A disease such as uterine tuberculosis is a manifestation of the genital form of the disease. It is always secondary, and in 90% of cases it occurs simultaneously with the pulmonary form, much less often with the intestinal form, very rarely there are forms when this pathology occurs in the female body in parallel with the corresponding bone disease. In recent years, scientists have noted an increase in the number of genital tuberculosis. However, most researchers believe that it is premature to talk about an epidemic or a sharp increase in the number of such cases. Most professionals assume that the reason for the discussed leap is in improving the quality of diagnostic equipment.
The fact is that tuberculosis of the genital organs always occurs quite secretly. Especially if the transfer of the disease occurs against the background of appropriate therapy. Women may complain of changes in the menstrual cycle, mild pain in the lower abdomen, but most attribute such symptoms to manifestations of the main diagnosis. A fairly characteristic symptom is infertility, but this sign does not help to identify the disease: few women with health problems, and quite serious ones, decide to purposefully have a child.
Causes of the disease
The causes of uterine tuberculosis are the entry of Koch's bacillus into a woman's body with its subsequent spread from the primary focus to the genitals.
The disease develops when several conditions are met:
- a certain amount of mycobacterium tuberculosis that entered the body did not die (this is possible due to insufficient activity of the immune system);
- bacteria have entered the respiratory system or (very rarely) the intestines;
- at first, due to sufficient activity of the nervous, cardiovascular, immune and endocrine systems, the bacterium could not cause disease;
- then, against the background of various diseases, the bacteria began to spread throughout the body, or the primary focus in the lungs began to heal, and Koch bacilli infected the genitals.
How is the infection transmitted?
The bacterium that causes this disease enters the body through airborne droplets. So it enters the bronchi, and then the lungs. This is confirmed by the discovery in 15-20% of women of “traces” of the disease in the form of thickening of the pleura, foci of calcium accumulation, and enlargement of intrathoracic lymph nodes. The tuberculosis bacillus enters the internal genital organs from the lungs through the bloodstream or through the lymphatic vessels.
In some cases, infection of the uterus occurs through the intestines. Mycobacteria enter the intestines during pulmonary tuberculosis, when sputum coughed up is swallowed, or when contaminated foods are consumed.
Tuberculosis of the female reproductive organs does not occur every time an inflammatory focus occurs in the intestines, lungs or peritoneum. The spread of infection to the genitals can be provoked by: pregnancy, childbirth, severe stress, hormonal and immunodeficiency diseases.
The likelihood that Koch's bacillus will land on the uterus increases if a woman suffers from chronic inflammation of the uterus (endometritis) or appendages, if she has already had menstrual irregularities (irregular, painful, scanty or heavy periods), uterine surgeries, or abortions.
Infection through sexual contact (from a partner who has genital tuberculosis) is extremely unlikely. Most scientists who have studied this issue have come to the conclusion that the mucous membrane of the external genitalia, vagina and lower cervix will reject Koch's bacillus.
Most cases of the disease develop in childhood, but the first signs of uterine tuberculosis can be noticed only during the formation of menstruation. The disease is diagnosed mainly at 20-35 years of age.
Consequences
Even cured tuberculosis of the reproductive system is fraught with negative consequences for the body, among which are most often noted:
- Uterine bleeding.
- Formation of abscesses in the abdominal cavity.
- Formation of fistulas and adhesions.
- Infertility.
- Chronic pain.
- Spread of tuberculosis infection to nearby organs.
Tuberculosis of the fallopian tubes is a serious disease that requires long-term and difficult treatment. Only by following all the doctor’s recommendations and completing the course in full is it possible to preserve reproductive function, and not everyone can do so.
Classification
According to the nature of its course, tuberculosis of the genital organs can be acute, subacute and chronic. The acute course of the process is observed extremely rarely, mainly when a secondary infection occurs. In 15-17% of cases, subacute tuberculosis is observed, when inflammation is not so active. The chronic variant is the most common.
There are also different activities of the tuberculosis process in the genitals. So, in the first 2 years it is considered active, the calming stage lasts 2-4 years, and the inactive stage lasts as long as desired. The last stage is also called a consequence of tuberculosis. If in the first 4 years from the moment of the disease its symptoms become more pronounced, this is called an exacerbation. When the same phenomenon develops after the first 4 years, it is a relapse of uterine tuberculosis.
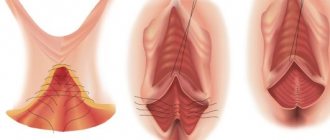
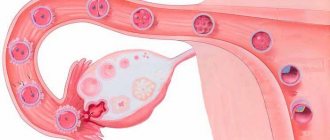
There is also a classification that takes into account the localization of the process. So, there may be tuberculosis of the uterine appendages, and it occurs more often - in 90-100%. This is due to the fact that the fallopian tubes receive nutrition from two arteries - the uterine and ovarian, which branch into many branches. The blood flow in such vessels is slow, and this allows Mycobacterium tuberculosis to settle in tissues fed by small-diameter arteries. And this is mainly the mucous membrane of the fallopian tubes.
Separately, tuberculous lesions of the uterine body are registered in 25-30%. It can involve only a section of the inner lining of the organ (focal endometritis), the entire endometrium (total endometritis) and even spread to the muscular lining of the organ (metroendometritis).
Inflammation of other structures develops quite rarely: the cervix - in 0.8-6%, the ovaries - in 6-10%, the vagina or external genitalia - in less than 0.4% of cases, and is considered a criterion for late detection of the process.
Depending on what picture the histologist finds in the biopsied tissue, uterine tuberculosis is:
- Chronic with productive changes: cells at the site of inflammation grow and divide, which is why tubercles (lupomas) appear on the mucous membrane.
- Subacute with exudative-proliferative changes: cells not only divide, but also secrete inflammatory fluid - exudate.
- Caseous, when the death of a section of tissue looks like a white cheesy mass that crumbles easily. Such tissue changes are typical for acute and severe forms.
- Complete, in which the foci of inflammation are saturated with calcium salts (calcified) and are themselves limited to the capsule.
How to treat genital tuberculosis in women
Treatment of tuberculosis of the genital organs in a woman is carried out by a phthisiogynecologist, taking into account the stage, localization, previous treatment, and concomitant pathology. The course of treatment is long, from 6 months to 2 years, and the regimen usually includes 3 anti-tuberculosis chemotherapy drugs. List of antibiotics with antituberculosis activity:
• Isoniazid; • Rifampicin; • Pyrazinamide; • Streptomycin; • Ethambutol, etc.
Reserve antibiotics include Kanamycin, Amikacin, Ofloxacin and Lomefloxacin
. All medications negatively affect liver function, so hepatoprotectors, multivitamins, and general tonics are additionally used.
It is important to normalize the work and rest regime, high-calorie nutrition with a sufficient content of proteins, vitamins and other useful microelements. There are sanatoriums that specialize in the treatment of genitourinary tuberculosis.
Physiotherapeutic methods of treatment for genital tuberculosis include the following:
• amplipulse. • pelvic diathermy; • electrophoresis with hydrocortisone. • sinusoidal currents.
It should be noted that the main method of treating tuberculosis remains long-term chemotherapy with anti-tuberculosis drugs. Hormone therapy can be used to normalize menstrual function.
Clinical picture
Acute course
Symptoms of uterine tuberculosis depend on the nature of the inflammation. So, in an acute case, a woman notices constant pain in the lower abdomen. They intensify if you perform electrophoresis with anesthetic medication, magnetic therapy or other physical procedure. In addition, there is an increase in body temperature, weakness, and night sweats.
The pain in the acute form of the disease can be so severe that doctors diagnose appendicitis, ovarian apoplexy, ectopic pregnancy, and operate on the patient. And if the form of the disease is such that during the operation the death of parts of the uterus is visible, the surgeon removes them and sends them for histological examination. This way a correct diagnosis can be made and treatment prescribed.
If, while conducting an intraoperative examination of the abdominal organs, the surgeon does not see any changes and does not perform any removals, then tuberculosis may not be diagnosed for a long time.
Subacute course
Subacute course implies not intense, but constant pain above the pubis. This is due not only to inflammation, but also to the fact that it becomes difficult for the intestines and pelvic organs to contract due to their movement being constrained by scars and adhesions. The temperature rises to 37.2-37.3°C, but may remain within normal limits. General weakness, fatigue and loss of appetite are alarming, but given the rhythm of life of a modern woman, this rarely leads to a visit to a doctor and further diagnosis.
Chronic process
With tuberculosis of the uterine body, which has a chronic course, the woman may not be bothered by anything (slight fatigue, periodic increases in temperature to small numbers are attributed to a viral infection, stress, work). Only infertility can prompt her to start testing. It may not develop immediately: a woman may have time to have an abortion or give birth to a child (and this can provoke the spread of tuberculosis to the genitals).
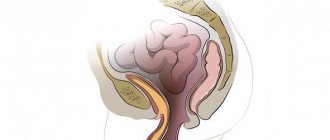
Most cases of infertility are due to the fact that, due to the peculiarities of local circulation, the tuberculosis bacterium is the first to enter the fallopian tubes and cause inflammation. Proceeding for a long time and unnoticed, it causes a narrowing of the oviducts, as a result of which the egg cannot pass into the uterine cavity and become fertilized. The patency of the fallopian tubes can be impaired when it is filled with cheesy masses formed by one’s own dead cells.
Pregnancy also does not occur if the tuberculosis process has led to partial or complete fusion or scarring of the uterine cavity.
About half of women with uterine tuberculosis experience menstrual irregularities. Usually these are scanty and short periods (3-4 days), the interval between menstruation is 35 days or more. There may be a long absence of menstrual flow. A tendency to uterine bleeding is not typical for this inflammation.
Cervical tuberculosis is a complication of inflammation of the uterine body. It develops more often in older women after the endometrium of the uterine body has died with the formation of cheesy masses, and the inflammatory process has moved to the myometrium. There are no specific symptoms that distinguish cervical tuberculosis. The disease can be diagnosed during colposcopy in the form of productive (formation of tubercles) or ulcerative (ulcers are visualized) forms.
Forecast
The success of therapy is determined by many factors:
- Timely diagnosis.
- The effectiveness of treatment.
- The power of immunity.
- The absence of concomitant chronic inflammatory diseases of the reproductive system.
- A woman's attitude to the doctor's recommendations.
The earlier tuberculosis is detected, the higher the chance of complete cure without serious consequences. But, given that the symptoms in the first stages are practically not expressed, it can be assumed that a fairly large percentage of patients are then diagnosed with infertility.
In 5-7% of cases, relapses of the disease are observed.
Establishing diagnosis
Diagnosis of tuberculosis of the uterus or other reproductive organs is extremely difficult. This is explained by the fact that tuberculous inflammation does not have any special symptoms, is not “heard of” by gynecologists, and is also rarely detected by standard bacteriological cultures of vaginal discharge and is not always noticeable even during surgery.
You can suspect it only if you have a long and thorough conversation with the woman, and it turns out that she was in contact with a person with tuberculosis, or in childhood and adolescence she often suffered from diseases of the bronchi or lungs (especially if diagnoses such as bronchoadenitis or pleurisy were made).
How to identify a disease using instrumental and laboratory methods?
The following will help in diagnosis:
- X-ray or computed tomography of the lungs: they reveal accumulations of calcium in the lungs, enlarged thoracic lymph nodes, which indicates a previous tuberculosis process.
- Examination on a gynecological chair. A sedentary and fixed uterus may be revealed; if the appendages are affected, the doctor can palpate them in the form of enlarged, painful and lumpy cords.
- Tuberculin test: tuberculin is injected under the skin, after which changes in the appearance of the cervix (according to colposcopy), body temperature, pulse, and abnormalities in blood tests are noted.
- Cultures of vaginal discharge or menstrual blood.
- Hysterosalpingography - x-ray of the uterus and appendages after preliminary filling with a contrast agent.
- Diagnostic curettage of the endometrium, which is carried out 2-3 days before menstruation.
- Laparoscopy is a method where a hole is made in the anterior wall of the abdomen through which video equipment is inserted, allowing one to examine the uterus and appendages and take a biopsy.
Diagnostic methods
When identifying genital tuberculosis, diagnostics pays great attention to the patient's medical history. The phthisiatrician prescribes a special tuberculin test if the patient has previously been diagnosed with the following diseases:
- lungs;
- upper respiratory tract;
- pleurisy;
- pulmonary form of tuberculosis.
The response is then assessed.
Contraindications to performing a tuberculin test are:
- renal failure;
- diabetes;
- open form of pulmonary tuberculosis.
A positive test is different:
- increased temperature;
- more frequent heartbeat;
- changes in blood composition.
Carrying out tests can cause serious negative changes in the patient’s health.
Important! A gynecological examination does not reveal the presence of genital tuberculosis.
In addition, diagnosis is carried out using:
- bacteriological smear examinations;
- endometrial scrapings from the cervix;
- PCR (polymerase chain reaction);
- laparoscopy (during it, in addition to the actual assessment of the condition of the peritoneum and genital organs, material is taken for histology, sometimes during laparoscopy additional adjustments are made to the consequences of genital tuberculosis: adhesions are removed, tubal patency is restored);
- X-ray studies may be ordered to make an accurate diagnosis.
Therapy
Treatment of uterine tuberculosis is carried out in anti-tuberculosis dispensaries. It includes the prescription of specific antibiotics (Isoniazid, Streptomycin), drugs that gently stimulate the immune system, and vitamins (anti-tuberculosis antibacterial drugs cause vitamin deficiency in the body).
Without fail, a woman should begin to eat a balanced and healthy diet, get enough rest and walk in the fresh air.
If fistulas appear in the reproductive organs, areas of caseous necrosis have formed in them, or the uterine cavity is filled with pus, an operation is performed. Surgical intervention is also used if there are adhesions and scars in the uterine cavity so that the woman can become pregnant.
The course of treatment necessarily includes physiotherapy and spa treatment.
Risk factors
We can distinguish a category of women who are at risk:
- Diagnosed with Hodgkin's lymphoma.
- If you have AIDS.
- Taking steroid hormones.
- Undergoing therapy with drugs that suppress the immune system.
You can also note risk factors that, if there is a predisposition to such a disease, only increase the likelihood of its development:
- Monotonous and poor nutrition.
- Contact with tuberculosis patients.
- Chronic inflammatory diseases of the reproductive organs, for example, endometritis, inflammation of the ovaries.
- History of tuberculosis of any location.
- Disrupted menstrual cycle.
The combination of several factors significantly increases the risk of developing tuberculosis.
Treatment
The disease is treated exclusively inpatiently, in specialized medical institutions. This process is quite lengthy (from six months to several years) and labor-intensive. The treatment regimen involves therapy in several areas:
- chemotherapy using three or more special drugs;
- physiotherapeutic treatment;
- surgical intervention (according to indications);
- restorative therapy, increasing general and local immunity.
We recommend watching a video about how tuberculosis is treated with chemotherapy:
During treatment, the patient must:
- maintain a daily routine;
- get adequate rest and nutrition;
- take vitamins.
Incorrectly selected treatment for genital tuberculosis can cause significant harm to the patient, so drugs are selected very carefully, taking into account all influencing factors. These include individual tolerance to drugs, the type and stage of the disease, as well as possible resistance of mycobacteria to the drugs used.
Surgical intervention is used in severe cases when conservative treatment has had no effect, or when the functioning of the pelvic organs is disrupted. The operation is not, in fact, a method of cure, since it does not destroy the pathogenic microorganisms themselves. After surgery, chemotherapy is continued.
For some forms of the disease, clinical guidelines prescribe symptomatic treatment. For this purpose:
- antipyretics;
- anti-inflammatory;
- painkillers;
- therapy for correction and restoration of the menstrual cycle.
In a small number of cases, women who have had genital tuberculosis regain their reproductive capacity. Physiotherapeutic treatment is carried out after the acute period. The following methods are used:
- phonophoresis;
- electrophoresis with the use of drugs;
- in some cases, homeopathy (the prescription of homeopathic remedies is aimed at eliminating the symptoms of the disease and is solely under the responsibility of the attending physician).
Important! Spa treatment is now considered insufficiently effective and unreasonably expensive. However, there is an opinion that mountain and sea air have a beneficial effect on the patient’s health.