A pathological condition such as endometritis can often lead to a diagnosis of infertility. It can have either an acute course or become chronic. This is a process that is characterized by a bacterial infection, which causes the absence of pregnancy, as well as its spontaneous termination, non-developing pregnancy.
Specific endometritis occurs due to penetration of various infections into the inner mucous membrane of the uterus. For example, these could be viruses, bacteria, fungi, parasites. This type of endometritis is the easiest to detect.
Acute endometritis - what is it?
The mucous layer that lines the inside of the uterus is called the endometrium. Its structure is not constant, it changes throughout the menstrual cycle. First, it grows and matures, preparing the uterus for a possible pregnancy. If pregnancy does not occur, then endometrial rejection occurs. In healthy women, there should be no microorganisms in the uterine cavity. If they penetrate there, an inflammatory process develops in the endometrium - acute endometritis.
Acute endometritis is associated with infection of the surface of the uterine cavity when the basal layer of the endometrium is affected. There are complicated cases when pathogens spread through lymphatic vessels into muscle tissue. Then they talk about the development of metroendometritis. These diseases make up just over 2% of all gynecological pathologies. Among acute inflammations of the upper genital tract they account for 9.7%. As for the general statistics on inflammatory diseases of internal organs, endometritis and metroendometritis occur in 0.9% of cases.
Causes of acute endometritis
Inflammation develops under the influence of such factors:
- Complicated childbirth with injuries.
When ruptures of the cervix, perineum and vagina occur, pathogenic microbes enter the uterine cavity.
- Damage to the vagina.
Neglect of personal hygiene, frequent douching, and the use of local contraception disrupt the normal vaginal flora, which reduces the protective properties.
- Bloody discharge (during menstruation, abortion, childbirth).
The release of blood provokes alkalization of the vaginal environment, which creates favorable conditions for the development of pathogenic flora.
— Use of intrauterine contraceptives.
A foreign body (IUD) remaining in the uterus for a long time can contribute to the infectious process.
— Use of tampons for hygienic purposes.
Tampons create a favorable environment for the proliferation of pathogenic microbes.
- State of stress.
In stressful situations, general immunity is suppressed, causing the body to lose protection against infections.
The most common cases are acute endometritis due to the IUD and postpartum endometritis, which develops in 4-20% of women in labor. In the case of cesarean section, the number of cases reaches 40%.
The risk of the disease increases due to hormonal fluctuations in a woman’s body, weakening of the nervous system, and decreased immunity. In such cases, the disease can be severe and with complications, and if left untreated, the disease can become chronic.
Clinical picture
Symptoms, course
Diagnostic criteria for diagnosis:
Complaints and anamnesis:
Complaints [1] : · reproductive dysfunction: infertility, miscarriage.
History: · history of acute or chronic endometritis; · complicated childbirth, abortion; · intrauterine invasive manipulations (curettage of the uterine cavity, insertion or removal of an IUD); · infertility; · habitual miscarriage.
Pathogenesis of acute endometritis
Primary inflammation, limited to the uterine area, is most often a consequence of infection ascending through the cervical canal. In this case, the intact endocervical barrier can be overcome by highly virulent organisms, such as gonococci. But usually microbes penetrate this barrier when it is damaged. The integrity of the cervical barrier may be impaired due to spontaneous termination of pregnancy, abortion, or the use of an IUD. Also dangerous in this regard are diagnostic curettages and some other medical procedures.
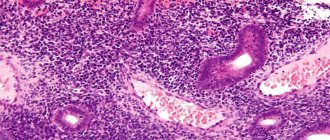
In some patients, inflammation spreads to the muscle tissue of the uterus. At the same time, vasodilation is observed in the affected areas, blood flow slows down, and thrombosis develops. There is severe exudation (purulent or serous purulent exudate). Histological examination reveals neutrophilic infiltration in the myometrium. If anaerobic pathogens join, necrotic changes in the myometrium cannot be ruled out.
Types of adenomyosis
The disease can take several forms and develop to different levels. There are 3 known types of it:
- Diffuse. With it, mucosal cells form foci of varying depths in the thickness of the myometrium;
- Nodal. In this case, endometrial tissue leaks through the protective membrane, forming corridors. Then they begin to rapidly divide, spreading into the myometrium with the formation of nodules, wrapped on the outside with connecting material and filled with brown liquid on the inside;
- Mixed. This type of internal endometriosis is diagnosed more often than others and is a mix of diffuse tissue growths and nodular ones.
Whatever category adenomyosis belongs to in a particular case, the ICD 10 code will be No. 80.0.
Symptoms of acute endometritis
The disease makes itself felt within 3-4 days from the moment of infection. The patient's general health deteriorates significantly, the temperature is usually elevated - from low-grade fever to febrile levels. Possible weakness and chills. Severe pain appears in the lower abdomen, which radiates to the groin or sacrum. Pathological discharge begins (seropurulent). They can be sanguineous for quite a long time, since the regeneration of the mucous membrane slows down. If fragments of the fertilized egg remain in the uterine cavity, severe bleeding begins. Endometritis associated with gonorrheal infection may begin with bleeding only. They pass through the type of prolonged menstruation or occur several days after its end. Purulent mucous discharge may have an unpleasant odor (if E. coli is present). Due to desquamation of the epithelium in some areas of the endometrium, purulent discharge may contain bloody admixture. Disturbances in the processes of endometrial rejection lead to the appearance of a characteristic symptom – hyperpolymenorrhea.
During a gynecological examination, the uterus is pasty, enlarged, and painful on palpation. The pain is most pronounced along the lymphatic vessels and on the sides. If the peritoneum is involved in the process, pain is felt when the cervix is displaced, the leukocyte count is shifted to the left, and the ESR is increased. The acute phase of the disease usually lasts up to 10 days. If the therapy was adequate, the disease is completely cured. If not properly treated, the inflammation can become subacute or chronic and become a serious problem.
Diagnosis of acute endometritis
Endometritis has some symptoms that are also characteristic of other diseases (such as proctitis, paraproctitis, appendicitis). Therefore, diagnosis must be carried out very carefully.
History taking
The examination begins with a conversation. In this case, the doctor asks the patient the following questions:
— Has she suffered from any gynecological diseases in the past?
— What treatment and when did she undergo it?
— Has she had to undergo gynecological surgery in the past?
— Were any diagnostic procedures carried out?
— Did your sexual partner have any sexually transmitted infections?
— Has the woman recently developed thrush or bacterial vaginosis?
The gynecologist also finds out the features of the menstrual cycle - its duration and volume of discharge. After talking with the patient, they proceed to a gynecological examination.
Gynecological examination
With endometritis, palpation of the lower abdomen allows you to determine the soreness of the uterus and its slight enlargement. After performing an examination using mirrors, the doctor notes the presence of purulent discharge, inflammation of the vaginal mucosa and cervix. The cervical canal can be widened.
Laboratory research and analysis
If endometritis is suspected, a woman is prescribed the following tests:
— Blood test (general analysis).
With endometritis, an increase in leukocytes is observed, due to immature forms, the level of neutrophils rises, and the ESR increases.
— Microscopic examination of vaginal discharge.
A smear is taken from the walls of the vagina and cervix. A large number of leukocytes are observed in the biological material under study. A pathogenic microbe is detected.
— Bacteriological smear analysis.
This study not only makes it possible to identify the pathogen, but also to evaluate its sensitivity to certain antibiotics. PCR method. It helps identify specific infections. Effective in diagnosing sexually transmitted diseases.
— Enzyme immunoassay of blood.
It can also help identify sexually transmitted diseases.
To clarify the diagnosis, an ultrasound examination can be performed, and smear tests can be performed over time.
Subacute endometritis
In the subacute form of endometritis, the inflammation is mild. In fact, this disease is a transitional stage between acute and chronic endometritis. Women, whose body's reactivity is reduced, are most prone to this pathology. The development of subacute endometritis begins approximately on the 4th day after infection with pathogenic organisms. In some cases, the inflammatory process may develop much later - after 2 weeks.
As already mentioned, the symptoms of subacute endometritis are mild, and sometimes the infection occurs hidden. Therefore, many women with this disease do not even suspect that they may have such a problem. They do not go to the hospital and do not receive treatment. And this threatens the disease becoming chronic, with periods of exacerbations. Possible symptoms of the subacute form of the disease include: slightly elevated temperature, constant fatigue, weakness. Aching pain may occur in the lower abdomen; as a rule, it radiates to the lower back and groin area. Vaginal discharge may be scanty.
The only characteristic sign that indicates trouble is bleeding. They are associated with disruption of endometrial repair processes and inflammation in the uterus.
Quite often the disease manifests itself as disruptions in the menstrual cycle. Brown discharge may occur in women between cycles, and much less blood may be released during menstruation. If the form is advanced, menstruation may stop altogether. This is due to the fact that the main layer of the endometrium is destroyed, and the layer that should be shed during menstruation ceases to be restored.
Differential diagnosis
Table – 1. Differential diagnosis of chronic inflammatory disease of the uterus
Chronic endometritis is a chronic inflammatory process that occurs with damage to the functional and basal (cambial) layers of the endometrium. In severe cases, the myometrium is involved in the pathological process.
N71.1 Chronic inflammatory diseases of the uterus.
EPIDEMIOLOGY OF CHRONIC ENDOMETRITIS
The incidence of chronic endometritis varies widely from 0.2 to 66.3%, but averages 14%.
Treatment of acute endometritis: basic methods and drugs
Therapy for acute endometritis must be started on time, it must be comprehensive and adequate. Since endometritis is an infectious process, antibiotics play a leading role in treatment. Before drug therapy, a bacteriological analysis of smears is performed, which makes it possible to determine which antibiotics the pathogen is sensitive to. It takes a whole week to obtain the results of a bacteriological study. It is impossible to leave the patient without treatment for such a period, otherwise the disease may worsen. Therefore, a course of broad-spectrum antibiotics that act on different groups of bacteria is immediately prescribed. In the acute form of the disease, hospital treatment is recommended.
Goal of therapy for acute endometritis
Treatment of patients with endometritis is aimed at:
— Destruction of the pathogen.
— Prevention of the disease becoming chronic.
— Restoration of the normal menstrual cycle.
— Preservation of a woman’s reproductive function.
Non-drug treatment of acute endometritis
During periods of elevated temperature, bed rest and adequate nutrition with easily digestible food containing vitamins are indicated. It is recommended to periodically apply cold to the lower abdomen.
Treatment of acute endometritis with antibiotics
In acute forms of endometritis, systemic antibiotics are indicated. The treatment regimen depends on the spectrum of suspected pathogens, taking into account their sensitivity to a particular type of antibiotic. It is necessary to take into account the fact that acute endometritis often has a polymicrobial etiology. Therefore, patients need combination therapy, for example, a combination of cephalosporins and metronidazole, lincosamides and aminoglycosides of the 2nd–3rd generation. During a course of monotherapy, inhibitor-protected aminopenicillins and carbapenems can be prescribed. If the presence of chlamydia is suspected, an additional course of doxycycline or macrolides is necessary. Dosages of drugs and duration of courses depend on the degree of the infectious process. If necessary, desensitizing and restorative measures are carried out, and infusion therapy is carried out. To improve the outflow of lochia, drugs that contract the uterus are prescribed together with antispasmodics. If the development of endometritis was provoked by a late abortion, the course of therapy should include intrauterine lavage using an antiseptic solution (dioxidine, nitrofural).
Treatment regimen for acute endometritis
Combination of penecillins with beta-lactam antibiotics: 1.2 g of Augmentin (intravenously, 4 injections per day) and 1.5 g of unasin (intramuscular injection, 4 times per day).
Combination of 2nd generation cephalosporins with nitroimidazoles and aminoglycosides: 1 g of cefazolin (intramuscular) three times a day plus 0.5 g of netrogil (intravenously) three times a day plus 0.08 g of gentomycin (intramuscular) three times a day.
The dosages of all medications should be determined only by a doctor on an individual basis for each patient. When selecting drug therapy, the type of infection, the state of the immune system, the stage of the inflammatory process and the nature of its development are taken into account.
Ways to combat body intoxication
Bacteria produce a lot of toxic substances that affect a large volume of uterine tissue. In addition, toxins penetrate the bloodstream and negatively affect the entire body. This means that it is necessary to carry out procedures that help cleanse the patient’s blood of toxic substances. First of all, droppers with saline solution, albumin, refortan, and rheopolyglucin are needed. Antioxidants such as vitamin C will also be of great help.
Immune system stimulation
A course of antibiotics and detoxification treatment can only rid the body of harmful bacteria and their toxins. The main role in the fight against endometritis is given to the immune system, so it needs to be supported. The patient is sent to a gynecological hospital, where she must remain in bed and eat a healthy, balanced diet.
To strengthen the immune system, vitamin preparations (B and C) and drugs that increase nonspecific immunity are prescribed:
— Timalin (or T-activin) every day, 10 mcg for a ten-day course.
— Rectal suppositories Viferon 500 thousand units twice a day for a five-day course.
Surgical treatment of acute endometritis
Major surgical procedures include:
— Removal of the intrauterine device.
— Removal of fragments of the fertilized egg from the uterine cavity.
In acute form, endometritis lasts from 8 to 10 days. If the treatment was adequate, the disease is cured. In the absence of timely treatment, the disease takes a subacute or chronic course.
If therapy is prescribed, but after 3 days there is no improvement, additional diagnostics are prescribed and, in some cases, surgery is resorted to.
Patients must remain in bed, apply cold to the lower abdomen, and take antibacterial drugs (the antibiotic regimen is determined depending on the nature of the inflammatory process, the type of pathogen, and the duration of the infection). Since the aerobic flora is often joined by anaerobic flora, tinidazole, ornidazole, and metronidazole are indicated. Non-steroidal anti-inflammatory drugs, desensitizing and sedatives are also indicated. If significant blood loss is observed, medications are recommended that enhance the ability of the uterus to contract. Hemostatic medications are prescribed. A course of immunomodulatory therapy is often recommended.
Another effective method is flow-through drainage of the uterus using a cooled antiseptic solution. If necessary, substrates that contribute to the inflammatory process (decidual tissue, fragments of the fertilized egg) are removed from the uterine cavity. This intervention is carried out after 2 or 3 days of active treatment, when the patient’s temperature returns to normal.
How to treat uterine endometriosis
Treatment of adenomyosis remains a complex, ambiguous problem, purely individual for each patient, for each specific case of the disease.
Treatment of internal endometriosis
Hormonal treatment of uterine endometriosis
Speaking about the effectiveness of hormonal treatment, you need to know that none of the drug therapy regimens leads to a complete cure or eliminates the possibility of relapse of endometriosis.
The effect of hormonal treatment is temporary - after stopping the drugs, the disease may gradually return.
In cases of asymptomatic uterine endometriosis, ultrasound signs of the disease are not an indication for hormonal therapy.
For asymptomatic adenomyosis of 1-2 degrees, a “wait-and-see tactic” is advisable, i.e. the patient does not receive hormonal treatment, but is under close dynamic monitoring. According to indications, restorative and physical therapy, immunocorrection, antioxidant and anti-inflammatory therapy may be prescribed (see below).
Objectives of hormonal therapy:
Drug therapy for uterine endometriosis is primarily aimed at patients interested in future pregnancy.
Hormonal therapy is based on the significant role of endocrine factors in the development of endometrioid disease. It is carried out in the absence of contraindications and side effects. Initially, treatment is prescribed for 3 months. Then its effectiveness is assessed and, if successful, extended for 6-9 months. In case of unsatisfactory results, drug replacement or surgical treatment is indicated.
First-stage hormonal drugs for uterine endometriosis
1.Oral progestogens. Monotherapy with drugs like progesterone is considered quite effective for adenomyosis. Progestogens are prescribed continuously, in fairly high doses, for 3-6 or more months. Their incidence of side effects is significantly lower than that of GnRH A (see below).