Uterus: structure and functions.
The uterus consists of the fundus of the uterine body and the cervix. The isthmus of the uterus is separated between the cervix and the body of the uterus. In turn, the uterus consists of three layers. The first layer is the inner layer, the mucous membrane - the endometrium. The middle layer consists of smooth muscle tissue - the myometrium. The outer layer is the serosa of the uterus, which covers most of the organ and is called the perimeter.
As already mentioned, the uterus performs a generative function. During the period of performing this function, the uterus undergoes some changes. With the onset of pregnancy, its shape changes: round is replaced by oval. Depending on the timing of pregnancy, the thickness of the walls changes. In addition, the weight of the uterus almost triples during this period.
Changes also occur in the cervix, but only towards the end of pregnancy. In the last weeks of pregnancy, it becomes soft and shortened. This will indicate the body’s readiness for childbirth.
An important function of the uterus in the female body is the menstrual function.
This function of the uterus is characteristic of those females who have reached puberty. This function is a cyclical process that normally occurs monthly in the absence of pregnancy. During the menstrual cycle, the inner layer of the uterus undergoes changes. It thickens and is rejected under the influence of progesterone. As a result, menstruation occurs.
You can also highlight several additional functions of the uterus in a woman’s body:
- protective. The uterus is a kind of barrier to infection that enters through the vagina;
- The uterus, together with its ligamentous apparatus, strengthens the pelvic floor.
Regular preventive examination by a gynecologist makes it possible to prevent possible pathologies in time, which will allow the important organ to function normally.
Ligamentous apparatus of the uterus and uterine appendages
The ligamentous apparatus of the uterus is represented by a number of ligaments. It should be emphasized that the muscular-fascial pelvic floor is of greater importance in strengthening the uterus and the ligaments are of lesser importance. Therefore, the apparatus that fixes the uterus must include, first of all, the pelvic diaphragm
, and then a system of strengthening ligaments.
At the same time, the pelvic diaphragm
refers
to the “supporting”
apparatus,
ligaments - to the “suspensory” apparatus.
According to modern views, thus, the supporting apparatus, consisting of strong muscular-fascial tissue, is a truly strengthening apparatus of the uterus; the ligamentous apparatus, on the contrary, has only an auxiliary value: the ligaments only limit the mobility of the uterus in one direction or another.
1 - Hg. pubovesicale; 2 - lig. vesicouterinum; 3 - lig. cardinal; 4 - lig. sacrouterinum; 5 - lig. ovarii proprium; 6 - lig. latum uteri; 7 - lig. suspensorium ovarii; 8 - lig. teres uteri
The ligaments of the uterus include:
I. big. latumuteri(dextrumetsinistrum)
—
the broad uterine ligament (right and left)
is a paired duplication in the frontal plane in the small pelvis.
In the process of development, the uterus, gradually enlarging, lifts the peritoneum upward, as if “dressed” with it and sends its double leaves to the sides, which are called the wide uterine ligaments. Approaching the lateral walls of the pelvis, the broad ligament of the uterus directly passes into the parietal peritoneum.
Stretched broad ligament
has a quadrangular shape.
Its medial edge is fixed to margo lateralis
uteri with the formation of a narrow interperitoneal track.
The lateral edge is fixed to the lateral wall of the pelvis minor
in the area of
the articulatio sacroiliaca
.
The top edge is free; the uterine tube passes through its thickness. The lower edge is located at the bottom of the pelvis. Both leaves here diverge anteriorly and posteriorly and turn into parietal peritoneum.
Along the lower edges of the wide uterine ligaments, compacted connective tissue cords diverge away from the uterus - the so-called cardinal ligaments.
The broad uterine ligaments are not smooth throughout their entire length.
In their thickness are the fallopian tubes, ovaries, own ovarian ligaments and round uterine ligaments. All these formations protrude the peritoneum of the broad uterine ligament with the development of a mesentery for each of them.
In the broad uterine ligament there are:
1.
Mesometrium
- own mesentery of the uterus, occupying most of the broad uterine ligament (approximately its lower 2/3).
Its duplication contains a significant amount of fatty tissue, gradually increasing downwards. Inflammation of this tissue is called lateral parametritis, parametritis lateralis
.
2.
Mesosalpinx
- mesentery of the fallopian tube, occupies the upper ⅓ of the broad uterine ligament. This is a transparent duplication of the peritoneum that does not contain fatty tissue between the sheets.
3.
Mcsovarium
- the mesentery of the ovary and its own ligament of the ovary is formed by extending the posterior sheet of the broad ligament posteriorly.
It is the boundary between the overlying leaves of the mesosalpinx and the underlying duplication of the mesometrium. It is also a transparent duplicator that does not contain fatty tissue.
4.
Mesodesma
- braid - peritoneal strip, under which is located the round uterine ligament, slightly elevating the peritoneum.
Unlike the mesentery of the small intestine, the broad uterine ligament is a paired mesentery; its duplication is located to the right and left of the uterus.
II.
The cardinal ligaments of the uterus, ligamentacardljiallauteri, are essentially the base of the broad uterine ligaments.
The lower edge of the wide uterine ligaments, thickening due to the development of fibrous elements and smooth muscle fibers, forms dense cords diverging away from the cervix of the uterus, round in shape, called the cardinal ligaments of the uterus.
These ligaments prevent lateral displacement of the uterus and act as an axis around which physiological movements of the body and fundus of the uterus anteriorly and posteriorly occur.
These ligaments arise at the level of the oriflclum uteri internum
and fix the uterus on both sides.
It can be concluded, therefore, that these ligaments prevent the emergence of lateropositlo (dextra or sinistra).
III. Round uterine ligament, llg.
rotundumuteri, is an analogue, as is llg.
ovarii proprium, Gunter's cord of men, gubernaculum hunteri. It departs from the lateral surface of the body, more precisely, from the angle of the uterus anterior to the beginning of the tuba uterina
, heading forward and outward and enters
the anulus ingulnalis internus
.
On the way the bundle crosses n
.
and vasa obturatorla
,
llg
.
umbil i cale laterale
,
vena iliaca externa
and
vasa eplgastrlca inferlora
.
In the inguinal canal lig
.
teres uteri
enters together with
a.
spermatica externa and
n
.
spermaticus externus
.
The basis of the round uterine ligament is fibrous tissue. From the uterus to the anulus ingulnalis internus
, the ligament has a significant admixture of smooth muscle fibers; in the inguinal canal it consists of fibrous tissue, smooth muscles derived from the muscular elements of the uterus itself, and striated fibers due to the attachment of muscle bundles from the internal oblique and transverse muscles, and at the exit from the inguinal canal - within
the labia majora
from only one fibrous tissue, the bundles of which fan out in the upper 2/3 of the labia majora.
Upon exiting the external inguinal ring, the round uterine ligament is surrounded by branched fatty lobules, forming a cluster of Imlach.
In some cases, the round uterine ligament carries with it a section of the peritoneum into the inguinal canal, similar to the processus vaginalis peritonaei of men.
This area of the peritoneum is called the nuccova.
diverticulum,
diverticulum Nuckii
, which often serves as the site of development of Nuck cysts filled with serous fluid.
In cases where a large amount of such fluid accumulates, real dropsy of these diverticula develops, called hydrocele femlnlnum
.
Functionally, the round ligaments have some significance, preventing the uterus from tilting backwards.
IV.
Sacro-label ligaments, lig.
sacrouterine, are muscular-fibrous bundles that somewhat stretch the peritoneum on both sides in the form of a fold. The muscular elements of this ligament are called m.
rectouterinus s. secrouterinus . This paired muscle in the form of a rounded stem on each side stretches from the posterior surface of the cervix, starting approximately in the middle of its length, goes back and is woven into the muscular elements of the rectum; some of the fibers go further and are fixed to the sacral bone at the level of the II-III sacral vertebra.
Hence the name m. rectouterinus s. sacrouterinus.
Female body
Representatives of the fair sex differ in many ways from men. In addition to external signs, there are also internal structural features of the body. Thus, representatives of the weak half of humanity are able to reproduce their own kind and feed them. A woman’s uterus, ovaries, pituitary gland and other organs play a major role in this process. Men are structured more primitively and simply.
Anomalies
All the characteristics of an organ listed above are characteristic of the normal structure and development of the organ, with its proper functioning and normal hormonal balance in the body. However, there are many types of pathologies of this organ. Of course, most of them are acquired and can (or cannot) be treated, but there are also many congenital anomalies that may or may not bother a woman, and may or may not require treatment.
Saddle
In this case, the fundus of the uterus is changed, and the organ itself has the shape, rather, not of a ball, but of a cone, directed with its apex downward (towards the cervix). This condition often leads to infertility, as it makes it difficult to bear a child.
Two-horned
This is a modified structure of a woman’s uterus, when the organ has two protruding angles located symmetrically. They are located in the upper part of the organ, that is, directed towards the chest.
Partition
Another congenital pathological condition that, without treatment, interferes with pregnancy and/or normal pregnancy. In this condition, there is a septum, the isthmus of the uterus in its cavity.
Doubling
As the name implies, this is a condition when there are two uteruses or some of its parts (three or four - if we are talking about paired organs). They may have different or the same (very rarely) degree of development. If pregnancy is planned, then first, usually, an operation is performed to remove the “extra” set of organs.
Hypoplasia
This is a congenital underdevelopment of organ tissues, in particular, thinning of the endometrium associated with hormonal disorders or structural features of the tissues. This condition usually makes it difficult to get pregnant and therefore requires treatment if the patient wants children.
Agenesis
Another name for this congenital condition is aplasia. With this congenital condition, the uterus is completely absent in women (at the same time, ovaries are present, and the hormonal balance may be more or less normal, although more often this phenomenon is combined with signs of intersexuality).
Location violations
There are such congenital anomalies when the position of the uterus in the body is changed (in this case, the uterine appendages can be located normally or changed). It can be bent forward or backward, to a greater or lesser extent, but if this condition is congenital, then it does not require treatment and can even be corrected during pregnancy.
A woman's uterus: what is it?
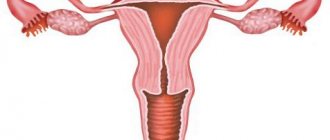
This organ is located in the small pelvis of every woman even before birth. Thus, the reproductive region is formed approximately at the 10th week of intrauterine life. Externally, the uterus resembles a small inverted pear or cone.
On the sides of a woman’s uterus there are two so-called processes. Doctors are more familiar with them under the name fallopian (uterine) tubes. Also under each of these processes there is a small oval-shaped organ. These structures are called ovaries.
In addition to the internal structural features of the uterus in women, it has a cervix and a cervical canal, which opens into the vagina. The internal cavity of the reproductive organ has three layers. The main one is the endometrium - the inner lining.
Vaginal blood supply
the vaginal part of the cervix, portiovaginalis cervicis, and the upper part of the cervix, lying above the vagina, is called the supravaginal part of the cervix, portio supravaginalis cervicis.
On the vaginal part you can see the opening of the uterus, ostium uteri (uterine os), leading from the vagina into the canal of the cervix and continuing into its cavity.
The blood supply to the uterus occurs through the paired uterine artery, a branch of the internal iliac artery. Each uterine artery passes along the lateral edge of the uterus between the leaves of the broad ligament of the uterus, giving off branches to its anterior and posterior surfaces. Near the fundus of the uterus, the uterine artery divides into branches leading to the fallopian tube and ovary. Venous blood flows into the right and left uterine venous plexuses, from which the uterine veins originate, as well as veins flowing into the ovarian, internal iliac veins and venous plexuses of the rectum.
The vagina, vagina (colpos), is an unpaired hollow organ in the shape of a tube located in the pelvic cavity and extending from the uterus to the genital slit. At the bottom, the vagina passes through the urogenital diaphragm. The length of the vagina is 8-10 cm, the thickness of its wall is about 3 mm. The vagina is somewhat curved posteriorly, its longitudinal axis with the axis of the uterus forms an obtuse angle (slightly more than 90), open anteriorly.
The vagina with its upper end starts from the cervix, goes down, where its lower end opens into the vestibule with the opening of the vagina.
The vaginal arteries originate from the uterine arteries, as well as from the inferior vesical, middle rectal and internal genital arteries.
Venous blood from the walls of the vagina flows through the veins into the vaginal venous plexus, and from it into the internal iliac veins.
Dimensions of the uterus and structural features
A woman's uterus has different sizes. It all depends on what phase of the cycle the body of the fair sex is in. Normal sizes after the end of menstruation are in the range of 4 to 5 centimeters. In this case, the length of the organ may be slightly greater than the width and cross section.
The cervix in women who have never given birth and have not undergone dilatation of the cervical canal has a rounded shape and the same tightly closed opening. If a representative of the fair sex has already become a mother, then her cervix may have a slit-like opening, which is somewhat expanded. All this is a variant of the norm. The length of the cervical canal in different women can vary from 2 to 5 centimeters. Moreover, special attention is paid to this figure during pregnancy.
The female reproductive organ has an interesting feature. The uterus is not anchored by any devices or bones. Her body is held together only by ligaments and muscles. One can only imagine the stress these components undergo while carrying a child. The female uterus may be positioned correctly or may have anterior or posterior deviation. This is not a pathology, but problems with conception may occur.
Where is the cervix located?
Did you know that the stage of the ovulation cycle can be indicated by the cervix. Where it is is not so difficult to determine. This is the junction of the vagina and the body of the uterus. The cervix consists of supravaginal and vaginal parts. The lower end of the vaginal part ends with an opening, the edges of which form the anterior and posterior lips. The body of the uterus in cross-section resembles a triangle; its truncated lower angle continues into the cervix.
The internal canal of the cervix has glands that secrete vaginal mucus, the texture and color of which depend on the phase of the cycle, and are also an indicator of women's health. The cervix itself is located deep in the vagina, at a distance of approximately 7.5-15 cm, and is shaped like a donut with a small hole in the middle.
Now you know exactly where the uterus and cervix are.
The uterus is a unique link in the reproductive system, designed for the reproduction of offspring. Only women are endowed with this natural gift. The organ is located in the central part of the pelvic region. Physiologically, it is protected by the pelvic bones, muscle frame and fat layer, which protects it from possible damage.
Functions of the female uterus
The female reproductive organ has many important functions. Let's look at the main ones.
- One of the main functions that a woman’s uterus has is childbirth. Every month, the inner layer changes and is exposed to hormones. Thus, the body prepares for conception. If fertilization has occurred, then the embryo is securely attached to the wall of the female organ and remains there until full development and readiness for life in the external environment.
- In addition, the female uterus performs a cleansing function. Each menstrual cycle, the organ contracts, pushing the unnecessary inner layer out. It is during this period that a woman menstruates.
- The female reproductive organ also has a protective function. The uterus reliably protects the fragile fallopian tubes from the penetration of pathogens and infections. The cervix, in turn, secretes mucus, which helps flush these bacteria out of the cervical canal and vagina.
- The function of promoting sperm is also inherent in the female organ. After sexual intercourse, the uterus actively contracts, helping male gametes penetrate the cavity and enter the fallopian tubes for fertilization.
- Also, the female uterus can be assigned the function of supporting organs and various systems. Due to being in its usual place, the uterus does not allow the intestines and bladder to move in different directions.
Standards for VDM indicators
The norm is considered to be the correspondence between the week of pregnancy and the height of the uterine fundus in centimeters, plus or minus 2–3 centimeters. That is, at the 16th week, for example, the UMR is from 13 to 19 centimeters, at the 30th week it is approximately 27–33. After the 38th week, the baby begins to prepare for childbirth, the stomach drops and the UMR readings decrease - this is normal.
Table: WYD by week of pregnancy
| Term | Approximate indicators |
| 16 weeks | 14–18 cm |
| 20 weeks | 18–23 cm |
| 24 weeks | 22–27 cm |
| 28 weeks | 26–31 cm |
| 32 weeks | 31–33 cm |
| 36 weeks | 33–37 cm |
| 40 weeks | 34–35 cm |
Diseases of the female organ
Many representatives of the fairer sex have to deal with pathologies that affect the reproductive system. These include endometritis, fibroids, uterine prolapse in women and other diseases. Some of them can be safely treated and have a favorable prognosis. Others lead to such a horrifying conclusion as hysterectomy. Women who have had to undergo this procedure feel depressed and inferior. Let's look at a few examples of pathologies of the female organ.
Lecture 12. TOPOGRAPHIC ANATOMY OF THE PELVIC, PRINCIPLES OF OPERATIONS ON THE PELVIC ORGANS
Lecture outline:
1. - bone-ligamentous base of the pelvis, connection with neighboring areas;
2. - anatomical features of the female pelvis;
3. - floors of the small pelvis;
4. - course of the peritoneum in the pelvis, significance in pathology;
5. - fascia and tissue of the small pelvis;
6. — operations on the pelvic organs.
The pelvis, in terms of the relationship of bones, ligaments, muscles, vessels, nerves and organs located in it, is a very complex anatomical area. In general, it is very difficult to examine the pelvis topographically and anatomically, so its study is divided into separate sections, and, in addition, it is necessary to highlight the pelvic area in particular.
The bony pelvis consists of paired bones - the iliac, ischial and pubic bones and unpaired bones - the sacrum and coccyx. The first three pairs of bones in the area of the acetabulum grow together and form single pelvic bones, which are connected to the sacrum in the posterior section and form the pubic symphysis in front.
There are large and small pelvises, separated by boundary lines - linea terminalis. The bone parts lying above this line and represented mainly by the ilium are called the large pelvis, and the bones and ligaments lying below this line and forming a kind of canal together with the muscles are called the small pelvis. The entrance to the small pelvis is limited in front by the upper edge of the symphysis, on the sides by the boundary lines, and behind by the articulation of the 5th lumbar vertebra with the sacrum, which protrudes forward in the form of a cape - promontorium.
Exit from the pelvis
Bounded in front by the edge of the symphysis, on the sides - by the branches of the ischium and pubic bones, by the tuberosities of the ischium, lig. sacrotuberale, and behind - the coccyx. A large pelvis provides support for the torso, abdominal muscles, back, and lower limbs. The small pelvis is the container for the rectum and genitourinary organs; in women it is also the birth canal.
In general, the pelvic bones form a strong closed ring. So strong that the basin can withstand pressure of more than 250 kg. The joints of the pelvic bones are especially strong, so in case of injuries, fractures are more often observed in places where the pelvic bones are thin and narrow - these are the branches of the pubic and ischial bones, i.e. in the area of the obturator foramen. Typically, pelvic fractures occur when large forces are applied, i.e., this is usually a traffic injury, a fall from a great height, or accidents in the mining industry.
The severity of pelvic fractures is due to three anatomical reasons:
- rapidly developing anemia due to bleeding from the spongy bones and venous plexuses of the pelvis;
- multiple fractures, double fractures with disruption of the pelvic ring are more common;
- damage to the pelvic organs (rectum, bladder, urethra, vagina in women).
In addition to two large openings in the pelvis (inlet and outlet), there are relatively small openings:
- obturator foramen , formed by the ischium and pubic bones; the opening is covered by the membrana obturatoria, in the upper part of which there is an obturator canal, which passes the obturator vessels and nerve to the thigh; Thus, the significance of the canal is that through it the pelvic tissue is connected to the thigh area; this channel is the path for the spread of urinary leaks and hematomas in case of fractures of the pelvic bones with damage to the bladder or urethra; the famous Russian surgeon Buyalsky proposed to drain pelvic phlegmon through an incision on the thigh and then through the obturator membrane;
- in the posterior-inferior part of the pelvis there are two openings, limited by the sciatic notch and ligaments (lig.
sacrospinale, sacrotuberale) – greater and lesser sciatic foramina . The greater sciatic foramen is divided by the piriformis muscle into two small openings - foramen supra - and infrapiriformis.
The superior gluteal vessels and nerves pass through the supragiriform foramen, and the inferior gluteal vessels and nerves, the sciatic nerve, the posterior inferior nerve of the thigh and the internal pudendal neurovascular bundle pass through the inferior foramen.
The latter, having gone around the lig.sacrospinale, is directed into the lesser sciatic foramen inside the small pelvis into the ischiorectal fossa. The significance of the marked holes is that through them there is also a spread of purulent leaks due to pelvic phlegmon and hematomas into the gluteal region and the posterior bed of the thigh.
The female pelvis has significant differences from the male pelvis - they are determined by the anatomical and physiological characteristics of the female body:
- the female pelvis (cylinder) is wider and lower than the male (cone) pelvis; the walls of the pelvis are flattened and the wings of the iliac bones diverge more to the sides;
- the sacrum is flatter and wider, removed posteriorly, thus increasing the capacity of the small pelvis;
- the angle of inclination of the pelvis (inclinatio pelvis - the angle between the axis of the pelvis and the horizontal plane from 45 to 60 degrees in some women) is greater in women; in men, the pelvic axis is more vertical;
- angulus subpubicus in men is less than a right angle (75 degrees), in women it approaches or exceeds a right angle (95-100 degrees);
— the shape of the entrance to the small pelvis is especially characteristic: in women, the promontory almost does not protrude into the pelvic cavity, so the opening is round; in men, the shape of the hole resembles a card heart;
- the obturator foramen of the female pelvis is similar in shape to a triangle, the male - to an oval, the long axis of which is directed vertically;
— the distance between the ischial tuberosities is more than 11 cm;
- the acetabulum is turned anteriorly.
Great importance is attached to the size of the female pelvic bone in obstetrics.
The direct size of the entrance to the pelvis, i.e. the distance between the upper inner edge of the pubic symphysis and the promontories is 11 cm. This is the so-called true conjugate - conjugata vera. There is also an anatomical conjugate - the distance between the promontory and the upper edge of the articulation is 11.5 cm. The transverse dimension of the plane of the entrance to the pelvis is equal to half the distance between the distant points of the iliac crests, i.e. - 13 cm.
There are three floors in the pelvic cavity:
- peritoneal floor - cavum pelvis peritoneale;
- subperitoneal floor - cavum pelvis subperitoneale;
- subcutaneous floor - cavum pelvis subcutaneum.
The first floor of the small pelvis is peritoneal, limited at the top by the plane of the entrance to the small pelvis.
This is the lowest part of the peritoneal sac.
The course of the peritoneum in the pelvis. From the anterior wall of the abdomen, the peritoneum passes to the bladder, forming a transitional fold. Thus, the anterior wall of the bladder is almost not covered by peritoneum, and when filled, the bladder rises upward, and the part of it not covered by peritoneum significantly extends from behind the womb, pushing the peritoneal sac upward.
Therefore, when filling the bladder, if for some reason it is not possible to remove urine with a catheter, you can puncture it to remove urine by puncturing the midline 2 cm above the pubis.
Extraperitoneal access to the bladder is based on the same feature. In men, the peritoneum passes from the bladder to the rectum with the formation of a notch - excavatio vesicorectalis. In the female pelvis, the peritoneum passes from the bladder to the anterior surface, bottom and posterior surface of the body of the uterus and vagina. It is very important that the top 1-2 cm of the posterior wall of the vagina is covered with peritoneum. Then the peritoneum passes to the rectum. Thus, two recesses are formed in the female pelvis: the vesico-uterine (excavatio vesicouterina), relatively shallow, and the deeper one, the uterorectal (excavatio rectouterina - Douglas space).
The practical significance of these spaces is that they are the most sloping place in the peritoneal sac, where pus accumulates and residual abscesses form in the abdominal cavity during peritonitis.
In men, pelvic abscesses are often a consequence of acute purulent appendicitis, and in the female pelvis - more often due to inflammation of the uterine appendages.
Diagnosis of pelvic abscesses in men begins with a digital examination of the rectum and, if there are signs of abscess formation, a puncture is performed. When pus is obtained, the vesico-rectal space is opened and drained through the rectum.
The diagnosis of pelvic abscess in women begins with a vaginal examination. If there are signs of abscess formation, a puncture of the posterior vaginal fornix is performed. Upon receipt of pus, opening and drainage of the rectal-uterine space is performed through the vagina. Puncture of the posterior vaginal fornix is also used to clarify the diagnosis of an interrupted ectopic pregnancy.
It should be noted that the peritoneum does not cover the lateral surfaces of the uterus (ribs), but in the form of a double fold stretches to the lateral walls of the pelvis. This is the so-called wide uterine ligament, on the back side of which the uterine appendages are located - tubes and ovaries.
The second floor of the small pelvis, subperitoneal, is limited at the top by the lower surface of the peritoneal sac, and at the bottom by the pelvic diaphragm. In the second floor, the organs and walls of the pelvis are covered with fascia and surrounded by loose and fatty tissue.
Pelvic fascia:
- pelvic fascia; - prevesical plate;
- peritoneal-perineal aponeurosis (Denonvilliers-Salishcheva).
The pelvic fascia, the main fascia of the pelvis, is a continuation of the intra-abdominal fascia.
It has two leaves. The parietal layer of the pelvic fascia lines the walls of the pelvis.
We especially note that the parietal layer of the pelvic fascia fixes the neurovascular bundles of the pelvis to the walls of the pelvis through spurs and forms the sheath of the neurovascular bundles. Thanks to this, in case of pelvic injuries, the vessels do not collapse - massive hematomas are formed. Next, the parietal leaf forms a tendinous arch, from which the levator ani muscle begins, covers it on both sides, forming a vagina for it.
Two layers of pelvic fascia and m. levator ani form the pelvic diaphragm. Under the symphysis m. The levator ani is absent, and a triangular-shaped space is formed where two leaves of the pelvic fascia, covering the muscles, grow together into a strong membrane, the edges on the perineal side are strengthened by the muscles of the perineum.
This is the so-called urogenital diaphragm.
Thus, the pelvic diaphragm has:
- muscular part (pars muscularis);
- membranous part (pars membranacea or trigonum urogenitale).
The pelvic diaphragm divides the pelvic canal into upper and lower sections; two floors above and two below.
From the walls, the pelvic fascia passes to the organs.
This part of the pelvic fascia is called the visceral layer. It runs in the form of two spurs in the sagittal plane from the sacrum to the pubis, the sacro-pubic plates. Thus, the pelvic organs are enclosed between two sacro-pubic plates on the sides, the symphysis in the front and the sacrum in the back. In addition, there are two more fascia in the pelvis, which are visceral fascia and lie in the frontal plane.
The prevesical plate lies in front of the bladder, is formed from the embryonic peritoneum, has the shape of a triangle, limited on the sides by obliterated umbilical arteries. The peritoneal-perineal aponeurosis (Denonvillier-Salischev aponeurosis) is a fascia that has a dense fibrous appearance, located between the vagina and rectum in women, and between the prostate gland and the rectum in men.
The aponeurosis divides the pelvis into anterior and posterior sections. Due to the presence of sagittal plates and two visceral fasciae, the pelvic tissue is divided into cellular spaces.
The visceral layer of the pelvic fascia forms capsules of organs with spurs. Ligaments with the parietal leaf fix the pelvic organs to the walls. The spurs usually go along the vessels.
Inflammatory processes may form in the cellular spaces around organs. Typically, inflammation occurs as a result of extraperitoneal damage to the bladder during pelvic fractures, the so-called urophlegmon. Their opening is performed with a transverse suprapubic incision (Rhine), or an incision along the inner surface of the thigh under the inguinal ligament with perforation of the membrana obturatoria (Mack Water-Buyalsky approach).
In the female pelvis, the visceral layers of the pelvic fascia surrounding the uterus and vagina reach the lateral walls of the pelvis, forming the so-called anchoring apparatus of the uterus: cardinal, uterosacral, vesico-pubic ligaments.
The third floor of the pelvis is located between the pelvic diaphragm, its lower surface, and the skin.
On the sides of the rectum, this is where the largest fiber space of the pelvis is located. It includes the fiber lying in the ischiorectal fossa, fossa ischiorectale. It is here that purulent-inflammatory processes near the rectum are most often localized - paraproctitis.
This is one of the most common diseases of the rectum. Based on the localization of abscesses in the tissue near the rectum, the following types of paraproctitis are distinguished: - ischiorectal (the most common); - subcutaneous; —submucosal; -pelviorectal (the most dangerous, anaerobic); - retrorectal.
The paraproctitis is opened with an arcuate incision on the side of the rectum.
CELLULAR SPACES OF THE SMALL PELVIS
| Parietal | Visceral |
| 1. Lateral (2). 2. Proper prevesical (Retsia). 3. Posterior rectum. | 1.Prevesical preperitoneal. 2.Perivesical. 3. Posterior vesicle. 4. Pararectal (Amuse fat capsule). 5. Circumferential. 6. Prostate capsule (Pirogov-Retsia). |
Uterine rabies (nymphomania)
Uterine rabies in women is a process in which the mental state is disturbed. This disease is often called hysteria. This name is now obsolete. Modern medicine does not recognize such a disease as uterine rabies in women. The symptoms of the pathology remained. Most often, the disease manifests itself as increased sexual desire, clouding of consciousness, laughter followed by tears. Now such women are called nymphomaniacs and are prescribed psychological correction.
Location Features
The uterus is an unpaired muscular organ that, along with the ovaries, represents the female reproductive system. Visually, the uterus is similar to a cone or an inverted pear. The reproductive structure is represented by:
In the place where the vagina ends, there is a cervix - the lower part of the organ, similar to a cylindrical tube, three centimeters long. Cervical parameters are not constant, values vary during pregnancy and in old age.
Inside the cervix there is a narrow cervical canal. The cervical canal is the connecting element between the uterus and vagina.
Above the cervix is the uterine body, the place where the embryo develops. The body of the uterus is represented by thick walls (about three centimeters), consisting of three layers.
- Mucous – endometrium. Inner lining of the cavity. It is the endometrium that is involved in the formation of menstruation, being shed monthly if pregnancy does not occur. But if conception has occurred, then the fertilized egg also clings to the endometrium.
- Muscular - myometrium. This layer provides muscle contractions during contractions. It also contracts after sexual intercourse, facilitating better penetration of sperm.
- Serous – perimetry. This is the peritoneal membrane covering the outside of the organ.
The fundus is located at the very top of the organ, in the place where the openings of the fallopian (uterine) tubes are located.
The woman’s womb is not fixed, it is in a “suspended” state: the necessary position is provided by the ligaments holding the uterus. So, where is a woman's uterus?
Removal of the reproductive organ
There are several ways to remove the uterus. Depending on the capabilities of the medical institution and the qualifications of doctors, the most suitable option is selected. The most common procedure is laparoscopic surgery. However, there are times when a laparotomy is required. Let's consider both of these options.
Removal of the uterus using a laparoscope
If you have time to prepare for surgery, then it is preferable to perform this procedure. During the operation, the doctor makes several incisions in the patient's abdomen and inserts small manipulators into them. Using a video camera, the doctor sees everything that is happening on a large monitor. Small manipulators carefully cut the ligaments and muscles that support the uterus. After this, the organ is removed from the abdominal cavity.
Recovery after such an operation is quick. However, a woman may experience discomfort and pain during the first month after the procedure.
Laparotomy surgery to remove the uterus
If the procedure for removing an organ from the peritoneum is urgent, then laparotomy is performed. This method is also chosen when a woman has a large layer of fat in the pelvic area. During the operation, the doctor makes an incision in the lower abdomen. It can be horizontal or vertical depending on the situation. After removing the reproductive organ, the incision is sutured layer-by-layer.
Recovery after such an operation is much more difficult. The woman is incapacitated for one month after the procedure.
Pathologies [edit | edit code]
Developmental anomalies [ edit | edit code ]
- Aplasia (agenesis) of the uterus
- extremely rarely, the uterus may be completely absent. There may be a small infantile uterus, usually with a pronounced anterior incursion. - Duplication of the uterine body
is a defect in the development of the uterus, which is characterized by duplication of the uterus or its body, which occurs due to the incomplete fusion of two Müllerian ducts at the stage of early embryonic development. As a result, a woman with a double uterus may have one or two cervixes and one vagina. With complete nonfusion of these ducts, two uteruses with two cervixes and two vaginas develop. - Intrauterine septum
- incomplete fusion of the embryonic rudiments of the uterus in various variants, can lead to the presence of a septum in the uterus - a “bicornuate” uterus with a clearly visible sagittal depression at the bottom or a “saddle-shaped” uterus without a septum in the cavity, but with a notch at the bottom. With a bicornuate uterus, one of the horns may be very small, rudimentary, and sometimes unlaced. - Hypoplasia is underdevelopment of this organ in a woman. In this case, the uterus is smaller than it should be normally.
What happens to the female body after surgery?
After removal of the uterus, a woman changes not only internally, but also externally. Most representatives of the fair sex note an internal emptiness in moral and physical terms. If a woman is of childbearing age, then in addition to depression, she feels helpless and useless.
After hysterectomy, many women are recommended hormone replacement therapy. This treatment allows you to maintain internal ligaments and muscles in tone.
Functions of the uterus in a woman’s body
A woman’s body is unique, because only the fair half of humanity is endowed with a uterus. This organ performs significant functions, the main one of which is childbirth.
The uterus is a smooth muscle hollow organ in a woman’s body, created for the development of the embryo and its birth. It is localized in the pelvic area between the rectum and bladder. When a fertilized egg enters the uterine cavity, pregnancy occurs. This generative function of the uterus in women is dominant, but not the only one.
The mother's womb consists of a body, cervix and fundus. The body is shaped like a triangle, and gradually narrows closer to the neck. The structural organization of the body is represented by muscle fibers, the contraction of which causes contractions.
The uterine walls consist of three layers, each of which performs significant functions.
- Perimetry (external). This is the peritoneum, which is fused with the muscular organ and covers it. The structure forms the serosa.
- The myometrium is a muscular layer that makes up the main part of the walls.
- Endometrium (internal) is a mucous membrane supplied with glands. It is this layer that provides menstrual function. Every month, the mucous membrane “prepares” for conception. In the absence of fertilization, the endometrium, along with the blood, descends into the vagina.
Ligamentous apparatus of the uterus during pregnancy
• The preservation of certain topographic relationships of the internal genital organs is ensured by the presence of: suspensory;
• fixing;
• supporting devices.
The unique function of these devices is such that, while holding the uterus and appendages in a certain position, they at the same time ensure their mobility within significant limits, which is necessary for the normal development of pregnancy and the course of labor.
The suspensory apparatus of the uterus and its appendages is represented by paired ligaments that connect these organs to each other and to the walls of the pelvis (Fig. 1.1.9):
Rice. 1.1.9. Suspension apparatus of the uterus
1) broad uterine ligament
(lig. latum uteri) - a transverse fold of the peritoneum covering the body of the uterus and tubes, making up their serous cover and the mesentery of the tubes. The broad ligaments go to the lateral walls of the pelvis, where they pass into the parietal peritoneum. The ovaries are located on their posterior surface in the lateral sections;
2) suspensory ligament of the ovary
(lig. suspensorium ovarii) - the outer part of the broad ligament, going from the ovary and the ampullary part of the tube to
Rice. 1.1.10. Fixing apparatus of the uterus:
lateral wall of the pelvis. The relative strength of this ligament is explained by the vessels passing through it (a. et v. ovarica);
3) ovarian ligament
(lig. ovarii proprium) passes through the thickness of the posterior sheet of the broad ligament from the uterine pole of the ovary to the uterus. The presence of smooth muscle elements and the passing ovarian branches of the uterine arteries and veins determine the strength of the ligament;
4) round ligament of the uterus
(lig. teres uteri) is a cord 10-15 cm long, 3-5 mm in diameter, consisting of smooth muscle and connective tissue. The round ligaments begin anteriorly and inferiorly from the tubal angles of the uterus and run under the anterior leaves of the broad ligaments in the inguinal canals, branching in the thickness of the labia majora.
The fixing apparatus of the uterus consists of (Fig. 1.1.10):
1. transverse (main) ligament of the uterus
(lig. transversum uteri, s. lig cardinale), consisting of a network of radially located smooth muscle and connective tissue elements surrounding the neck at the level of the internal pharynx. The fibers of the main ligament are woven into the pelvic fascia, fixing the uterus to the pelvic floor;
2. vesicouterine
(lig. vesiconterinum) and
pubovesical ligaments
(lig. pubovesicalia) - smooth muscle and connective tissue fibers running from the lower part of the anterior surface of the uterus to the bladder and pubis;
Rice. 1.1.11. Perineum
3. uterosacral ligaments (lig. sacrouterina), consisting of smooth muscle and fibrous fibers. They come from the posterior surface of the cervix, slightly below the level of its internal pharynx, cover the rectum from the sides and merge with the pelvic fascia on the inner surface of the sacrum.
In a woman standing, the uterosacral ligaments are directed almost vertically and support the cervix.
The suspensory and fixing ligaments of the uterus stretch during pregnancy, ensuring the mobility of the uterus within the limits necessary for its growth.
The supporting apparatus of the female internal genital organs is the muscles and fascia of the perineum, which make up the pelvic floor. The pelvic floor muscles are divided into three layers (Fig. 1.1.11):
• external;
• average;
• internal.
In outdoor
The layer includes the following muscles:
• ischiocavernosus muscle (m. ischiocavernosus) - steam muscle, running from the ischial tuberosities to the clitoris;
Rice. 1.1.12. Arteries of the pelvic organs:
• bulbospongiosus muscle (m. bulbospongiosus) - a paired muscle that covers the entrance to the vagina on both sides;
• the external muscle that compresses the anus (m. sphincter ani externus) surrounds the lower part of the rectum in a ring;
• the superficial transverse muscle of the perineum (m. transversus perinei superficialis) is usually poorly developed. This is a paired muscle that runs from the inner surface of the ischial tuberosity to the tendon center of the perineum, where it connects with the muscle of the same name on the other side.
Average
The layer of muscles of the perineum, called the urogenital diaphragm (dfaphragma urogenitale), includes:
• muscle that compresses the urethra (m. sphincter urethrae externum);
• deep transverse muscle of the perineum (m. transversus perinei profundus), paired, located in the triangle between the symphysis, pubic and ischial bones.
Interior
The layer of pelvic floor muscles, or the pelvic diaphragm (diaphragma pelvis), is formed by the levator ani muscle (m. levator ani). This is a powerful, well-developed muscle, consisting of three paired bundles (legs):
• pubococcygeus muscle (m. pubococcygeus);
• iliococcygeus muscle (m. iliococcygeus);
• ischiococcygeus muscle (m. ischiococcygeus).
During childbirth, the perineum is often injured, and it is the inner layer of the pelvic floor that is damaged. These muscles must be sutured most carefully, since the inner layer of the pelvic floor is most important in maintaining the position of the vagina and uterus.
The muscles and fascia of the pelvic floor perform the following essential functions:
• The pelvic floor provides support for the internal genital organs and helps maintain their normal position. The levator ani muscles are of particular importance. When these muscles contract, the genital fissure closes, narrowing the lumen of the rectum and vagina. Damage to the pelvic floor muscles leads to prolapse and prolapse of the genital organs, as well as the bladder and rectum.
• The pelvic floor provides support not only for the genitals, but also for the internal organs. The pelvic floor muscles are involved in the regulation of intra-abdominal pressure together with the thoraco-abdominal diaphragm and the muscles of the abdominal wall.
• During childbirth, when the fetus is expelled, all three layers of the pelvic floor muscles stretch and form a wide tube, which is a continuation of the bony birth canal. After the birth of the fetus, the pelvic floor muscles contract again and return to their previous position.
Functional values
Nature has endowed a woman with the unique ability to give birth. This function of the uterus in a woman’s body is paramount. Menstrual and endocrine functions are also distinguished, each of which complements and interacts with the other.
Generative purpose
The ability to conceive, bear and give birth to offspring is the main unique ability of the uterus. During the period of bearing a child, significant changes occur in the organ:
- the size and shape changes: asymmetry disappears, the shape takes on an oval shape;
- the wall thickness changes. If before pregnancy they reach 3 cm, then during pregnancy they thin out to 1 cm;
- weight increases. In the body of a non-pregnant woman, the uterus weighs about 50 grams, and by the end of the term - almost 1.5 kilograms.
In addition, the ovaries change their functioning - they actively synthesize estrogens, and in the early stages - progesterone. When the placenta is formed, it takes over the production of progesterone. Significant changes also affect the cervix. During normal periods, the cervical canal is smooth, elastic, and pink in color. After the birth of life, the canal glands grow rapidly, produce mucus, and the surface becomes bluish. In the last weeks of pregnancy, the cervix is characterized by softness and shortens, which means its maturity and the body’s readiness for the birth process.
Menstrual function
Only the female body is endowed with a similar property - a cyclical menstrual process. Such physiological activity of the uterus is the result of the absence of pregnancy. Cycling is regulated by the hypothalamus, pituitary gland and ovaries. The thyroid gland also plays an important role.
The cycle is divided into two phases:
The first phase is characterized by the rejection of the endometrium with bloody discharge. This may be accompanied by painful sensations. The duration of this period is on average seven days. After this, a new layer of endometrium grows - it actively proliferates. This process is regulated by hormones such as FSH and estradiol.
At the second stage after ovulation, preparation for pregnancy occurs. The mature egg moves through the fallopian tubes into the uterine cavity. This process lasts about 2 weeks, accompanied by the synthesis of progesterone. The amount of estradiol and FSH decreases, the level of LH and progesterone increases. In the absence of fertilization, the next cycle begins.
Pathologies such as PCOS, MFJ, endometrial hyperplasia, hypothyroidism, adrenal diseases, and hyperandrogenism have a significant impact on menstrual function.
Gynecological abnormalities
The norm is for the uterine and pelvic axis to be parallel to each other. A slight deviation from the axis is not considered a pathology. However, with some dysfunctions, the localization of the uterus and appendages changes, and a significant deviation from the axis is observed. Such diseases include prolapse, bending or prolapse of the uterus.
The uterine location depends on the muscle fibers that hold it. If muscle tone weakens, prolapse occurs. Without proper treatment, complete loss may occur. At the initial stage of uterine prolapse, it is recommended to perform Kegel exercises. This will avoid loss and surgical interventions.
The female reproductive system is susceptible to dysfunction and various types of pathologies. The most common ones include:
The modern medical base has a wide range of possibilities for curing almost any ailment. The main factor in successful therapy and prevention is constant monitoring of the state of the reproductive system.
Uterine anomalies are quite rare, however, they do exist.
- Double uterus. Combined with double vagina. This pathology is often diagnosed along with other defects: pathologies of the kidneys and ureters.
- Two-horned. Bicornus is characterized by varying degrees of severity. Visually, the uterus is similar to the shape of a heart.
- One-horned. This defect occurs due to incomplete development of the uterine (Müllerian) canal. Women experience pain during sexual intercourse and are unable to become pregnant.
- Saddle. In this case, only the fundus of the uterus is abnormally divided: an unusual depression is formed in it. A woman is able to conceive, but there are problems with pregnancy.
- Uterus with septum. With this pathology, the shape of the organ remains normal, but the cavity is separated by a partial or complete septum.
The described disorders of the anatomical structure of the female reproductive system are not diagnosed so often. The most common anomaly is the saddle uterus.
Every woman must know where the uterus is and understand its functions and features. This knowledge will help to avoid pathological complications and identify the disease at the initial stage.
Uterus
(Latin uterus, Greek ὑστέρα) is an unpaired smooth muscle hollow organ in which the embryo develops and the fetus is born. The uterus is located in the middle part of the pelvic cavity, the bladder lies in front, and the rectum lies behind, mesoperitoneally. From below, the body of the uterus passes into a rounded part - the cervix. The length of the uterus in a woman of reproductive age is on average 4-7 cm, width - 4 cm, thickness - 4-5 cm. The weight of the uterus in nulliparous women ranges from 40 to 60 g, and in those who have given birth reaches 80 g. Such changes arise due to for muscle hypertrophy during pregnancy. The volume of the uterine cavity is ≈ 5 - 6 cm³.
The uterus as an organ is largely mobile and, depending on the condition of neighboring organs, can occupy different positions. Normally, the longitudinal axis of the uterus is oriented along the axis of the pelvis (anteflexio). A full bladder and rectum tilt the uterus forward into the anteversio position. Most of the surface of the uterus is covered by the peritoneum, with the exception of the vaginal part of the cervix. The uterus is pear-shaped and flattened in the dorsoventral (antero-posterior) direction. Layers of the uterine wall (starting with the outer layer): perimeter, myometrium and endometrium. The body just above the isthmus and the abdominal part of the cervix are externally covered with adventitia.