In medical practice, calcifications are defined as deposits of calcium salts. Moreover, this can happen in the cavities of various organs. Calcifications are often found in the uterus.
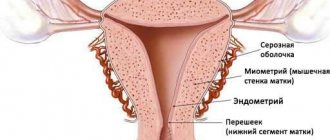
The uterus is an unpaired hollow organ that consists of three layers. The inner layer is the endometrial, represented by powerful muscles. The widest middle layer is the myometrium. The outer part of the uterine structure is the peritoneum.
Description
Calcifications in the uterus are many times more common than in the peritoneal layer or in the myometrium. They are also often found on the uterine cervix. In each of these cases, calcification represents a certain kind of protective reaction of the body. Salts, which have inorganic properties, encapsulate areas where tissue breakdown occurs. This prevents the spread of the necrotic process to other areas. The formation of calcium deposits is secondary in nature and is not a disease in the full sense of the concept.
Calcifications in the uterus are very common. Medical statistics report that calcium deposits form in approximately 30% of all women, and in most cases the process occurs without any external manifestations.
Reasons for education
All causes of calcium deposits can be divided into several groups. The first group includes the so-called trigger factors of occurrence, that is, those that directly determine the formation of calcification. Among them:
- Lesions of organs located in the pelvis are of a traumatic nature. Such lesions include, but are not limited to, diagnostic curettages, surgical abortions, hysteroscopies and other similar manipulations. They lead to an increased likelihood of invasion of uterine tissue by pathogenic microorganisms. The greatest danger is posed by abdominal surgeries performed on the organ.
- Predisposition to the development of infectious and inflammatory lesions of a genetic or other nature. For example, endometriosis or endometritis can develop under the influence of family history. If a woman has at least one sick relative in the ascending line in five generations, then the probability of calcification in women increases to 30%, but if there are two sick relatives, then the probability increases to 50%. Fortunately, the pathology is not inherited in a dominant or autosomal recessive manner. Only features of the reproductive system can be transmitted.
- Stenosis of the cervical canal and genital tract. Such disturbances cause reflux of menstrual blood and other secretions back into the uterine cavity, resulting in stagnation of these substances, which ultimately significantly increases the likelihood of developing an infectious lesion (most often endometritis).
- Poor environmental conditions in the woman’s place of residence. Under the influence of environmental factors, adenomyosis can develop, which is a risk factor for the accumulation of calcium salts.
- Menstrual irregularities. In the vaginal cavity there is a large number of different bacteria, some of which are pathogenic and can infect tissues and organs (human papillomavirus, herpes agents, mycoplasmas, ureaplasmas, staphylococci, streptococci and other representatives of pyogenic flora). When menstruation is delayed, blood stagnates, which contributes to the formation of an environment favorable for the proliferation of bacterial agents.
- Allergic reactions to exposure to internal and external factors. Most often, in such a case, a nutritional reason is meant, that is, improper nutrition and the entry of antigens into the systemic bloodstream.
- Excessively early or late onset of sexual activity. Both options are undesirable for women's health. With a late onset of sexual activity, the aggressiveness of microorganisms increases. If it is too early, dystrophic processes in the pelvic organs are initiated. As a result, the risk of calcifications increases.
- Late birth. They can have a negative effect on the condition of the uterus and often cause anatomical changes that can lead to the death of uterine tissue (complete, partial).
- Pathological changes in the endocrine system. These also include diabetes mellitus, disorders of the hypothalamus, pituitary gland, hyperthyroidism, hypothyroidism and other pathologies.
- Pathological changes in the reproductive system. First of all, the provoking factors are infectious diseases: adnexitis, endometritis and others.
- Scar on the uterus after cesarean section. Calcifications can occur on the scar, which arose as a result of abdominal surgery on the organ.
- Decreased local and general immunity. Unfavorable environment, stress, heavy physical activity (provoking excess production of corticosteroids), frequent viral respiratory diseases, hypothermia.
Treatment of phleboliths
Since the majority of stones develop asymptomatically, they do not require active treatment. Therapeutic correction is necessary in situations where phleboliths manifest clinically, cause hemodynamic disorders, and create a risk of complications. To solve these problems in clinical phlebology, the following methods are used:
- Sclerotherapy. Malformations and varicose veins, which are associated with most phleboliths, can be eliminated from the bloodstream by injecting liquid or foam-like sclerosant substances into the lumen of the vessels. To achieve a complete and stable result, several procedures must be performed. The most common is precision sclerotherapy under the control of imaging devices.
- Endovascular laser coagulation. The effectiveness of endovascular laser therapy administered through a venous catheter has been confirmed in the removal of stones. The minimally invasive percutaneous technique is often combined with sclerosant injections, which provides a faster therapeutic response. For multiple stones, laser coagulation is combined with surgical techniques.
- Phlebectomy. Typically indicated for lesions of superficial veins or mass-producing malformations in the pelvis. To facilitate removal of altered areas and reduce the risk of bleeding, it is performed after preoperative sclerotherapy.
- Selective removal of phleboliths. In various anatomical areas, stones are removed from open access under ultrasound, microscopic or manual control. The technique can relieve symptoms, but is usually performed in combination with other treatment options.
- Conservative therapy may include taking anticoagulants (low molecular weight heparins), non-steroidal anti-inflammatory drugs . To reduce congestion in the pelvic area, physical therapy exercises and an ascending contrast shower . The presence of free inclusions in the inferior vena cava requires implantation of a vena cava filter .
Indirect factors
The second group of causes of pathology usually includes factors that indirectly determine the beginning of the process of deposit formation. Among them are:
- Alcohol and tobacco abuse. These factors negatively affect the condition of tissues and immunity.
- Poor nutrition, which can lead to decreased immunity.
- Intense loss of calcium ions from bone structures.
- Obesity. Being overweight is an increased risk factor.
- Increased level of calcium salts in the blood. This situation is abnormal; it is fraught with the development of calcification not only in the uterus, but also in other organs and tissues. This factor is often a trigger for the formation of calcifications in the mammary glands, prostate gland, kidneys, lungs, and aorta. In this case, the uterus is damaged less frequently, but in each such case we can talk about multiple lesions of the organ.
- Stressful situations. Against the background of stress, general and local immunity decreases, as there is increased production of cortisol, adrenaline, and norepinephrine by the adrenal glands.
The listed factors are not the only ones that provoke the occurrence of calcifications. This should be taken into account when determining the etiology of the disease.
Symptoms
Calcifications in the uterus practically do not manifest themselves with any symptoms. The presence of weak nagging pain in the lower abdomen may indicate the process of salt deposition.
But, as a rule, in most cases, calcium deposits are discovered incidentally during studies for other pathologies or conditions. Most often, with calcification, symptoms of the underlying pathology are revealed, which became the provocateur of the formation of calcifications.
In this case, the list of possible symptoms is very extensive. Practice shows that the most common causes are endometritis and endometriosis. It is these two diseases that cause the onset of calcification.
An appointment with a gynecologist at the antenatal clinic should be made if there is a suspicion of the development of pathology.
Conclusion
Calcium formations in the uterus confuse women, causing certain difficulties in the functioning of the organ. Any measures to diagnose formations and their removal or treatment are agreed with the doctor. You should not self-medicate, since calcifications on a regular ultrasound can be confused with polyps.
When the corresponding formations are found during an ultrasound, women, for obvious reasons, become very interested: calcifications in the uterus, what it is, whether it is a diagnosis, how dangerous it is. In most cases, the gynecologist will say that this condition in itself is not a disease. This is a consequence of the disease, chronic inflammatory processes. Calcifications often form at the site of injury, for example, after complications arising from a difficult birth. Sometimes they are confused with polyps, so a correct diagnosis is fundamentally important here.
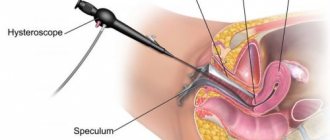
Calcifications are deposits of calcium salts localized in a specific part of the uterus. It may appear at the site of formation of fibromatous nodes; more specific information can be obtained after hysteroscopy. During an ultrasound examination, it is only permissible to assert with some degree of probability that in this case we are talking about calcification.
Main signs of inflammation
The main signs of inflammation in the uterine mucosa are:
- Pain in the lower abdomen, which can be of varying intensity. When the process is complicated, shooting, aching, and pulling pains predominate. The severity of discomfort is directly dependent on the degree of aggressiveness of the main pathogen, the general state of the immune system, and the location of the lesion. Discomfortable sensations can radiate to the projection of the uterus, lower back, legs, and groin area.
- The appearance of bloody discharge that has an unpleasant odor. In some cases, which is extremely rare, the exudate may consist entirely of pus. As a rule, the discharge has a sharp putrid odor and the color of meat slop. They are abundant in nature.
- Disruption of the menstrual cycle up to a delay of a week. This situation is not normal.
- Increased body temperature to febrile or higher levels. If the disease is chronic, relatively mild hyperthermia may occur.
- Symptoms of general intoxication: vomiting, nausea, dizziness, headaches.
- Deviations in a woman's reproductive function. Fertility is not excluded, but may decrease.
Most often, calcium deposits occur against the background of long-term chronic endometritis, and therefore the clinical picture may be blurred. In such cases, an urgent appointment with a gynecologist at the antenatal clinic is required.
Types of research
Then a bimanual examination and examination of the genitals using mirrors are required. In addition, you need:
- General laboratory examination of blood samples to identify the classic picture of inflammation, accompanied by an increase in the level of leukocytes and their sedimentation rate.
- Biochemical study of venous blood samples.
- Examination of organs located in the pelvis using ultrasound. Uterine calcifications will be noticeable on ultrasound.
- X-ray of organs located in the pelvis. Both benign and malignant neoplasias can calcify.
- ELISA, PCR diagnostics. Allows you to identify the main causative agent of the pathology if it has an infectious etiology.
- Smears from the cervical canal, vagina.
- Bacteriological cultures for the presence of nutrient media.
These studies are sufficient to identify the root causes of calcifications. In some cases, CT and MRI are indicated.
Is it possible to remove calcifications in the uterine cavity? Let's figure it out.
Therapy
Calcifications cannot be treated. Treatment of the underlying pathology is necessary. Calcifications are not a disease; they do not pose a danger in themselves, but only indicate the presence of a disease. Calcified areas are not prone to progression, so you can not remove them, but live with them calmly.
Now it has become clear what calcifications are.
The onset of hormonal changes in the female body leads to a number of anatomical and physiological changes in many systems and organs. To a greater extent, women's reproductive organs, namely the ovaries and uterus, undergo changes during menopause. Let's take a closer look at what changes the female uterine organ undergoes with the onset of menopause.
Uterus during menopause
The main phases of menopause are premenopause and menopause, after going through which a woman begins a long period of postmenopause, which accompanies her throughout her entire subsequent life.
The premenopausal period is quite long: from 3 to 10 years. This period is characterized by changes in almost all organs and systems in the female body. They can appear in a more vivid form or, with timely treatment, in a smoothed form:
- psychological disorders;
- changes in thermoregulatory processes in the body;
- hormonal imbalance, accompanied by a deficient level of production of sex hormones;
- disturbances in the menstrual cycle, until its completion.
The menopausal period begins immediately after the last menstrual period and continues throughout the next year. It is believed that the end of menopause occurs after 12 months of absence of menstruation. During this period, involutional changes in the genital organs occur in the female body. Almost all reproductive organs begin to decrease in size, and even the uterus decreases in size during menopause. Not only the size of the genital organs decreases, but also the amount of cervical mucus, which subsequently has an important impact on the state of the microflora.
Moreover, during menopause, the overall level of resistance of the body to the effects of pathogenic factors decreases. Some organ systems begin to function less well, which leads to a decrease in the body's immune defense system.
Therefore, many women who have entered the threshold of menopausal changes are faced with various diseases, especially those related to the reproductive system.
Thus, in most cases, the occurrence of tumor-like processes in the area of the mammary glands and uterus is noted during menopause. Therefore, with the onset of menopause, it is necessary to regularly visit a gynecologist and undergo an annual examination. The main most dangerous pathological changes include:
- Inflammation of the uterus.
- Development of benign neoplasms in the uterine cavity.
- Development of a tumor-like neoplasm of oncological nature of the uterine organ.
- Breast cancer.
- Salpingitis or inflammation of the fallopian tubes.
- Endometritis.
- Vaginitis.
- Carcinoma.
- Fibroma, etc.
Clinical manifestations
Often, vein stones are present in the human body for years without any unpleasant symptoms. Their presence can be suspected if the patient develops diseases that contribute to the formation of calcifications. The most likely cause of phlebolithiasis is venous stagnation of blood. This condition in women is manifested by the following symptoms:
- constant aching pain in the lower abdomen, lower back, legs;
- spider veins on the thighs;
- heavy, prolonged menstrual bleeding, cycle irregularities;
- change in consistency and volume of vaginal secretion;
- swelling of the genitals.
Symptoms of pelvic calcifications in men are:
- reduced amount of prostatic secretion, reduced sperm volume, its consistency becomes more liquid;
- if calcification blocks the urethra, a disturbance in the urination process is observed;
- When the secretion of prostatic fluid stops, erectile function suffers.
Despite the fact that the presence of phleboliths is not accompanied by pronounced symptoms, this pathology requires close attention. In this case, it is necessary to identify and eliminate the causes that caused the development of calcifications.
Ultrasonography
Ultrasound of the uterus during menopause is prescribed as a standard examination of the pelvic organs and diagnosis of pathologies with symptoms similar to menopausal syndrome.
The ultrasound research method provides a fairly high level of information content, is safe and does not cause hostility.
Despite the fact that menopause is a natural process, for most representatives of the fair half of humanity it can cause a number of unpleasant symptoms and discomfort, expressed as follows:
- disruption of the regularity of the menstrual cycle, up to its cessation;
- occurrence of dizziness and headaches;
- sleep disturbances with the development of insomnia;
- hot flashes;
- dryness in the vaginal area;
- frequent urge to urinate;
- pain during sexual intercourse.
Sometimes women cope with these manifestations on their own, but most often the help of hormone replacement therapy is needed. To assess the condition of the woman's reproductive system, an ultrasound examination is performed using a transvaginal sensor.
During menopause, the norm of changes in the uterus, revealed by ultrasound, is as follows:
- Increased echogenicity (or density) of the uterus.
- Its anteroposterior size decreases.
- Severe atrophy of the endometrial layer.
- Formation of adhesions and synechiae.
During the menopausal period, ultrasound examination may also reveal the presence of fluid in the uterine cavity. This is sometimes perceived by specialists as the development of a polyp or hyperplasia of the endometrial layer, although in fact this is not the case.
The formation of this fluid may normally be a consequence of the process of overgrowth of the cervical canal associated with the aging of the female body. But this condition requires a mandatory additional research method by hysteroscopy, which will help to more accurately assess the benign quality of the processes occurring.
A diagnostic examination using ultrasound examination of the pelvic organs is of great importance for a woman’s life, as it helps to identify serious pathologies in the initial stages of development.
Especially considering the fact that mature women are more susceptible to pathological changes in the uterus, such as its enlargement during the development of oncology during menopause. The process of enlargement of an oncological tumor is sluggish and does not cause specific symptoms. And the appearance of uterine bleeding and pain in the lower abdomen are observed in later stages of the disease.
Therefore, it is so important not to ignore timely ultrasound, which will help identify and promptly begin appropriate treatment.
What do calcifications indicate?
Among other things, sometimes during ultrasound examination, experts note the presence of calcifications in the uterine cavity. And, therefore, all representatives of the fair half of humanity are interested in questions about what it is, what happens to the uterus when they are in it?
Almost all gynecological specialists do not classify the presence of calcifications in the uterine cavity as a separate disease, but consider it a consequence of the chronic course of an inflammatory process, such as salpingitis.
Calcifications themselves are deposits of calcium salts that are localized in a specific place in the uterine cavity. This usually occurs in the area of previous injuries, for example, after a complicated birth process. Also, these deposits can form at the location of fibromatous nodes.
A more accurate clinical picture can be obtained only after hysteroscopy, based on the results obtained, a further treatment regimen and prevention of new calcification formations are developed.
What is calcification in the endometrium?
Often, after undergoing an ultrasound examination, the patient is informed that there are calcifications in her uterus. Any neoplasm is perceived as a dangerous disease, so the logical question arises about what it is, why such formations are dangerous, and how to treat them.
What kind of phenomenon?
This is not a disease, it is a consequence of a pathological process in the main reproductive organ of the uterus. This phenomenon itself represents the localization of calcium salts in a certain uterine area.
Note that calcifications can occur not only in this organ, but also in other organs, for example, in the liver.
Thus, calcification is not only a gynecological disease, it is a pathological process that occurs due to disruption of the normal functioning of a specific organ.
Such formations are clearly visible during ultrasound and MRI. But during an ultrasound, the tissues that make up the formation are not visible, so the presence of calcification can only be assumed. This situation requires additional examination of the woman in order to exclude diseases much more serious than the presence of calcium salt deposits.
Calcification on ultrasound
Reasons for education
Salts of this microelement are found in our body, and this is normal. Calcium participates in the metabolic process inside cells, saturates certain tissues, and so on.
If there is not enough of it in the female body, phenomena such as hair loss, brittle bones, tooth decay, and impaired functioning of the body occur.
The presence of an excessive amount of this microelement in the body also leads to pathologies, for example, urinary retention, deposition in various organs.
What are calcifications in the uterus, and what is their cause? The answer is simple: calcium deposits in the uterus occur due to an inflammatory disease of this organ. Thus, the body protects itself by degenerating chronically affected tissues into calcium deposits, preventing the pathological process from spreading further.
The cause of calcification is often inflammation in the uterus.
Diagnostics
A common diagnostic method is ultrasound examination of the reproductive organ. Gynecologists offer transabdominal ultrasound, which allows you to examine organ pathologies using sensors that the doctor moves across the patient’s abdomen.
The specialist can also offer additional diagnostic methods, if necessary:
- transvaginal ultrasound, which allows you to examine the organ closer, especially during pregnancy;
- hysterography - examination of the pelvic organs using the introduction of a contrast agent, sometimes x-ray and ultrasound;
- Dopplerography;
- three-dimensional ultrasound is a modern method for diagnosing uterine pathologies, which allows you to see calcifications in three dimensions;
- blood test to determine the total amount of calcium.
Three-dimensional ultrasound is by far the most reliable way to diagnose uterine diseases, but its price is significantly higher than other methods.
Danger
Is calcium deposits dangerous? - a question of interest to all women in whom they are detected. It is especially concerning for women who want to get pregnant soon.
We have already understood that the occurrence of such deposits is not an independent disease, but indicates the presence or result of an inflammatory process in the uterus. To determine the condition of the female body as a result of the occurrence of calcifications, additional examination is necessary. It is necessary to determine the root cause of the occurrence of such formations.
After additional diagnostics, it will become clear whether this is a threat to a woman’s reproductive health. Often, on a regular ultrasound, calcifications in the reproductive organ are confused with polyps. Polyps threaten a woman with constant bleeding and pregnancy pathologies.
The expectant mother's uterus should naturally stretch. But with calcium formations it is deprived of this opportunity; changes in the size of this organ will be accompanied by pain. But there is also evidence of the normal course of pregnancy with the presence of such formations. Each case is individual and should be under the supervision of a doctor.
Treatment
To treat the pathology, all necessary diagnostic methods are used, since calcium neoplasms are not a cause, but a consequence. After determining the cause, gynecologists treat the underlying disease or its consequences.
What measures are used in the treatment of this pathology?
- Surgical intervention. It is carried out extremely rarely, since these deposits are not worth the surgical damage to the tissues of the reproductive organ. The risk of bleeding after uterine surgery must also be taken into account. There must be clear indications for surgery when no other method is effective.
- Scraping. With this pathology, this manipulation is effective, but after it calcifications can reoccur.
- A balanced diet and timely treatment of inflammatory processes in the reproductive organ are rather preventive methods, since they are aimed at preventing calcium deposits, and not at removing them.
- Preparations for resorption of such formations are not used. The doctor may prescribe water pepper and several injections of oxytocin so that the calcification is detached from the wall of the uterus, and she pushes it out with her contractions. But any treatment must be carried out under the supervision of a doctor.
Conclusion
Calcium formations in the uterus confuse women, causing certain difficulties in the functioning of the organ. Any measures to diagnose formations and their removal or treatment are agreed with the doctor. You should not self-medicate, since calcifications on a regular ultrasound can be confused with polyps.
Source: https://feedjc.org/kalcinaty-v-jendometrii-chto-jeto/
Pathological changes in the uterine organ
During hormonal changes in the body, especially in premenopause, exacerbation of existing chronic gynecological pathologies may occur, as well as the formation of new ailments that can cause painful symptoms and uterine hemorrhages.
Let's consider the most dangerous pathological changes in the uterus during menopause.
Development of fibroids
This neoplasm itself has a benign course. Typically, fibroids appear during the fertile period, and with the onset of menopause it becomes more acute and begins to increase in size.
Fibroids can form in the form of one or several nodes localized in any part of the uterine cavity. Growing fibroids increase the standard size of the uterus several times, which leads to compression of nearby organs and the appearance of pain symptoms. Enormous growth of this neoplasm can lead to an enlarged abdomen. Moreover, fibroids also cause the following symptoms:
- Uterine bleeding.
- Pain in the lower abdomen.
- Frequent urge to urinate.
- If fibroids grow towards the rectum, stool disturbances and constipation are observed.
Painful sensations may appear during intimacy with a partner.
Treatment for this pathology is prescribed after a full examination, taking into account the individual characteristics of each woman.
Endometriosis
This pathological change in the uterus during the menopausal period is characterized by the growth of the endometrial layer with pathological penetration into the muscular layers of the uterus. Most often it occurs in premenopause, when the menstrual cycle has not yet completely subsided.
Causes symptoms such as:
- painful sensations in the lower abdomen of an aching nature, as well as pain during sexual intercourse;
- prolonged menstruation, when the uterus does not contract for 10-14 days, which is the reason for diagnostic curettage;
- against the background of prolonged menstruation, a disturbance in the psycho-emotional state occurs;
- Infertility may develop.
If one of the presented symptoms appears, you must immediately contact a medical specialist to prevent complications and the development of a more serious pathology.
Chronic form of salpingitis
Salpingitis is an inflammatory process in the fallopian tubes and appendages, which can occur long before the onset of menopause, and with the onset of hormonal changes it can become an aggravated form of the disease. Typically, salpingitis causes symptoms such as:
- Sharp pain in the lower abdomen.
- Increased body temperature.
- Formation of purulent discharge.
In the absence of timely treatment, it can become complicated and lead to the development of pathology requiring immediate removal of the uterus.
Folk remedies
The healing properties of many plants have long been used to get rid of inflammation of the urinary system. Successful:
- Cranberry – has a pronounced diuretic and anti-inflammatory effect. Daily consumption of juice squeezed from cranberries will have a beneficial effect on the course of the disease.
- You need to brew tea from the leaves and berries of black currant. This will relieve the inflammatory process, and if you add a few linden blossoms, your immune indicators will increase.
- A warm bath of St. John's wort, chamomile, and string can improve a person's condition and relieve discomfort.
Prevention of the disease, timely diagnosis of the cause of inflammation of the ureter, is the main guarantee of recovery.
Physiological norm
Calcium salts are found in the body in dissolved form. This is completely normal, since this micromineral is directly involved in many reactions; it is necessary for the normal metabolic process inside. Scientists even suggest that people used to consume this substance three times more. A sufficient amount of calcium allows you not to suffer from brittle bones, ensures healthy teeth, and has a positive effect on blood composition and general well-being.
However, an excess of calcium salts leads to a disease such as calcinosis.
We are talking about calcification that occurs in the soft tissues of the body. The appearance of corresponding deposits inside the uterus is a particular manifestation of this process. Also, an excess of the substance under discussion can result in problems with joints, the formation of kidney stones, and bladder stones. With calcification, the kidneys are most often affected. Therefore, detection of deposits in the uterus should be the reason for a visit to a nephrologist to check the condition of the genitourinary system.
Diagnostics
Since phleboliths do not have typical clinical signs, methods of instrumental visualization of the venous system play a decisive role in their diagnosis . If intravascular inclusions are suspected, the following are informative:
- Ultrasound ultrasound of veins Allows you to evaluate the anatomical features and hemodynamic profile of the affected segments. Phleboliths are defined as rounded echogenic foci with posterior acoustic shadowing and flickering (colored) artifact.
- X-ray of the pelvis. On survey photographs, radiopaque phleboliths are visible as oval structures with concentric rings (“laminations”). The presence of radiolucent stones is considered to be an important diagnostic sign of pelvic stones.
- CT scan of affected areas. Contrast-enhanced computed tomography clearly visualizes intravascular petrification. The venous malformations containing them are distinguished by multiple voids, feeding and draining branches.
- Magnetic resonance imaging. MRI of soft tissues gives an accurate picture of the condition of the surrounding tissues and the extent of vascular damage. Calcifications appear as small foci of low intensity (the “void flow” phenomenon).
Subscribe to our VIBER channel!
a biopsy with histological analysis of stones can help a phlebologist make a final diagnosis . It is necessary to differentiate phleboliths from ureteral stones, appendicoliths, sialoliths, in which excretory urography and sialography . Calcified atherosclerotic plaques and lymph nodes, miliary cutaneous osteomas should also be excluded.
Conflicting opinions
It should be noted that most scientists cannot develop a common point of view on calcifications in the uterus. Some are convinced that this symptom is quite alarming and can indicate a serious hidden pathology inside the body. Others believe that the danger of such deposits is greatly exaggerated; as confirmation of their opinion, they cite statistics indicating numerous cases of successful births with this deviation.
Therefore, you should not be surprised when faced with completely opposite opinions. One gynecologist may advise doing nothing, while another may recommend medications that will stabilize the amount of calcium in the blood. A separate group of scientists suggests that when calcifications are detected in the soft tissues of the body, a special shortage of the corresponding salts should be achieved. After this, the body can “reach out” for replenishment, due to which the tumors will be reabsorbed independently without additional effort.
However, another group of doctors does not agree with this practice. They indicate poor process control. It is difficult to say whether such a reaction will be caused or in what specific time frame. The lack of one of the most important components of the normal metabolic process can seriously affect overall well-being. As you might guess, this is far from improving. If other health problems are added to the calcifications in the uterus, for example, a decreased immune status, inflammatory processes, then such experiments can only lead to a general deterioration. Therefore they are undesirable.
Complications
Many experts consider phleboliths to be harmless intravascular formations. However, it is common that they are associated with thrombosis, indicating a risk of recurrent occlusion. Varicose veins, aggravated by the presence of stones, only increase the likelihood of recurrent thrombosis. Migrating calcifications that enter the portal vein can become a source of pulmonary embolization with quite serious consequences, including death.
Solution
A solution to the problem seems quite reasonable, in which the woman is asked to undergo a comprehensive examination. If there is some kind of hidden pathology, a chronic gynecological disease that decides to make itself felt in this way, it needs to be identified and worked with the root cause. In any case, the general normalization will definitely not make things worse.
A blood test is also taken to examine the total amount of calcium. The diet is often adjusted to increase sodium (especially if there is a lack of sodium) and reduce the amount of foods containing the first micromineral. By achieving this balance, the appearance of further tumors can be prevented.
Treatment may vary depending on the woman's age, her general condition, and whether she plans to have a child in the future.
The uterus of a pregnant woman undergoes certain transformations. It should stretch due to natural flexibility. However, calcifications deprive soft tissues of such an opportunity; any change in size occurs in a traumatic way, causes severe pain, and sometimes bleeding can occur. For this reason, it is advisable for a woman to first remove calcifications before a planned pregnancy.
Surgical intervention is rarely allowed; if the problem is mild, it can be removed by curettage (cleaning). However, it is worth keeping in mind that the last named procedure can also provoke the further appearance of calcifications. Therefore, you should be careful here.
A question of prevention
Prevention of calcification in relation to the uterus can be expressed in a healthy, nutritious, balanced diet. No one will argue: cottage cheese is a truly nutritious food, like many other foods containing calcium.
However, the abuse of any food can only upset the natural balance and lead to an increase in existing problems. It is also worth treating any diseases in a timely manner and trying to avoid the development of pathologies.
Chronic diseases are dangerous because a woman often gets used to them and begins to perceive them as a natural part of her life. And this is absolutely not true, pathology is a strong deviation, it is necessary to work with it.