraceptives after the uterine cleansing procedure:
- Jess.
- Logest.
- Belara.
- Janine.
- Silhouette.
- Novinet and others.
The first tablet is taken on the day of curettage. The selection of the drug is carried out only by a gynecologist and based on the results of a blood test for hormones.
After curettage, it is recommended to resume physical activity no earlier than after 2 months. Visiting the gym should be delayed, and heavy lifting (more than 3 kg) and running should be avoided. Any physical activity is stressful for the body, which undoubtedly reduces immune activity and will interfere with healing.
One of the important recommendations of a gynecologist after curettage is the implementation of physiotherapeutic measures. The most effective methods of physiotherapy in gynecology include:
- EHF therapy. The therapeutic effect is achieved through irradiation with electromagnetic waves in the EHF range, which increases the nonspecific resistance of the body, increasing resistance. It is recommended to use EHF therapy after cleansing to prevent endometritis.
- Ultrasound therapy. The method is recommended for preventing the formation of adhesions in the uterus and pelvis resulting from curettage.
- Phototherapy. Infrared rays have an anti-inflammatory effect.
After curettage manipulation, many experts recommend using sorption therapy as a preventative measure, the essence of which is the introduction into the uterine cavity of a special solution that has sorbent and antiseptic properties. Usually a mixture of Enterosgel and Dioxidin is used.
The composite solution is injected into the uterus using a thin catheter. Due to its thick consistency, the mixture does not leak, so no special restrictive recommendations for physical activity are required. Aspiration biopsy is used to monitor healing.
The aspirate is examined under a microscope and the condition of the resulting cells is assessed.
After the uterine cleansing procedure, doctors monitor the healing process using aspiration biopsy. It is carried out on days 23-25 of the cycle, 2 months after all types of curettage.
Artificial termination of pregnancy by curettage for medical reasons is a strong stress factor that negatively affects the adaptive and compensatory capabilities of the body.
An equally important task facing the gynecologist is to provide comprehensive rehabilitation using means aimed at restoring psycho-vegetative disorders.
As a rule, after curettage, the patient is recommended the following therapeutic measures and medications:
- Acupuncture.
- Psychotherapy.
- Herbal soothing infusions for 2 weeks after cleansing (Phytosedan, soothing teas with lemon balm, sedative infusions).
- Antidepressants (Coaxil, Gelarium, Azafen) for 10-20 days.
The problem of purulent-inflammatory diseases in gynecological practice after curettage continues to be one of the leading ones. Complete, adequate prescriptions and the patient’s compliance with them during the recovery period guarantee the complete absence of consequences and complications in terms of reproductive function.
Source: https://mediccare.ru/montazh-i-puskonaladochnyie-rabotyi-sistem-konditsionirovaniya.html
Best answers
Nonsense. Anesthesia during cleaning is not general, but intravenous. The drugs used for this provide only a short-term anesthesia effect (10-15 minutes), do not have a deep inhibitory effect on the central nervous system, do not have a toxic effect on the body and are not harmful to brain cells. I won’t say that they are useful, but their purpose for cleaning is quite justified; they are used for short-term interventions. (to avoid painful shock during operations) Therefore, everything will be fine, don’t worry.
I had surgery on my right eye 4 times) it’s not dangerous. It’s true that after anesthesia the recovery is so severe, after one operation I couldn’t take a shit for 2 days)
It’s better, of course, not to do anesthesia at all. but during cleaning they give a short-term anesthesia, which is not dangerous.
they lived...nowadays they call murder a purge, that's where you belong, girl...what else are you going to clean up there? I'm fine
Type in the search engine anesthesia for abortion. There your answer is not here.
It’s not even anesthesia, it’s just amnesia for a few minutes. The heart has nothing to do with it. Smoking, drugs and alcohol take your life, not momentary amnesia.
Tell the anesthesiologist about your weak heart, he will choose the best option for you. Well, in general there is a light anesthesia, for an hour maximum. Don’t be afraid, an injection into a vein, a mask on the face - and it’s all the same
There the whole cleaning takes 5 minutes - they look at the cavity with an LED and cut off what is not necessary. no waste - go home in the morning
Do you think that live surgery is better for the heart? This is a terrible pain.
I don’t want to scare you, a week ago I had an allergic reaction to anesthesia, so now I’m very afraid of anesthesia.
Nowadays, anesthesia is gentle and doctors should first check your tolerance
Cleaning is not always an abortion. There is such a thing - hyperplasia, the walls of the uterus grow, thicken and need to be cleaned. A friend of mine had this operation under general anesthesia for three years in a row. The doctor must decide this based on the results of the heart examination. Just don’t hide this problem, God forbid.
I call a frozen pregnancy a cleanse...
How to take birth control pills to avoid getting pregnant?
Any girl or woman with an established menstrual cycle can start taking birth control pills. This method of contraception, when used correctly, provides an almost 100% guarantee of protection against pregnancy. Failure to follow the instructions and recommendations of the doctor reduces the contraceptive effect. In order not to harm your health, you need to take the pills correctly and complete the course.
Types of birth control pills and mechanism of action
Based on their composition, birth control pills are divided into two groups:
- estrogen-gestagen, or combined oral contraceptives (COCs). These include most drugs, for example, Jess, Yarina, Regulon, Novinet;
- pure gestagens are Charozetta, Laktinet and Modell Mam.
The mechanism of action of the two groups is the same. Due to gestagens, the synthesis of the pituitary hormones FSH and LH is blocked, which normally contribute to the maturation of the egg and ovulation.
An additional contraceptive effect is provided by thickening the cervical mucus, reducing peristalsis of the fallopian tubes and reducing the thickness of the endometrium.
Therefore, if ovulation occurs and conception occurs as a result of unprotected sex, the embryo will not be able to implant into the wall of the uterus.
But COCs contain an estrogenic component. It does not have a contraceptive effect and is necessary to maintain ovarian function and control the menstrual cycle. But it is ethinyl estradiol that is associated with the majority of side effects and contraindications.
Attention! Taking birth control for the first time without a doctor's prescription is dangerous. Only after examination by a gynecologist can you choose the appropriate remedy.
Rules for taking birth control pills
Before you start taking hormonal birth control pills, you should visit a gynecologist to make sure there are no contraindications. The examination consists of a gynecological examination, taking a smear for oncocytology, and studying the medical history. Blood clotting tests and biochemical studies will also be required.
The doctor selects the drug, taking into account concomitant gynecological pathologies. It is necessary to specifically select a product in the following conditions:
- nulliparous girls;
- with endometriosis;
- polycystic and functional ovarian cysts;
- somatic pathologies;
- for problems with the thyroid gland, diabetes;
- in the postpartum period.
It is not recommended to independently replace a drug prescribed by a doctor. This will lead to side effects.
On what day can you start a course of birth control?
The best day to start taking birth control pills is the first day of menstruation. at this time, hormones are at a minimum level, and there is confidence in the absence of pregnancy.
drink one tablet from the pack every day, moving along the arrow. If you follow the rules of administration, you do not need to take additional protection in the first cycle.
the contraceptive effect develops within 7 days, so ovulation has time to slow down.
It is allowed to start taking birth control pills on the 3-5th day of your period . but with this scheme, during the first half of the cycle you need to protect yourself with a condom. Without waiting for your period to start, you can start taking birth control pills in the following cases:
- after an abortion;
- after curettage of the uterine cavity;
- with spontaneous miscarriage in a short term.
in this case, the pills are necessary not only as a means of contraception, but also to restore the menstrual cycle.
Taking birth control pills before your period starts is not recommended. A doctor can prescribe such a regimen for dysfunctional bleeding and other gynecological pathologies and irregular cycles.
Do I need to strictly adhere to the appointment time?
It is recommended to take hormonal pills at any time of the day, but adhere to an interval of 24 hours. This is the period during which the components of the drug are metabolized in the body and gradually its concentration in the blood begins to decrease. if a slight time shift occurs, this will not reduce the effectiveness of the drug, but it is better not to allow deviations of more than an hour.
The best time to take birth control pills is considered to be 8-9 a.m., regardless of meals. The medicine is well absorbed on a full stomach or on an empty stomach. It is not contraindicated to take pills in the evening, but the morning hours are considered more suitable due to the natural daily increase in hormones.
Should I take a break from taking birth control pills?
It was previously believed that taking hormonal contraceptives for a long time was harmful to the body. they were considered the culprits of ovarian hyperinhibition syndrome.
But such side effects were typical for large doses of hormones; in modern drugs they are minimal.
Sometimes after finishing treatment, women do not have periods, but this condition often occurs in patients with pathology of the menstrual cycle, which was present before the start of the course.
birth control pills are taken without interruption for several years, until the woman plans a pregnancy (for more details, see here). If you suddenly stop taking it, on the contrary, the likelihood of unplanned conception increases. this is due to the rebound effect: after a long rest, the ovaries begin to function especially strongly, often several eggs mature.
what to do if you miss a pill?
You take birth control pills every day, you can’t skip pills. if the time for taking it is missed, you need to focus on the number of the tablet in the pack and the period that has passed since the last pill you drank. missing up to 12 hours is relatively harmless. a woman needs to drink the drug as soon as possible, and take the next dose at the usual time.
If 24 hours have passed since the forgotten contraceptive pill, proceed as follows:
- tablet number up to 7 - take 2 doses at once, and the next one at the usual time, use a condom until the end of the cycle, pre-ejaculatory withdrawal of the penis is ineffective;
- tablets numbered 8-14 - take 2 tablets at once, and at normal times - 1, additional contraception is not needed;
- from 15 to 21 tablets - take the forgotten one and continue to use the tablet as usual.
if there are 28 contraceptive pills in a package, then the last 7 tablets, colored in a different color, are pacifiers . If you skip them, you don’t have to worry about your health and, after a forgotten dose, switch to a new pack. But you can’t start taking new birth control pills in the middle of your cycle.
How to stop using oral contraceptives correctly?
Women who start taking birth control pills from the group of combined oral contraceptives after their period are advised to wait until the end of the package, even if it is one month of use. exceptions are severe complications and side effects that result from the use of the drug.
those to whom the doctor has prescribed progestin contraceptives can stop taking the pills on any day of the cycle without harm to health. this will allow the menstrual cycle to resume normally and avoid complications of use.
When is it permissible to quit a started pack of birth control pills?
Contraceptives can be produced in various combinations of estrogens and gestagens:
- monophasic - in them the concentration of hormones is the same in all tablets;
- biphasic - in a monthly package, the concentration of hormones changes in the second phase, but currently these drugs are not used;
- three-phase - in a package of 3 types of tablets with different doses, often used in women approaching menopause.
monophasic contraceptives have less effect on the cycle than others. You can stop taking birth control pills halfway through the pack. but three-phase tablets are taken to the end, with the exception of allergic reactions and severe side effects.
How to move the day of menstruation?
Oral contraceptives allow you to influence the day on which menstruation begins. some resort to them in order to delay its onset. this can be done in several ways:
- To start taking hormonal pills, choose the 5th day of your period, so the next menstruation will begin a week later;
- after finishing a pack of 21 tablets, do not take a break for 7 days, but immediately start a new pack.
the latter method will shift menstruation to a full cycle, after which a week-long break is taken. but frequently using such methods to correct menstruation can result in hormonal imbalance.
In order to take birth control pills correctly, it is necessary to take into account their compatibility with other medications, including antibiotics. some antibacterial drugs may reduce the concentration of ethinyl estradiol in the blood. a lack of estrogen will not lead to a decrease in the contraceptive effect, but can lead to breakthrough bleeding and disruption of the menstrual cycle.
It is not recommended to combine contraceptives with antibiotics from the tetracycline and penicillin groups. Clarithromycin and erythromycin can, on the contrary, increase plasma concentrations of hormones.
Therefore, women who need treatment for vaginal inflammation should give preference to drugs in the form of suppositories.
in other cases, if possible, the doctor should prescribe alternative antibiotics to avoid drug interactions.
which reduces the efficiency of the spinner
Hormonal drugs undergo several stages of hepatic metabolism. Therefore, they may be affected by medications that stimulate or inhibit liver enzymes. The effectiveness of COCs is reduced when used simultaneously:
- tinctures, decoction of St. John's wort;
- barbiturates;
- azole antifungals;
- protease inhibitors used to treat HIV;
- grapefruit juice.
Alcohol in small quantities does not significantly affect the metabolism of hormonal contraceptives, but with alcohol abuse, adverse reactions increase.
Smoking is not recommended for women using COCs. It affects blood clotting and promotes the development of thrombotic complications. After 35 years, COCs with estrogens are not suitable for smokers, but taking gestagenic contraceptive drugs is allowed (for more details, see which COCs to take after 35).
The effectiveness of contraception decreases with indigestion. If you vomit within 2-3 hours after taking the tablet, you need to repeat the dose. Diarrhea also accelerates peristalsis and removes unabsorbed drug.
Precautionary measures
Having correctly chosen the day of the menstrual cycle for the first dose of OK, you may encounter the appearance of spotting bleeding on the 14th-15th day. A small amount of blood is released, which indicates addiction to the drug. Sometimes bleeding occurs in unexamined women with endometrial hyperplasia or polyps. To avoid this, you need to visit a gynecologist before purchasing the medicine.
A delay in menstruation while taking contraceptives does not always indicate pregnancy; sometimes it is a consequence of an incorrectly selected dosage. Therefore, stop taking the pills until the reasons are established.
Some women worry that hormones are disrupting their metabolism. It is possible to gain weight while using modern contraceptives, but this is a rare side effect. If your weight starts to increase, you need to change your contraceptive.
COCs are sometimes used as emergency contraception, where a large dose of pills is taken at short intervals. This method can be used if there are no other contraceptives at hand, but it will not help cause a miscarriage; pregnancy cannot be frozen with this treatment.
Advice from gynecologists
To take hormonal pills correctly, you need to follow the instructions for the prescribed drug. Then the effectiveness of contraception will be maximum. But a consultation with a gynecologist is necessary if there is a severe reaction to the drug.
It is not always associated with contraindications to taking COCs, but may be the result of an incorrectly selected medication. To improve the condition, a change in drug is required.
Undesirable reactions such as spotting in the middle of the cycle, breast tenderness are an indicator of addiction to the drug during the first 2 months, and later require replacement of the COC.
Source: https://ProKontraceptivi.ru/pill/kak-prinimat/
Answers from experts
I will not be lazy to write in detail about my experience. It might come in handy) My third pregnancy was frozen. Moreover, the fetus froze at 6-7 weeks, and I reached the 12th week. Without even guessing about anything. Only at the scheduled ultrasound I was “delighted”. I won’t describe the psychological side. And it’s so clear: it couldn’t have been worse (Basically. The cleaning was done on the same day. It doesn’t hurt at all. Of course, they give you anesthesia. An hour later you wake up in the room. A little fun getaway) You meet women who have similar diagnoses. There was no pain. And there is little blood. And this should have alerted me. The doctors said nothing. I was discharged on the third day. They gave free antibiotics. I took the course
It is important! And two days after being discharged, blood poured out of me like a bucket. I have never seen so much blood in my life. I woke up in a pool of blood and the pad was wet within 5 minutes! I was seriously scared! I thought that was it, I would never give birth again
Again the ambulance, again the same department in the hospital. Diagnosis: hematometra. Something was blocked there, and the blood was not coming out as it should. Again anesthesia and repeated cleaning! Again the same girls - hello))) Then even huge clumps came out of me. I woke up the doctors on duty in the middle of the night. She made everyone hesitate. But it’s better this way than to be infertile later)
CONCLUSION: after cleaning and before discharge, insist on an ultrasound! To avoid such an outcome! And it’s also important! What they didn’t tell me at the hospital either! Immediately after cleansing, start taking birth control! Because I didn’t start drinking them, a cyst formed on my ovaries. And then we treated it with a paid good gynecologist
After cleaning, in any case, the reproductive system should rest. So pills are a given. Although I didn’t tolerate them well. Cleaning is equivalent to menstruation, and you can start taking the normal pills within 7 days.
The period after cleaning the uterus
The period after curettage of the uterine cavity requires a special approach on the part of the doctor and responsible implementation of all recommendations on the part of the patient. The reproductive and physical capabilities of the female body are not limitless, therefore, an important task of the gynecologist who has performed uterine cleansing is considered to be complete, careful observation and provision of a protective regime.
In the period after cleansing the uterus, experts identify three main areas of work for complete rehabilitation:
- Prevention of infections.
- Restoration of the endometrium and menstrual cycle.
- Restoring physical and mental health.
To achieve these goals, gynecologists give recommendations in terms of taking antibacterial drugs, oral contraceptives, limiting physical activity, maintaining sexual rest and performing general strengthening measures.