Squamous cell carcinoma or carcinoma of the cervix is a tumor that develops from the epithelium lining the cervical canal and the vaginal part of the cervix - the endocervix and ectocervix, respectively. This neoplasm ranks first among all malignant diseases of this organ - up to 80% of all cases. In terms of frequency of occurrence in the general structure of all oncological pathologies, squamous cell carcinoma of the cervix is in fifth position. The peak incidence occurs at the age of 30-34 years.
- Etiopathogenesis
- Precancerous conditions
- Clinical manifestations
- Classification
- Diagnostics
- Treatment
- Medical observation after treatment
- Prevention
What is cervical cancer?
ICD-10 code: C53 C 53.1 Cancer of the external part of the cervix C 53.0 Cancer of the internal part of the cervix
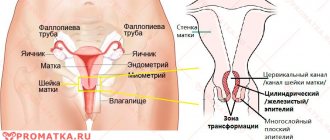
Location of the cervix and cervical canal
Cervical cancer (CC) is an aggressive1 epithelial2 malignant3 tumor that occurs in mature women.
Primary localization of cervical cancer: on the surface of the cervix or in the cervical canal.
1What does “aggressive” mean? This type of tumor is characterized by rapid spread: early metastasis to regional lymph nodes, followed by involvement of various organs and tissues in the pathological process.
2What does “epithelial” mean? Epithelium is tissue that covers all surfaces and cavities of internal organs.
The mucous membrane of the vagina and the outer (vaginal) surface of the cervix is represented by multilayered squamous epithelium. The mucous membrane of the cervical canal is lined with columnar epithelium.
Forms of the cervical epithelium, location of the transition zone
CC develops from altered (atypical) cells of squamous or columnar epithelium. Most often, the pathological process originates at the border between two types of cells - in the transition zone of transformation.
3What does “malignant” mean? Has all the signs of a malignant tumor, namely:
1. Irreversibility of the process The growth and spread of a malignant tumor, including cervical cancer, is irreversible without radical surgical treatment.
Any types of conservative treatment (including radiation and chemotherapy) cannot significantly influence the spread of the malignant process. They only partially suppress it and bring the disease into remission, i.e. to temporary “recovery”.
2. Infiltrative growth A malignant tumor tends to infiltrate: germinate, invade, spread into surrounding organs and tissues. The “tentacles” of cancer damage (“corrode”) the tissue structures involved in the disease, which leads to disruption of the functioning of the affected organs and the entire organism as a whole.
(The growth of a benign tumor is accompanied by an increase in its own volume. At the same time, it seems to “push”, pushes apart neighboring tissues, but does not grow into them.)
3. The ability to metastasize Metastases are secondary foci of a malignant process, distant from the primary tumor.
They are formed by the spread of malignant cells through the lymphatic and blood vessels. Cervical cancer most often metastasizes to regional and distant lymph nodes, lungs, liver, and bones. And extremely rarely - to the brain. At what age do people get cervical cancer?
- Among the cases, women aged 34-65 years predominate.
- The peak incidence is observed in the groups: 45-49 years, 50-54 years and 60-62 years
- Recently, the number of cases of cervical cancer in women under 34 years of age has doubled. Moreover, about 1.7% of cases are women and under 25 years of age
Return to contents
How is cervical cancer treated?
The choice of treatment for cervical cancer in women depends mainly on the prevalence of the disease. Treatment of cervical cancer includes treatment of the primary tumor (surgical, radiation) and areas of regional metastasis.
1. For “cancer in situ” (stage 0), the main method is surgical, the extent of which depends on the age of the patient. Conization and cervical amputation are performed mainly in young women who wish to have children and agree to undergo subsequent examinations. In other cases, a simple hysterectomy is performed.
2. Surgical treatment is possible only for stages 1 and 2a; it is carried out in combination with radiation therapy. The depth of invasion determines the likelihood of metastases to regional lymph nodes and recurrence of cervical cancer, which is taken into account when planning radiation therapy
3. If “cancer in situ” is diagnosed during pregnancy, the woman must be allowed to carry a normal pregnancy to term, and the process must be monitored with a “Pap test”. Treatment for cervical cancer can begin after several months.
4. If invasive cancer is detected during pregnancy before 20 weeks, then it is terminated. After the 2nd trimester, a cesarean section is performed if the fetus is viable and at the same time a hysterectomy is performed as a method of treating cancer. Radiation therapy can be used only after the uterus has been freed from the fetus.
5. Indications for radical surgery are limited by the prevalence of the disease. A typical operation performed for cervical cancer is extended hysterectomy with appendages or Wertheim operation, which includes removal of parametrial tissue. More advanced operations include removing nearby regional nodes. Radical hysterectomy with ovarian transposition is an advantage over radiation therapy in a young patient.
6. In recent years, chemotherapy has also been used. Some groups of drugs are recommended as adjuvant and preventive therapy after surgery and/or radiation treatment. For stage 3 and 4 cancer, gamma methods and chemotherapy are used.
Radiation therapy
Radiation therapy is performed in all stages of invasive cervical cancer. Radiation therapy according to the radical program includes intracavitary introduction of radioactive applicators and external irradiation of the parametrium and lymph nodes of the iliac and para-aortic zones, which may be involved in the process. The cervix is accessible to radiation therapy and is surrounded by tissues that are highly resistant to radiation. The anatomy of the cervix allows the dose of intracavitary irradiation of the cervix to be increased to 100 Gy.
Since the radiation dose decreases inversely to the square of the distance from the radiation source, they are moved to the side to protect the bladder and intestines. Radioactive applicators are inserted into the vagina and into the uterine cavity with a total dose of 60-70 Gy to the paracervical area. The missing dose to the parameters and other areas is compensated by remote gamma therapy up to 30 Gy. The use of radiation therapy in the early stages of the disease allows one to achieve the same level of survival as after surgical treatment.
Prognosis after treatment
The prognosis for cervical cancer is determined by the stage of the disease. Five-year survival rate according to collected data from a number of countries averages:
- At T0-T1 - 100-80%
- At T2 - 60-40%
- At T3 - 30%
- At T4 - less than 10%.
Pregnancy worsens the prognosis of the disease. With successful treatment in the early stages, we can talk about complete recovery, although oncologists always use this word with caution. However, long-term observations have established that in this case the cancer does not recur for decades, and the woman is not bothered by the consequences of treatment.
Prevention
Cervical cancer today remains the leading tumor in the structure of female cancer diseases. But at the same time, this is one of the few malignant tumors, the occurrence of which can be prevented. This is possible due to the fact that it is preceded by a long precancerous process. Among the measures of primary and secondary prevention of cervical cancer, the most applicable are the promotion of a healthy lifestyle and the identification of risk factors.
And timely diagnosis requires new discoveries by doctors, wonderful inventions by pharmacists, and some incredible efforts. In most cases, it is enough to reconsider your life priorities, take the problem of contraception seriously, give up bad habits, get vaccinated against HPV and, of course, undergo medical examination on time.
We can offer you to undergo medical examinations according to a standard or expanded program. It is well known that timely diagnosis of various disorders contributes to their faster and more successful elimination. Individual groups and teams are invited (conditions are negotiated separately).
Squamous cell carcinoma
Squamous cell carcinoma of the cervix is the most common form of the disease.
Diagnosed in 70-80% of patients with invasive cervical cancer. The tumor develops mainly from the stratified squamous epithelium of the transition zone.
Where does cervical cancer start?
What are the types of squamous cell carcinoma of the cervix? /histological forms/: - keratinizing - non-keratinizing - basaloid - verrucous - condylomatous - papillary - lymphoepithelial - squamous-transitional cell
Return to contents
Classification
There are several approaches to systematize squamous cell carcinoma of the cervix. The international morphological classification divides carcinoma into several subtypes: basaloid, verrucous, non-keratinizing, flat keratinizing cervical cancer, etc.
Based on the degree of development of tumor cells, poorly differentiated, moderately differentiated and highly differentiated types of squamous cell carcinoma are distinguished.
There is also a classification that is based on the characteristics of the growth and spread of the tumor process:
- The first stage is characterized by squamous cell carcinoma limited to the cervix.
- In the second stage of cancer, the formation extends beyond the organ, but does not reach the walls of the pelvis. Or the tumor grows into the vagina, but does not reach its lower third.
- In the third stage, the pelvic walls or lower part of the vagina are affected. During a rectal digital examination, there is no “free space” between the neoplasm and the inner surface of the pelvis—the entire space is occupied by the tumor process.
- At the fourth stage, squamous cell carcinoma grows into adjacent organs - the rectum or bladder.
This classification also takes into account metastases in the lymph nodes and other organs, such as the uterus, bones, lungs, etc. Their presence always indicates stage 4 of the disease.
Glandular cancer
In approximately 18% of cases, cervical cancer develops from the prismatic (glandular) epithelium of the cervical canal mucosa.
This is adenocarcinoma or glandular cancer of the cervix.
What is glandular cancer? /histological forms of cervical adenocarcinoma/: - mucinous (endocervical, intestinal, signet ring cell, glandular villous) - endometrioid - clear cell - serous - mesonephric
Glandular cancer of the cervix occurs predominantly in older women
Other forms of cervical cancer
There are mixed (glandular-squamous) cervical cancer carcinomas, as well as poorly differentiated tumors, the cells of which are so altered that they cannot be attributed to any type of body tissue.
Cervical sarcomas are very rare (1-2%)
Histological forms of cervical carcinoma: - glandular squamous cell - adenoid cystic - adenoid basal - neuroendocrine: typical carcinoid, atypical carcinoid, small cell carcinoma, large cell neuroendocrine carcinoma - undifferentiated (undifferentiated) carcinoma
Why does cervical cancer develop?
The main (but not the only) reason for the formation of cervical cancer is cell mutation under the influence of oncogenic human papillomaviruses (HPV 16, 18, 31, 33, 45) and herpes virus type 2 (HSV-2)
In the vast majority of cases (mostly, but not exclusively), these viruses enter a woman’s body through sexual contact.
Penetrating into the nuclei of epithelial cells of the vagina and cervix, viral DNA can be stored for years in a suppressed (latent) state without causing harm.
But when immunity is weakened, viral genetic information damages the genome of the infected epithelium, causing atypical oncogenic changes in cells (mutations).
The proliferation of atypical cells causes disruption of the development of the cervical mucosa, leading to the appearance of a precancerous condition - dysplasia (CIN 2-3).
Read everything about CIN 2 in detail here: Cervical dysplasia 2 (second) degree - treatment, is surgery necessary
Over time, under the influence of various factors, mutations in cells worsen and the pathological process acquires malignant properties. This is how dysplasia develops (malignizes) into cancer.
Read in detail about all treatment methods for severe dysplasia here: Treatment of grade 3 cervical dysplasia - prognosis and methods
Can cancer occur without previous dysplasia? In rare cases, yes. Why this happens is not entirely clear, just as the cause of the formation of any tumors is not completely known.
In every 10th woman with cervical cancer, previous dysplasia or precancer (non-invasive carcinoma “Ca in situ”) cannot be identified.
What increases the risk of developing CC?
- Early (before 16 years of age) onset of sexual activity
- Early pregnancy
- Infection with STIs, HIV
- Frequent change of sexual partners
- Cervical injuries
- Smoking
- Taking hormonal contraceptives and, as a consequence, abandoning barrier methods of contraception, leading to repeated infection with a viral infection
- Genetic predisposition
Stages of cervical cancer
There are two classifications that determine the extent (invasion) and severity of the tumor process: FIGO and TNM.
Where does RMS apply first:
- On the vagina
- On the body of the uterus
- On the parametrium
- To the regional pelvic lymph nodes: paracervical, parametrical, hypogastric, common iliac, external iliac, presacral, lateral sacral
Staging of cervical cancer according to the FIGO system
| Stage | Substage | Description |
| Stage 0 | No | There is no invasive tumor. There is a precancerous condition: non-invasive cancer or carcinoma “in a separate cell” (“in situ”, Ca in situ). Diagnosed solely by the results of histological examination. |
| Stage 1 | The tumor does not extend beyond the uterus | |
| Stage 1 | IA | Microscopic cancer, determined only by histological examination of tissues |
| Stage 1 | IА1 | Microinvasive cancer: the tumor penetrates into tissue depth ≤3 mm. Horizontal spread no more than ≤7 mm. |
| Stage 1 | IА2 | Tumor penetration depth: 3–5 mm. Horizontal spread: ≤ 7mm |
| Stage 1 | IB | Penetration of the tumor in depth: more than 5 mm The tumor is determined (visible) during colposcopy. |
| Stage 1 | IV1 | Tumor size: ≤4cm |
| Stage 1 | IV2 | Tumor size: ≥4 cm within the uterus |
| Stage 2 | The tumor has already spread beyond the uterus, but has not yet affected the pelvic wall or the lower third of the vagina | |
| Stage 2 | IIA | Without damage to the parametrium |
| Stage 2 | IIA1 | Clinically detectable tumor size: ≤ 4 cm |
| Stage 2 | IIA2 | Clinically detectable tumor size: more than 4 cm |
| Stage 2 | IIВ | There are lesions of the parametrium |
| Stage 3 | The tumor has spread to the walls of the pelvis and the lower third of the vagina. Also, all cases of cervical cancer with hydronephrosis and/or non-functioning kidney. | |
| Stage 3 | IIIA | Tumor spread to the lower third of the vagina |
| Stage 3 | IIIB | Tumor spread to the pelvic wall/hydronephrosis/non-functioning kidney |
| Stage 4 | The tumor spreads beyond the pelvis, grows into the bladder, rectum, and gives distant metastases | |
| Stage 4 | IVA | The tumor grows into the mucous membrane of the bladder or rectum, beyond the pelvis |
| Stage 4 | IVВ | There are distant metastases |
Cervical cancer assessment using the TNM system
In clinical case histories, tumor staging is often described using TNM nomenclature: T – condition of the primary tumor N – condition of regional lymph nodes M – metastases (present or not)
Explanation of TNM nomenclature for cervical cancer
| Designation | Decoding |
| Tx | Little/no data to evaluate the primary tumor |
| T0 | The primary tumor is not determined (no tumor) |
| Tis | Precancerous condition |
| T1 | Tumor limited to the cervix |
| T1a | Microscopic invasive cancer, determined only by histological examination |
| T1a1 | Tumor ingrowth into tissue: ≤3 mm Horizontal spread: ≤7 mm |
| T1a2 | Tumor ingrowth into tissue: ≤5 mm Horizontal spread: ≤7 mm |
| T1b | Macroscopic invasive cancer (tumor determined clinically) |
| T1b1 | Visible tumor lesion size: ≤4 cm |
| T1b2 | Visible tumor lesion size: ≥4 cm |
| T2 | The tumor has spread to the upper 2/3 of the vagina/body of the uterus/parametrium. But the pelvic walls are not affected. |
| T2a | ...without damage to the parametrium |
| T2a1 | Tumor size: ≤4cm |
| T2a2 | Tumor size: more than 4 cm |
| Т2b | ... parametrium is damaged |
| T3 | Involvement in the tumor process of the lower third of the vagina and/or pelvic walls... |
| T3a | ... with damage to the lower third of the vagina |
| T3b | ...with damage to the pelvic walls/hydronephrosis/non-functioning kidney |
| T4 | Tumor growth into the rectum/bladder or distant metastases |
| Nx | No/little information to assess the condition of regional lymph nodes |
| N0 | No signs of lymph node involvement |
| N1 | There is damage to regional lymph nodes |
| N2 | Damage to the lymph nodes near the pelvic walls is determined |
| Mx | No/little data to assess metastases |
| M0 | No metastases |
| M1 | There are metastases |
Grouping of cervical cancer stages - according to FIGO and TNM
| FIGO | TNM |
| Stage 0 | Tis |
| (I) Stage 1 | Т1N0M0 |
| IA | T1a N0M0 |
| IА1 | Т1а1N0M0 |
| IА2 | Т1а2N0M0 |
| I.B. | Т1bN0M0 |
| IB1 | Т1b1N0M0 |
| IB2 | Т1b2N0M0 |
| (II) stage 2 | Т2N0M0 |
| IIA | Т2аN0M0 |
| IIA1 | Т2а1N0M0 |
| IIB; IIA2 | Т2а2N0M0 |
| IIВ | Т2bN0M0 |
| (III) stage 3 | Т3N0M0 Т1(any)N1M0 Т2(any)N1M0 Т3(any)N1M0 |
| IIIA | Т3аN0M0 |
| IIIB | Т3bN0M0 Т3bN1M0 Т3аN1M0 Т1(any)N1M0 Т2(any)N1M0 |
| (IV) Stage 4 | T4 N(any)M(any) T(any)N(any)M1 |
| IVA | Т4N(any)М0 |
| IVВ | T(any)N(any)M1 |
Example: Diagnosis: cervical cancer T1bN1M1. This means: stage 4 cervical cancer.
Stages of cervical cancer
What does cervical cancer look like?
Colposcopy.
Cervical cancer Signs of cervical cancer on colposcopy (read about what colposcopy is below, in the “Diagnostics” section)
Vascular atypia – blood vessels in the form of “hairpins”, “commas”, twisted spirals. They do not narrow (do not turn pale) when cervical tissue is treated with acetic acid. The vessels are fragile, bleed easily, and small submucosal hemorrhages are visible.
Rough punctuation and mosaic - red dots, a mosaic pattern on the surface of the cervix occurs due to vascular atypia.
The glands are “rough”, with a raised keratinizing ridge.
Colposcopy. Invasive cervical cancer
Acetowhite epithelium (ABE) - when the cervix is treated with acetic acid (3%), pathological areas of the tissue noticeably turn white (positive test).
Iodine-negative areas (Schiller test) - when the cervix is treated with an iodine-containing solution, the pathological areas remain pale, i.e. do not stain brown (positive Schiller test).
Colposcopy. Positive Schiller test
This is what stage 2 cervical cancer looks like (IIA1; T2a1NxMx)
Colposcopy. Cervical cancer IIA1, stage 2 Return to contents
Causes
Cervical cancer begins its development in altered epithelial tissue, the cells of which line the cervix. Based on this, it was concluded that the occurrence of oncology is often facilitated by precancerous pathologies, which in turn affect changes in the epithelium, called dysplasia. In many gynecological patients, cervical cancer is localized in the area of the junction of squamous and glandular epithelium.
In the pathogenesis of cervical cancer and dysplasia, viruses and infections have a major impact. Scientists have found that the human papilloma virus can have a huge impact on cells, resulting in their mutation and subsequent malignant neoplasm. Studies have shown that every 9 out of 10 women with cervical cancer were infected with HPV. This type of virus is not a rare occurrence and can affect more than 60% of all women, especially during periods of active sexual life.
The human papillomavirus has the ability to cause the appearance of precancerous conditions, such as: cervical dysplasia of varying severity; without timely treatment, it very often degenerates into invasive cancer. Because of this feature, it is necessary to carry out high-quality diagnosis and etiotropic treatment, which is entirely aimed at the causative agent of dysplasia, in order to eliminate dysplastic changes in the cervical epithelium. Likewise, excellent prevention of invasive cervical cancer can be achieved.
Risk factors for HPV infection:
- Early onset of sexual activity, while the epithelial cells of the cervix and uterus are not yet fully mature, which makes them more sensitive to invasive viruses and infections;
- A large number of different sexual partners;
- Unprotected sexual intercourse, that is, without the use of barrier contraceptives (condom) - if a condom is used during sex, both partners significantly reduce the risk of infection with many viruses and infections, the effectiveness of protection against HPV is about 70%.
Risk factors for cervical cancer :
- Smoking – Smoking is known to have a great negative impact on the human body, especially on the chances of developing cancer. Carcinogens contained in tobacco smoke can affect not only the respiratory system. A woman who smokes exposes herself to several times greater risk of being affected by a cervical tumor than a non-smoker. The products of tobacco combustion are often found in the mucous membrane of the cervix. They have the properties of causing changes in the DNA of cells, thereby provoking their mutation.
- HIV – as you know, the HIV virus affects the state of a person’s immunity, gradually destroying white blood cells, thereby reducing resistance. Reduced immunity makes the female body susceptible to many viruses and infections, in particular HPV, which, as described above, in most cases of infection becomes one of the main causes of cervical cancer. In addition, the ability of the immune system to resist malignant cells and suppress their growth decreases, which affects the rate of development of pathology. When AIDS develops from HIV, precancerous cervical pathologies progress to invasive cancer much earlier than in other women.
- Chlamydia infection – chlamydia often affects a woman’s genitals. The only route of transmission is through sexual contact. Most of those affected do not even realize that they are infected until they determine the presence of the pathogen in the results of cervical smears. If a woman has a chlamydial infection, her chance of developing cervical cancer increases several times.
- Diet – if the diet does not contain enough plant foods and vitamins, or a woman has problems with excess weight, her risk of cancer increases.
- Oral contraceptives - if you take oral contraception for a very long time (5 or more years), the risk of developing cervical cancer increases several times.
- Repeated pregnancies – women who have given birth more than 3-4 times are also at increased risk.
- Heredity - if there is or has been a woman in the family diagnosed with cervical cancer, the risk of developing it in relatives increases several times. If you watch out for such factors, you will be able to significantly reduce your chances of being affected by cervical cancer.
The first signs of cervical cancer
A dangerous feature of cervical cancer is that in the early stages of its development the disease does not manifest itself in any way.
Signs of early stage cervical cancer
Precancer (cancer in situ) and stage 1 cervical cancer in the vast majority of cases does not have any symptoms.
Only a very small number of women in the early stages of the disease may experience:
- Lymphorrhea - liquid, watery-transparent, colorless and odorless vaginal discharge of slight or moderate intensity
- Mixed watery-bloody vaginal discharge that looks like “meat slop”
- Contact bleeding from the genitals: after sexual intercourse, gynecological examination, physical stress not associated with the menstrual cycle (both during the reproductive period and postmenopause)
- Menstrual irregularities, changes in the duration and abundance of menstruation
In the case of cervical cancer, even minor contact bleeding may indicate an advanced malignant process that is difficult to treat
Return to contents
Lymph nodes: N = Nodes, regional lymph nodes
Lymph nodes (lymph nodes) act as filters, helping to fight infection and remove harmful substances from the body. There are hundreds of them in the human body.
Regional lymph nodes are the lymph nodes of a certain area of the body; for cervical cancer these are parametric, obturator, sacral and iliac lymph nodes - external, internal and general.
The treatment regimen and tactics depend, among other things, on whether the cancer has affected the lymph nodes.
To describe the number and type of affected lymph nodes, doctors use the letter “N” in combination with numbers:
NX
means that there is not enough data to assess the condition of the lymph nodes.
N0
- no metastases in regional lymph nodes.
N1
- one or more regional lymph nodes are affected by cancer.
The letter “N” is indicated in documents only together with numbers or the letter X - without digital designations it does not contain information about damage to the lymph nodes.
Symptoms of cervical cancer at different stages
| Stage of cervical cancer | Symptoms |
| Stage 0 (precancer) | Asymptomatic or without specific symptoms |
| Stage 1 | Asymptomatic Rare: watery discharge, contact bleeding |
| Stage 2 | In reproductive age: spotting of varying intensity, not associated with menstruation (against the background of normal menstruation). In postmenopause: bleeding of various types. Pain during gynecological examination. |
| Stage 3-4 | Acyclic bleeding, uterine bleeding. Pain in the sacrum, lower back, rectum, kidneys. Dysfunction of the bladder (impaired urination) of the rectum (impaired defecation) |
The appearance of obvious symptoms in cervical cancer is a poor prognostic sign
Is it possible to determine it yourself?
No matter how cervical cancer manifests itself, it is impossible to recognize it by signs and symptoms at home.
After all, many gynecological diseases, including cervical erosion, uterine cancer, adenomyosis, endometrial hyperplasia, uterine polyp, adnexitis, and other background and inflammatory processes of the female genital area have similar and sometimes identical symptoms. Therefore, only a specialist doctor can give an objective assessment of the patient’s complaints during a face-to-face appointment, after examination and further examination.
Every woman (even one who feels completely healthy!) is required to undergo a regular medical examination by a gynecologist once a year, regardless of whether she has any negative symptoms (suspicious of cancer of the uterus, cervix, etc. ) or not.
How quickly does a tumor develop?
The formation of precancerous conditions followed by malignancy can take decades.
Time stages in the development of cervical cancer
| Stage of pathology development | Progression time |
| From primary infection with an oncogenic type of HPV ... to the development of precancerous dysplasia (CIN 2-3) | Average 20 years |
| From dysplasia CIN 2-3... ...to precancer (non-invasive cancer Ca in situ) | 3-8 years |
| From precancer Ca in situ... ...to microinvasive cancer (stage 1 IA) | up to 10 years |
| From stage 1 IA...to macroinvasive advanced cancer | Individually |
Return to contents
Metastasis: M = Metastasis
Each healthy cell in the body has its own specific place in a tissue or organ. Cancer cells can travel throughout the body, creating tumors in different parts of the body.
The tumor created by the division of these cells is called a metastasis.
To describe the presence or absence of metastases, the designation “M” is used in combination with numbers or letters:
M0 —
there are no metastases in organs located far from the uterus.
M1—
Cancer cells have spread to other parts of the body and created metastases—additional tumors.
Next to the letter “M”, 0 or 1 must be indicated. “M1” means that you have stage 4b of cervical cancer; in all other stages, “M0” is written.
Diagnosis of cervical cancer
RMS refers to tumors that remain asymptomatic for a long time. That is why, for early diagnosis and prevention of the development of this deadly disease, every woman aged 18-21 to 65 years should undergo a special screening test: Pap test (see below)
Cervical cancer is a well-controlled disease. Its development can be completely prevented if detected at the precancer stage.
Types of diagnostics
Gynecological examination
In the case of macroinvasive and infiltrative forms of cancer, examination of the cervix on a gynecological chair using vaginal “mirrors” and a recto-vaginal examination can suggest a diagnosis and detect tumor germination in the parametrial tissue, near the pelvic walls.
Cervical cancer is one of the tumors that can be visualized
PAP test
A Pap test or smear for oncocytology is a cytological examination (examination under a microscope) of tissue samples taken from the surfaces of the cervix and cervical canal.
A smear for oncocytology is carried out regularly throughout the life of all women who contact a gynecologist during clinical examinations with an interval of 3-5 years.
According to statistics, the Pap test gives a false negative result in 10-30% of cases.
HPV testing
Cervical cancer is associated with a viral infection in almost 100% of cases. To identify women infected with oncogenic types of human papillomavirus (HPV or HPV), a Digene test, Cobas HPV Test, is performed.
A real-time HPV PCR test is performed to determine the viral load, isolate HPV DNA, and type the virus.
Extended colposcopy
Colposcopy is the study of the vagina and vaginal part of the cervix using an optical colposcope equipped with a binocular and lighting equipment.
Colposcopy
Indications for mandatory testing: positive PAP test (atypical cells detected), positive HPV test, suspicion of cervical cancer.
The method is most valuable for identifying early forms of the disease: precancer, microinvasive cancer.
The sensitivity of colposcopy for diagnosing asymptomatic HPV infection, precancer and cervical cancer is 80-90%
As part of an extended colposcopy, the following is carried out:
- Test with 3% acetic acid: - under the influence of vinegar, healthy vessels narrow and become invisible within 60 seconds, tumor (atypical) ones do not disappear; - if, when treated with vinegar, limited areas of the vagina, transition zone, outer surface of the cervix (stratified squamous epithelium) noticeably turn white (ABE) - this is a sign of pathological transformation of the tissue (leukoplakia, dysplasia, non-invasive or microinvasive cancer, etc.).
- Schiller's test - when Lugol's iodine-containing solution is applied to the cervix, healthy tissues turn brown, but pathological areas do not. All clearly defined light (iodine-negative) areas of tissue are suspicious for atypia and require histological examination.
- Colposcopy with color filters is used for a more detailed study of the vascular pattern of the surface of the cervix.
- Colpomicroscopy is the study of the surface of the cervical tissue under high magnification.
For any deviation of the colposcopic picture from the norm, a targeted biopsy of suspicious areas of tissue is performed. If cervical canal cancer is suspected, a biopsy is performed by conization of the cervix.
Methods for early diagnosis of cervical cancer
Many experts believe that colposcopy should become an expert method for the early detection of dysplasia and microinvasive forms of cervical cancer. The study should be carried out for every woman once a year, regardless of the results of cytology (PAP test) and PCR-HPV testing.
Clinical case: Patient A., 27 years old, underwent a dispensary gynecological examination.
According to the cytology results: type 1 cervical smear (NILM), i.e. PAP test is negative.
HPV testing gave a positive result: infection with HPV type 16 was detected.
Colposcopy was performed: an abnormal colposcopic picture of grade 2, dense acetowhite epithelium was revealed. Suspicion of moderate cervical dysplasia (H-SIL).
After antiviral treatment and local sanitizing therapy, a targeted biopsy of a suspicious area of tissue was performed, followed by histological examination of the biopsy sample.
Confirmed histological diagnosis (after expert review of histological material at the oncology clinic): microcarcinoma of the cervix (T1aN0M0).
Conclusion: in this case, the PAP test turned out to be false negative (uninformative). But unsatisfactory results of colposcopy became an indication for a biopsy with histology. As a result, the diagnosis was made in a timely manner and the treatment was successful.
Taking into account the patient's age, a wide excision (conization) of the cervix was performed. The patient was saved not only her life, but also her reproductive function.
The correct interpretation of the results of extended colposcopy largely depends on the professionalism of the doctor. Use the services of competent specialists.
Histological examination of the biopsy specimen
Cervical cancer - histological diagnosis
All samples of suspicious tissue (biopsy) obtained under colposcopy control are subject to special processing, staining and histological examination (examination under a microscope).
Read more about cervical biopsy here: Cervical biopsy - how it is done and what it shows, preparation and progress of the operation
Sometimes, if a tumor process is suspected in the cervical canal, as well as if there is doubt about the original location of the tumor (where the tumor began to grow from: from the cervix or from the body of the uterus), material for histological examination is obtained by separate diagnostic curettage of the mucous membrane of the cervical canal and endometrium.
Only histology can confirm or refute suspicion of cervical cancer
If the histological picture is controversial, an immunohistochemical study is performed to determine proliferation markers (p16; Ki67) and clarify the degree of tumor differentiation G.
The prognosis for the outcome of cervical cancer largely depends on the “degree of tumor” G:
- G1 is a highly differentiated tumor - its cells are close to normal cells of the body. The most optimistic in terms of cure: it spreads slowly, metastasizes less often.
- G2 - moderately differentiated tumor - not entirely predictable course, uncertain prognosis.
- G3 – poorly differentiated/undifferentiated tumor – the most pessimistic prognosis. It spreads and metastasizes quickly and responds poorly to radiation and chemotherapy.
All types of cervical cancer diagnostics, including cytology, colposcopy and histology, are equally valuable. They do not replace, but complement each other
Ultrasound
An ultrasound examination is performed after histological confirmation of the diagnosis of invasive cervical cancer to determine the extent of the tumor's extent (invasion).
In other words, using ultrasound they try to determine whether cervical cancer has affected neighboring or distant organs and tissues.
To do this, an ultrasound is performed: - pelvic organs, - abdominal cavity, - retroperitoneal space, - lymph nodes, including inguinal and supraclavicular.
X-ray, CT and MRI, PET-CT
The purpose of these procedures is equivalent to ultrasound - to determine the extent of the spread of breast cancer and detect metastases. But the information content of CT, MRI and PET-CT is significantly higher than ultrasound diagnostics.
To exclude or confirm metastatic lesions of the lungs, a chest x-ray must be taken.
Additional Research
If there is a suspicion that the tumor has spread to the bladder, rectum, kidneys, bones, emergency studies are performed according to indications: - cystoscopy, - rectosigmoidoscopy, - kidney scintigraphy, - skeletal bone scintigraphy.
Return to contents
Tumor differentiation: G = Grade, assessment
Before treatment, the doctor will take a piece of tumor tissue and send it to the laboratory for study.
A pathological study establishes the differentiation of tumor cells - how much they differ from healthy ones. This procedure cannot be avoided, since the degree of differentiation affects the prognosis of survival and treatment. The more tumor cells have had time to change, the faster they grow and the less responsive to treatment.
GX
means that doctors were unable to determine the extent to which the cells were different.
This may occur because not enough tumor tissue is provided for testing. G1 -
cancer cells are very similar to healthy ones, which means that most likely they will not grow very quickly and will respond well to treatment.
Such a tumor is called highly differentiated. G2 -
cancer cells differ from healthy ones, this tumor is called moderately differentiated.
G3 -
cancer cells are very different from healthy cells.
This means that the cells are likely to grow quickly and be difficult to treat. Such a tumor is called poorly differentiated. G4 -
cancer cells are not at all similar to healthy ones. This is an undifferentiated tumor that grows quickly and is difficult to treat.
Often, instead of the letter G in combination with a number, doctors simply describe the degree of tumor differentiation with words: for example, “poorly differentiated tumor.”
Cervical cancer: risk factors, dysplasia and symptoms October 6, 2020764 31
Treatment methods for cervical cancer
Treatment tactics for cervical cancer are individual and depend primarily on the stage of the disease, as well as on the age and general condition of the patient.
Main methods of treatment:
- Surgical
- Combined (surgical + radiation)
- Combined radiation therapy (external and intracavitary)
- Chemoradiation therapy
There is no consensus on the tactics of managing cervical cancer - treatment is selected purely individually
Treatment options for cervical cancer by stage
| Stage | Treatment |
| Stage 0 | Conization of the cervix followed by curettage of the remaining part of the cervical canal and uterine cavity. Read more: Conization of the cervix: how the operation is performed, why and when it is done or Hysterectomy with or without appendages |
| Stage 1 (substage IA) | Conization or amputation of the cervix or hysterectomy with or without appendages |
| Stage 1 (substage IB) | Extended hysterectomy during which the following are removed: the cervix and uterus, appendages (tubes and ovaries), pelvic tissue, regional lymph nodes, uterine ligaments, and the upper part of the vagina. Sometimes: postoperative radiation therapy |
| Stage 2 (substage IIA) | Extended hysterectomy or Radiation therapy according to a radical program or Chemoradiation therapy according to a radical program |
| Stage 2 (substage IIB) Stage 3 Stage 4 (substage IVA) | Sometimes it is individually acceptable: surgical treatment + radiation therapy options Standard: chemoradiotherapy according to a radical program (Combined radiation therapy / External beam radiation therapy + Cisplatin weekly during radiation therapy) Possible: maintenance chemotherapy after radical chemoradiotherapy |
| Stage 4 (substage IVB) | Standard: systemic platinum-containing chemotherapy + palliative treatment Occasionally: individual radiotherapy |
Read more about the treatment of stage 1 of the disease: Treatment of stage 1 of cervical cancer. How long do they live after surgery?
Complications of the disease
- Complications of radiation therapy: development of radioresistance of the primary tumor
- Late complications of radiation and chemoradiotherapy
- Tumor recurrence
- Progression of tumor spread, metastasis
Patient survival prognosis
The real possibility of a 100% cure for cancer is absolutely complete, radical surgical removal of the tumor
Radical surgery for cervical cancer is feasible only when the tumor has spread exclusively within the cervix, i.e. in the early stages of the disease: 0 and 1(IA)
In other cases, the effectiveness of treatment depends on the stage and individual characteristics of the tumor process, the qualifications of the attending physician, the technical capabilities of the medical institution, the general condition and fortitude of the patient.
Is it possible to cure stage 4 cervical cancer? read more: Stage 4 cervical cancer - life expectancy prognosis, symptoms
Forecast of 5-year survival for cervical cancer:
- Stage 0 – 100%
- Stage 1 – 85%
- Stage 2 – 65-66%
- Stage 3 – 35-39%
- Stage 4 – about 7-11%
The effectiveness of treatment for cervical cancer Return to contents
Stages
The first signs of cervical cancer depend directly on its type and stage, as mentioned above. Experts have identified at least 4 stages of cancer development in this part of the female body:
- Precancerous. Histological examination will show the presence of cancer cells that have not yet had time to penetrate the epithelium. Timely treatment allows you to get rid of not only the symptoms of the disease, but also its cause. Most specialists guarantee a complete recovery.
- Stage 1 cancer. Malignant cells penetrate the epithelium to a depth of 4-5 centimeters, but the tumor is still small and does not extend beyond the cervix. At this stage, possible signs are bleeding from the uterus and severe pain in the lower abdomen.
- Stage 2. The malignant tumor metastasizes and leaves the cervix. The pain intensifies, my back begins to ache, and anemia occurs. The disease at this stage is considered relatively curable.
- Stage 3. The tumor affects the pelvic walls and the upper part of the vagina. The prognosis is unfavorable, the patient loses strength, heavy bleeding occurs, and anemia develops.
- Stage 4. Metastases affect the pelvic organs and lymph nodes, and their active spread throughout the body is observed. The survival rate of women whose disease has reached this stage is low.
Unfortunately, in a number of cases, patients turn to a doctor precisely at the moment the disease moves to stage 4, which suggests a high degree of danger to life from cervical cancer. The clinical picture at this stage is so unfavorable that nothing can be corrected. The bleeding practically does not stop, anemia begins, the lower extremities swell, the pain is sharp and does not stop even at night.
Methods for effective disease prevention
- High-risk HPV vaccination
- Cervical screening: smear for oncocytology (PAP test at least once every 3-5 years) + PCR testing for HPV and HSV2 DNA + extended colposcopy once a year
- Dispensary examination by a gynecologist at least once a year
Effective treatment of cervical dysplasia prevents the development of cancer in almost 100% of cases
Today, thanks to mandatory cervical screening, the incidence of cervical cancer has begun to decline. However, mortality remains very high - about 190,000 women die from this disease every year in the world.
Return to contents
Doctors' advice on early diagnosis of the disease
Every woman should undergo cervical cancer screening - this is a pre-symptomatic screening method that women should undergo 3 years after the start of sexual activity, but no later than 21 years of age. Screening is carried out every year with a smear examination.
If a woman is over 30 years old and has previously had 3 negative smear results in a row, she is allowed to undergo screening less frequently (every 2-3 years). If a woman has HPV or is immunocompromised, undergoing chemotherapy or steroid hormones, annual screening should be performed.
Contraindications
The vaccine contains a lot of components that can have a negative effect on the body, for example: sodium chloride, polysorbates, sodium tetraborate, aluminum. It is also based on processed transgenic yeast. Girls who are allergic to yeast are not recommended to be vaccinated against cervical cancer due to the risk of complications. Photo 3 shows one of the vaccines (Gardasil), which is used to prevent cervical cancer.
Video on the topic
No similar articles found.
Features of treatment
By contacting me, each patient can count on an individual approach; I select the tactics of examination and treatment, taking into account many nuances: age, the presence of concomitant pathologies, previous surgical interventions, etc.
My experience includes more than 400 successfully performed laparoscopic operations. I perform a low-traumatic intervention on all patients using laparoscopic access - all manipulations are performed through several centimeter punctures on the anterior abdominal wall. Due to the low-traumatic nature, recovery is faster than with open surgery. Using the latest generation equipment, I manage to achieve maximum efficiency, while the intervention itself is safe and short-lasting.
An important step is lymphadenectomy. During surgery, performed by most surgeons, after removal of lymph nodes and vessels, a large amount of lymph flows into the abdominal cavity; To treat this complication, it is necessary to install drainage in the pelvic cavity for a long time. To avoid drainage, I use instruments during lymph node dissection that can be used to reliably seal vessels (blood and lymphatic). Thus, the operation area remains dry, which allows all manipulations to be carried out with high precision. Our clinic has developed and successfully used the Fast Track system - rapid recovery surgery: the body's stress response is reduced, the time of hospital stay is minimal.
Cervical diseases are one of the few that can be detected by visual examination during a screening examination. Therefore, I recommend that all women undergo regular scheduled examinations - once a year. If cervical cancer is suspected, early diagnosis is crucial; with timely treatment, recovery is possible in more than 90-95% of patients.
Treatment
Thanks to the latest developments by foreign specialists in the field of screening, cervical cancer can be detected in the early stages, thanks to which it can be successfully treated. According to statistics, diagnosing cervical cancer at an early stage can guarantee that the patient will be cured in 98% of cases.
The choice of treatment plan depends on the stage of the disease, the age of the patient, the presence of concomitant diseases and many other factors.
As with any other localization of a malignant process, cervical cancer is treated using traditional methods of therapy: surgery, chemotherapy and radiation therapy.
Surgery
The extent of the operation depends on the extent of the lesion and the stage of the disease. The initial stages, which are most often successful in young women, allow for organ-preserving treatment. Many patients manage to maintain menstrual and reproductive function. If the disease has reached a severe form, surgeons perform a radical hystrectomy - removal of the uterus, cervix and appendages. If a woman has reached the age of 40-43 years, this operation is performed with preservation of the ovaries to prevent post-castration syndrome.
Radiation therapy
Refers to effective and alternative methods of treatment for cervical cancer in the first stage. Radiation therapy can be used as an independent and main method of treating more advanced forms of the disease, since during these stages the tissues surrounding the neck are involved in the process. Irradiation is carried out using special radiation devices that direct high doses of radioactive rays to the lesion. The latest technical equipment minimizes the impact on healthy tissue, and therefore reduces the occurrence of complications.
Some patients are prescribed a course of radiation therapy, with the parallel introduction into the body of chemotherapy drugs that complement each other's action.
Also, radiation is used as an additional method after surgery. It can destroy malignant cells missed by the surgeon and minimize the occurrence of relapse.
Chemotherapy
The use of chemotherapy for cervical cancer is very rare. This can be explained by the fact that this location of the cancer is considered insensitive to this treatment. Basically, anticancer drugs are prescribed for palliative treatment, in order to ease the patient’s symptoms and alleviate her general condition. Indeed, in some cases, cancer can no longer be cured, but doctors try to alleviate the suffering of the patient.