Everywhere among Patients there is an opinion that if you have been diagnosed with cancer or pre-cancer, then you need to have surgery. The gynecologist gives a referral to an oncologist and there, in the old fashioned way, the woman is sent for surgical treatment. This is not always justified and there is a progressive treatment method called photodynamic therapy (PDT).
PDT (photodynamic therapy) is an organ-preserving method of treating cancer, based on the ability of photosensitizers to selectively kill tumor cells under the influence of light.
Photodynamic therapy for cervical dysplasia
Today, many women suffer from dysplasia, a precancerous pathological condition of the cervix. This disease is treated in a variety of ways, from medications to surgery. Radical measures are taken only in critical situations with a high risk of damaged cells degenerating into cancerous ones. In any case, the main goal of doctors is to preserve reproductive health in women.
The tactics of the chosen treatment directly depend on each individual case and the degree of development of the pathology. Photodynamic dynamics is one of the frequently used tools in the fight against dysplasia, which is able to carefully remove damaged areas of the cervix, while minimally affecting healthy tissue.
But can all women use this method? Does PDT have any obvious disadvantages? Let's try to understand these issues together with the reader.
Indications and contraindications for the use of FTD
Indications for FTD are such gynecological pathologies as:
• Erosion damage; • Cervical endometriosis; • Dysplasia I and II degrees; • Leukoplakia, in which there is coarsening of the mucosa; • Cervicitis or inflammation; • Ectropion (a disease in which there is a protrusion of the cervical canal, observed during examination of the vagina); • Retention cysts. The use of FTD in the primary stages of pathology development is the only solution that allows you to quickly and without any complications get rid of diseases, thereby protecting yourself from cancer. FTD cannot be used by persons: • Those who are at the stage of bearing a child; • Those who have acute inflammatory processes in the genital tract; • Having diseases of the kidneys, liver and cardiovascular system; • Those whose skin has increased photosensitivity; • Individual intolerance to drugs used during the procedure and diffuse mastopathy. Unfortunately, if one of the contraindications is present, FTD cannot be used. After all, this can be harmful to health and complicate the course of existing diseases.
How is FTD carried out?
Several components are used to carry out FTD:
• Gel penetrator; • Laser equipment. First, a penetrator gel is applied to the affected area by application, which is left to act for one hour. During this time, the active substances contained in the drug “tag” diseased cells, penetrating them and triggering a chemical reaction with oxygen. And then the cervix is irradiated using laser equipment for 10–20 minutes. The timing of the procedure to treat the cervix depends on the extent of the disease and the area it covers. The larger the treatment area, the longer the irradiation lasts.
Treatment of diffuse mastopathy with gestagens >>>
After completing the FTD, the woman can immediately go to her home and take care of her daily routine. Women undergo gynecological examinations every other day, on the 7th day and every 30 days for three months. Wound healing, as a rule, occurs only after 28–40 days. During this time, the woman may experience slight bleeding from the vagina and pain when the abdominal cavity is tense. As practice shows, most patients experience tingling and pinching during the procedure. Only 1/3 of women complained of severe pain and burning. In case of severe pain in the cervix, the use of local painkillers cannot be ruled out. To prevent the development of phototoxic reactions, the woman is informed in advance about the importance of observing the light regime several days before and after the PDT. What should you not do after FTD?
Highly not recommended after FTD
• Engage in sexual intercourse; • Take a hot shower or bath (possible bleeding); • Lift more than 3 kg; • Visit swimming pools, saunas and steam baths, as well as swim in ponds and rivers (there is a high probability of infection). A woman who has undergone PDT is strongly advised not to disregard these recommendations, because this may lead to a slowdown in the recovery process. After using the laser, a wound appears on the cervix. If you lift something heavy or have sexual intercourse, it may burst, which can lead to the development of inflammatory and infectious diseases. In addition, this threatens the opening of bleeding, the development of a purulent process and other complications. Therefore, you should check with a specialist for a detailed list of restrictions.
Treatment of fibrous mastopathy - treat or operate? >>>
About photodynamic therapy
In Russia, photodynamic therapy began to be used in 1992. The purpose of this method is to combat malignant tumors, but gradually PDT began to be used in the fight against diseases such as dysplasia. Today, an innovative method of treatment makes it possible to achieve an antitumor, antibacterial, regenerating or immunostimulating effect.
How is photodynamic therapy of the cervix done?
The PDT procedure consists of two stages:
- At the initial stage, the photosensitizer is administered in one of the following ways: externally in the form of a gel, taking the powder orally, or intravenously in the form of a solution. The main feature of the drug is the ability to accumulate only in affected cells, separating them from healthy tissues.
- Approximately 1.5-2 hours after taking the medicine, the doctor performs a laser treatment procedure, affecting only the source of the pathology.
This joint method is based on the action of chemical reactions, as a result of which damaged tissue is rejected and replaced with connective tissue.
What should you expect during and after photodynamic therapy of the cervix?
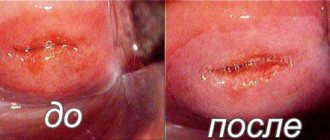
Photodynamic therapy is a fairly effective and safe way to combat cervical erosion when compared with the usual “cauterizations”. During the procedure, the woman is completely safe - PDT is performed without incisions, without injuries, without toxic effects, without the risk of bleeding and virtually without pain. Depending on the extent of the lesion, the patient is offered local or general anesthesia.
What kind of pain relief is used during photodynamic therapy of the cervix?
To minimize pain during PDT treatment, doctors use anesthesia. The choice of local or general anesthesia depends on the time of intervention and the complexity of each procedure.
The healing process is accompanied by light bleeding and does not cause much discomfort to the woman. As a result of such an operation, no scars remain on the cervix, its natural integrity and elasticity are preserved, which is especially important for expectant mothers.
On what day of the cycle is it better to perform photodynamic therapy of the cervix?
A PDT session is carried out either before the start of the menstrual cycle or immediately after its end. This allows you to preserve the natural process of epithelization of the cervix, and menstruation does not interfere with it.
Reference. When a woman is diagnosed with early stage cervical cancer, photodynamic therapy sessions are carried out 5 days or less before the arrival of the next cycle.
How many photodynamic therapy treatments of the cervix are needed for complete cure?
The number of PDT procedures required to completely get rid of cervical pathology is an individual question. As a rule, the positive effect of treatment lasts from several months to several years. But some women with a more severe degree of dysplasia are prescribed repeated treatment with a course of up to 5 PDT sessions. After such therapy, long-term remission occurs in 70% of cases. Relapses occur in an average of 7% of patients.
Sexual rest after photodynamic therapy of the cervix?
Do not forget that PDT is an operation, albeit without stitches, cuts and blood. Young epithelium is immature and very susceptible to infection and injury. Doctors recommend maintaining sexual rest for two months after the procedure to avoid prolonging the healing period.
Habitual lifestyle after photodynamic therapy of the cervix?
After the PDT procedure, doctors recommend the following:
- avoid prolonged exposure to the sun;
- wear glasses and clothing that covers the body as much as possible;
- do not take a hot bath and avoid visiting saunas and baths;
- Temporarily observe sexual rest.
A woman can return to her usual image after 1-2 months, but in any case after a gynecological examination by the attending physician.
Disadvantages of photodynamic therapy of the cervix
If we talk about the disadvantages of this method of treatment, we can only note a number of contraindications, the presence of which prohibits the use of FCT. These include:
- pregnancy;
- chronic diseases of the liver, kidneys and cardiovascular system;
- an inflammatory process in the genital organs that occurs in an acute form.
Another disadvantage is the fairly high price of such a procedure.
Alternatives to photodynamic therapy for the cervix
Dysplasia is treated using both PDT and alternative methods:
- diathermocoagulation;
- radio wave destruction;
- cryodestruction;
- laser vaporization.
Such methods of treating cervical pathologies are quite effective, but still have many disadvantages. Their use can lead to a number of complications in the form of bleeding, the development of endometriosis and cause problems with further bearing a child.
How does a session of photodynamic therapy of the cervix work?
If the doctor plans to administer a photosensitizer intravenously, it is recommended to perform the procedure in a semi-dark room. This will allow the drug not to react to artificial and daylight.
Having provided the office with minimal lighting, the doctor waits for the time during which the drug accumulates in the patient’s affected cells. Usually it is about two hours.
The most crucial moment is the treatment of the cervix with a laser beam, which allows you to launch photochemical reactions in the mucous membrane of the cervix. The operation lasts from 30 to 90 minutes, depending on the complexity and extent of the lesion.
The total time for performing PDT takes from 2.5 to 4 hours.
Benefits of photodynamic therapy of the cervix
Clearly, the method of treating dysplasia using PDT has many advantages. Here are the main advantages:
- rapid rehabilitation after the intervention;
- minimum pain;
- preservation of reproductive functions in women;
- no complications after PDT;
- the ability to cure cervical dysplasia in one procedure;
- no age contraindications;
- the ability to perform surgery under local anesthesia.
Disadvantages of photodynamic therapy of the cervix
Like any intervention, PDT has a number of disadvantages:
- presence of contraindications;
- high demands on the professionalism of the doctor performing the PDT procedure;
- risk of damaging healthy tissue;
- the need to wear sunglasses 2-3 days after the procedure;
- high cost of the service.
Lecture “How to avoid becoming a victim of a gynecologist”
Modern medicine in Russia is gradually turning into a wide fair of folk, or more precisely, “medical creativity.” Various methods and approaches to treatment are created in numerous departments of medical universities, where they gain their legitimacy by defending dissertations and writing methodological recommendations. Numerous attempts to create standards or regulated recommendations for everyone have not been successful - there is a dull feudal fragmentation)
Under these conditions, it is not at all difficult to promote various treatment methods even if they diverge from the principles of evidence-based medicine, since one can always refer to the “unique Russian experience.”
We will talk about a treatment method that is gaining popularity in our country - photodynamic therapy (PDT).
The idea of the method is extremely interesting and, at first glance, encouraging. A substance is introduced into the body that accumulates in all cells of the body - healthy and sick. This substance is eliminated from healthy cells faster than from pathological cells, so they wait for some time after administering the substance. Next, a focused beam of light of a certain wavelength (laser) is directed to the affected tissue. As a result, cells that have accumulated this substance die. Since the light source must be brought directly to the affected tissue, only superficial diseases can be treated with this method. In particular, PDT is used for certain skin diseases. In America, PDT is approved only for a few diseases: esophageal cancer, Barrett's esophagus, large cell lung cancer and cutaneous keratoses. PDT is actively practiced in South Korea, China and Japan. According to literature reviews, PDT is being used to treat a very wide range of diseases, but I would like to focus on the treatment of the cervix.
Let me immediately make a reservation that PDT is not included in the national recommendations for the treatment of cervical pathology in most countries of the world, even as an alternative treatment method. What is treated on the cervix?
Let me briefly remind you of the essence of the issue.
Oncogenic types of human papillomavirus (HPV) can cause changes in cervical cells. Cells affected by the virus are called “atypical”, and the process of cell changes is called “dysplasia”. As recent studies have shown, the relationship between the virus and our body can proceed in different ways. The first and most common option is that HPV infection develops like a regular viral infection, for example, the flu, but it lasts not a week, but several years. That is, initially, as with the flu, a complete recovery is expected without any consequences. Another option is when the onset of a viral infection in the process of its development begins to give complications that can even lead to death or serious consequences. This unpleasant course of influenza is primarily due to the state of a person’s immunity at the time of infection and other changes in the body that do not allow one to actively resist the virus.
Now we move from the example of influenza to the cervix, but before we talk about damage to the cervix, I need to explain the terms that I will use.
First, let's talk about how we study the condition of the cervix. Imagine that the true state of the cervix is a picture, for example, “Morning in a pine forest.” We need to solve it. The painting is covered with an opaque matte film. At the first stage, we can “wet” this film and try to discern the contours of the picture. This method corresponds to “colposcopy”. A solution of 5% vinegar is applied to the cervix, followed by Lugol's, which reveals areas of altered cells. Under a microscope we see how and to what extent the cells have changed, on the basis of which we can make the first assumption about the diagnosis. If we return to the example with the painting, then by the color scheme and the outline of the bears on the tree we assume what kind of painting it is. Obviously, the brighter the colors of the picture hidden behind the film, the easier it is to guess, and during colposcopy - the more pronounced the changes on the cervix - the more accurate the preliminary diagnosis will be. But this does not allow us to know exactly which picture is hidden.
At the next stage of solving the picture, we are asked to evaluate its many fragments, cut up like a puzzle. This corresponds to a method called “cytology”. There are two types of cytology: simple - in which the doctor uses a brush to remove cells from the cervix and its canal and smear it on a glass slide; liquid cytology: cells are collected with a special brush, which is immersed in a container with a solution. This container is sent to the laboratory where the cells are cleaned in a special apparatus and applied to the glass in one layer in an even circle to the size of the microscope eyepiece. That is, all cells are available for research and can be fully assessed, since they are located in one place in one layer. Unlike liquid cytology, a smear of cervical cells, smeared on glass by the doctor’s hand, has an uneven thickness, the material is blurred throughout the glass, so the ability to evaluate such a smear is significantly lower and therefore its diagnostic value is lower. Returning to the example with the puzzle - with ordinary cytology we are simply heaped with many different pieces, some of which are upside down, but with liquid cytology - all the puzzles lie side by side, face up and compactly collected in one place.
Based on cytology (if we are talking about liquid cytology), we can already guess the picture with a high probability, especially if it confirms the assumptions made during colposcopy. Simple cytology may not be informative enough. So far we have only talked about the norm.
However, having assembled the puzzle, we may suddenly discover, conditionally, fragments of a person’s face or an ax - which should not be in our picture. Based on this, we can make a diagnosis using cytology, but this can only be proven by doing a targeted biopsy or, by analogy, cutting out a small fragment of the picture that we are studying. To do this, under the control of colposcopy, a piece of the cervix is taken from places where staining has shown zones of changed cells, and not cells, as happens with cytology. That is, we will not have in our hands a set of puzzles, but a cut out small piece of canvas, but a very small one. It is no longer assessed by cytologists, but by pathologists. As a result of the study, they can either confirm the cytological diagnosis or refute it - by reducing or, conversely, increasing the severity of the changes. A small nuance - if the changes on liquid cytology and colposcopy are quite convincing, then the biopsy stage is often skipped and the changed part of the cervix is immediately removed and subjected to histological examination. This approach is also called “therapeutic-diagnostic”. When not a small piece is subjected to histological examination, as with a biopsy, but the entire removed fragment, a final diagnosis can be made, and most importantly, it can be assessed whether the entire affected area has been excised. If there are no atypical cells at the edges of the removed part of the cervix, then the affected area is completely removed; if atypical cells are detected at the edges of the removed fragment, then some of them remain in the cervix and there may be a relapse. Pay attention to this point, as it is extremely important within the framework of this article. In other words, we can claim that we have removed all diseased tissue based solely on the histological assessment of the resection margins and nothing else.
Now that you understand the methods for diagnosing cervical pathology, let’s move on to what changes we can identify with these methods.
There are several classifications of cervical pathology, which overlap because they were created at different times. For the purposes of this story, we will limit ourselves to the two most common ones. According to an earlier classification, the degree of cell changes under the influence of HPV is graded as CIN I, CIN II, CIN III, carcinoma in situ, cervical cancer. Here are the changes from minimal to cancer. Later another classification appeared:
- NILM is the norm; in fact, the name reflects the absence of atypical cells
- LSIL - mild dysplasia, it corresponds to the old classification CIN I
- HSIL - severe dysplasia: it corresponds to CIN II, CIN III and carcinoma in situ (translated as cancer in situ or pre-invasive cancer)
- ASCUS - this inscription appears in the conclusion when the cytologist sees cells in the smear that are different from normal, but cannot diagnose dysplasia, since there are not enough other signs. This is because cells can change their appearance not only because they are exposed to the virus, but also as a result of inflammation, injury or during the repair process.
- AGS - atypia of the columnar epithelium lining the cervical canal - is quite rare; curettage of the cervical canal is always indicated.
Liquid cytology describes changes using all classifications; pathologists (evaluating a biopsy) often resort to the old one, that is, they use the abbreviations CIN. The same (CIN - classification) is also used for colposcopic findings. In fact, both classifications describe the same changes, only in different degrees of detail.
Let's return to a viral infection, more precisely, for example, with the flu. The vast majority of the world's inhabitants become ill with this viral disease and recover from it on their own, with only a small percentage developing serious complications. As it was established relatively recently, changes in the cervix of the uterine cervix such as LSIL or CIN I or mild dysplasia, by the nature of the process, correspond precisely to a typical viral infection, which proceeds the same in most people and ends with recovery.
HSIL develops initially as a process moving towards the transformation of cells towards the oncological process, that is, the mechanism of this viral infection differs from that which occurs with LSIL. Essentially these are two different diseases.
It is currently questioned whether HSIL results from progression of LSIL. As studies have shown, the progression of LSIL to HSIL is observed only in 11% of cases, and the location of HSIL detection on the cervix differs from the place where LSIL was previously detected, which does not indicate progression, but an independent process.
It was also found that in the vast majority of cases, HSIL occurs against the background of long-term presence of two types of viruses, 16 and 18, in the body. It was noted that type 16 of the virus is divided into European and non-European, and it is the second type of HPV type 16 (non-European) that more often remains in the body and causes severe dysplasia.
It is impossible to answer the question: why in some women the immune system cannot cope with HPV and allows it to remain in the cells for a long time. However, it has been established that the violation of immunity in this case is quite specific, that is, there may be no general manifestations of decreased immunity; it is local immunity that is impaired. There is compelling evidence that smoking may significantly increase the risk of developing more severe dysplasia. One of the metabolites of nicotine, katanine , selectively accumulates in cervical epithelial cells and makes it easier for HPV to remain in the cells for a long time and transform them.
LSIL - regresses on its own in 90% of cases by the age of 30, and in 10% of cases it is a stage of formation of HSIL. This point must be understood very well in order to move on. Let's return to the example with the flu once again: an increase in temperature, nasal congestion and body aches will be observed in anyone with the flu in the first days of the disease, both in those who recover and in those who subsequently encounter complications. In the beginning it is impossible to distinguish. We just know that 90% will get better, and 10% will continue to get sick.
Based on this knowledge, a screening plan for cervical conditions in women has been proposed. It suggests that from 21 to 65 years of age, all women should have a cervical smear. from 21 to 30 years old - once every three years, after 30 years old once every 5 years if, according to an HPV test, the virus is absent. An HPV test is not taken as part of screening before the age of 30, since it does not matter, and after 30 years, this test only allows you to increase the period between tests.
If your smears come back normal (NILM), everything is fine, you can relax and do nothing, even if a persistent gynecologist took an HPV test from you and revealed its presence. Your immunity “works” with it and prevents your cells from changing.
But what to do if changes are detected?
If you are under 30 years old and have LSIL, how can you differentiate this simple manifestation of a viral infection from a step in the development of HSIL? For this purpose, a special marker is used - the p16ink protein, which can be detected in the same material that is assessed in liquid-based cytology. Without going into complicated details, I will explain that this protein appears in cells when they are in the process of further transformation into a more severe form of dysplasia. That is, if you have LSIL, this protein is detected in the analysis, the process will progress and this is no longer just a manifestation of a viral infection, but a stage on the way to HSIL.
In addition to the p16ink protein, when identifying LSIL, the viral load is assessed, that is, a test is performed based on the same material, a test that allows one to estimate the amount of virus present. If the viral load is high, this indirectly indicates the possibility of progression of the process, however, in the absence of the p16ink protein, only the presence of a high viral load only indirectly indicates the possibility of progression, and no measures are required, but will only reduce the interval between studies from 3 years to 1 year.
The picture changes a little after 30 years. Since we assume that the virus should be defeated in the vast majority of women by the age of 30, its presence after this age is suspicious. In this case, the cut-off age of 30 years, as always in medicine, is taken with large assumptions. For example, a woman could start sexual activity quite late, for example, at 26 years old, and by the age of 30, she simply had not yet had enough time for the virus to be suppressed or for LSIL to have not yet regressed. However, the doctor, that’s why he is a doctor, must keep all these nuances in mind when making a decision.
Apart from the particular cases described above, the attitude towards LSIL after 30 years is already more serious. The decision is made based on the totality of data from all studies: colposcopy, assessment of viral load, p16ink protein, cytology and biopsy data. In some cases, observation will be acceptable, but the interval will be once a year.
ASCUS - as I wrote above, this is a situation when a cytologist sees changed cells, but cannot decide why they have changed. In this case, an HPV test is prescribed and repeated testing is done in 2-3 months. If the changes were caused by HPV, then this will be confirmed by a positive analysis, and if the changes were reactive (in response to inflammation or healing), then they may no longer be present in the next analysis, of course, if the doctor identified the inflammation in the smear and cured it. Thus, if your analysis says ASСUS, there is no need to be afraid, with a high degree of probability everything will be fine in a repeat smear.
It's time to tell you how to treat HSIL. Despite the fact that this pathological condition of the cervix can regress on its own in 35% of cases, and progresses to cancer in only 12% of cases, treatment for HSIL is mandatory. The main goal of this treatment is the complete removal of altered areas of the cervix. To do this, a fragment of the cervix is excised using the radio wave method, laser, or scalpel. Without going into details: removal of a small fragment is called excision, removal of part of the cervix is called conization (since the removed fragment has the shape of a cone). It is also possible to carry out destructive methods, when the changed cells are destroyed by the same laser or cryo-influence.
The removed fragments are sent for histological examination to make a final diagnosis, which may differ from what was initially made for the better or worse, and this is extremely important. It is not uncommon for cytology and biopsy to diagnose HSIL, and the final histological report reveals LSIL, but there are also situations in the opposite direction, when initially mild dysplasia turns out to be severe.
No treatment for HPV with immunomodulators or other drugs is carried out, since HPV is not treatable. It is assumed that after removal of the altered tissue, the viral load is significantly reduced, which allows the immune system to suppress the remaining amount of the virus.
Now let's move directly to PDT. When performing PDT for cervical dysplasia, the cervix and cervical canal are irradiated in order to destroy altered cells, which, as noted above, take longer to remove the photosensitizing substance than healthy cells. The light beam can penetrate to a fairly shallow depth of up to 5 mm and it is impossible to reliably control this process. That is, treatment with this method is carried out virtually blindly, since there is no way to make sure that all the changed tissues have been affected. In addition, there is no histological conclusion about what degree of dysplasia actually was. Let me remind you once again that the data of a histological examination of a removed fragment of the cervix may differ from the data of cytology and even biopsy.
That is why none of the reputable organizations that control medical activities recommend this method for the treatment of severe cervical dysplasia, not to mention cervical cancer. Let me clarify this point once again: treatment of any precancerous or oncological disease requires verification that all altered tissues have been removed during treatment. For this purpose, a histological examination of the removed material is always carried out to make a final diagnosis and assess the resection margins. PDT specialists, provided that they cannot confirm the effectiveness of their treatment in this way, focus on control cytological studies of the cervix after treatment. It's not the same thing. A positive effect in the coming months after PDT does not exclude recurrence of the disease after a longer period of time due to some of the cells that did not die during therapy.
The vast majority of studies published in the world medical literature on the use of FTD for the treatment of cervical dysplasia do not allow evaluating this method from the point of view of clinical evidence-based medicine. The studies include no more than 30-50 patients - this is extremely small for full statistics; the study designs suffer from serious errors. The vast majority of articles were published by Chinese and Korean doctors. There is not a single publication devoted to PDT in the treatment of the cervix from the largest European and American scientific centers.
Some articles describe isolated cases of the use of FTD for cervical cancer and cancer in situ in patients with serious contraindications for traditional surgical treatment.
The most common argument of the ideologists of the use of PDT for the treatment of cervical dysplasia is that PDT, unlike conization, does not shorten the cervix, and thereby does not increase the incidence of premature birth and other complications during pregnancy. In fact, numerous retrospective studies show that patients who undergo conization have an increased risk of preterm birth. According to recent publications, authors are increasingly coming to the conclusion that everything is not so simple. First, the incidence of complications during pregnancy after conization is highly dependent on the size of the removed cone. Secondly, the authors point out that the causes of preterm birth are not fully understood and many retrospective studies did not take into account many associated factors that could affect pregnancy outcome. It is important that these studies assessed the pregnancy outcomes of tens of thousands of women, and pregnancies after FTD (according to published studies) number no more than a couple thousand worldwide. Accordingly, there are no comparative studies showing the superiority of FTD over conization in relation to pregnancy outcomes.
What do PDT specialists do in our country? Based on an analysis of the medical histories of my patients and direct observation of such specialists, I tell you.
- They firmly believe that the mere presence of oncogenic types of HPV in the body is dangerous, and HPV must be treated, and PDT actively treats HPV, and even builds immunity to HPV. This fact is refuted by several studies that can be found on pubmed, which show that some patients after FTD became infected with new types of HPV after 6 months.
- Who should be treated? Since HSIL is detected extremely rarely when using liquid cytology (0.7% of all studies performed in one of the largest Moscow laboratories - I previously published these data), they begin to treat LSIL, which, as I described above, should not be done (after except in cases of p16ink protein expression). LSIL is presented as an inevitable step on the path to cancer (you already know that this is not the case) and treatment is carried out based on this.
- Quality of diagnosis. In this article, I described clear tactics for making a diagnosis based on colposcopy, liquid-based cytology and additional markers, as well as cervical biopsy. However, such a complex and high-quality diagnostic protocol is not always followed. I have repeatedly seen cytological reports performed in conventional laboratories of hospitals or antenatal clinics, where it was simply written “the picture is consistent with HSIL” or “severe dysplasia” without describing the detailed cytological picture. In the overwhelming majority of cases, these diagnoses were not confirmed and, according to high-quality liquid-based cytology, a normal cytological picture was revealed. The same situation arises when reviewing the histological findings of a cervical biopsy; in some cases, the diagnosis is removed completely or the degree of dysplasia is reduced.
- As a result of conization, the doctor receives a histological conclusion about what he actually removed, and the pathologist also describes whether the affected tissue was completely removed. That is, control is obtained not only over the quality of treatment, but also over the correctness of the indications. When performing PDT, there is no control, that is, what was actually treated is not known.
In conclusion, I will once again remind you on the basis of which you can agree to treatment of the cervix.
Indications:
- HSIL or LSIL with the presence of p16ink protein expression and a high viral load - at any age.
- LSIL with the presence of high oncogenic risk HPV after 30 years (destructive methods)
How is the diagnosis made?:
— liquid cytology + p16 ink protein for LSIL
— colposcopy (the elements that matter are: mosaic, punctuation, atypical vessels)
- targeted biopsy
Treatment
- excision
- conization
- laser vaporization
Remember, if there are any doubts about the diagnosis, especially if severe dysplasia (HSIL) is diagnosed in cytology and/or biopsy, retake the test in another laboratory or take away slides/blocks with the material and have them reviewed in the laboratory of those medical institutions where they treat cancer diseases.
Photodynamic therapy: preparation and rehabilitation
Carrying out an intervention using photodynamic therapy does not require special preparatory procedures. The doctor conducts a gynecological examination of the patient, takes smears for flora and the presence of chronic inflammation, and then sets a day for surgery. Usually the date is chosen on days 8-12 of the menstrual cycle.
The operation is performed in a gynecological chair. The PDT procedure does not require the patient to be admitted to a hospital, and within 10 minutes after the end of the intervention the woman can go home.
Recovery after such treatment for dysplasia is quite rapid and is not accompanied by pain. The only thing women note is the presence of watery discharge with slight traces of blood in the first days.
Advantages of conducting FTD
FTD is a painless method of treating gynecological diseases of the cervix, which uses a laser. It, in turn, does not contribute to severe damage to the treated surface, which leads to a reduction in the rehabilitation period. For the same reason, the likelihood of bleeding is also minimal, which cannot be said about the surgical method. When using it, various piercing surgical instruments are used, which often lead to damage to blood vessels, which can cause complications and a long period of wound healing. In addition, the use of laser equipment helps prevent the appearance of scars and cicatricial changes on the tissues of the cervix, which also has a beneficial effect on its condition. FTD has no side effects. Individual intolerance to drugs is observed in isolated cases. And if an allergic reaction to medications does occur, it can be easily relieved by taking antihistamines. Only a few treatments are required for complete recovery. After just a few sessions, the affected areas begin to recover, and after a few months there is no trace left of cervical pathologies.
Popularity among women under 40
Although the use of laser therapy is not as reliable and effective as surgery, it has gained great popularity among women under 40 years of age for the treatment of the cervix. And all because it eliminates the occurrence of any complications affecting the functioning of the reproductive system. All this makes FTD popular not only in our country, but also abroad. Its use has helped to reduce the number of cancer patients. Evidence of this is provided by numerous reviews from patients who have tried this treatment method on themselves and were satisfied with the result. FTD allows you to get rid of gynecological diseases of the cervix and preserve the opportunity in the future to feel what it is like to become a mother!
98
Results of treatment of the cervix using photodynamic therapy
To control the disease, the patient should consult a doctor one month after treatment with photodynamic therapy. If you strictly follow the instructions and recommendations of doctors, PDT gives excellent results and significantly reduces the risk of relapse.
Recovery after photodynamic therapy of the cervix
For a quick recovery, a woman must prepare for the procedure in advance and follow all the doctor’s recommendations. Contact with artificial and sunlight should be avoided in advance and minimal contact with sources should be ensured after the operation. If everything is done correctly, within a month the patient can return to her usual rhythm of life.
Reviews of photodynamic therapy of the cervix
Most women speak positively about photodynamic therapy as a method of treating cervical dysplasia. Here are real examples from people's lives:
A great way to get rid of gynecological problems. With the help of PDT, I forgot about what erosion is once and for all, and became a mother. I recommend!
Last year I was diagnosed with cervical dysplasia and the presence of human papillomavirus. Having turned to a worthy doctor, who prescribed me treatment using photodynamic therapy, I got rid of the disease. I hope there won't be a relapse. This method of treatment is absolutely painless and effective. Checked personally.
Photodynamic therapy has successfully established itself as an effective method in the fight against diseases of the female organs. Timely consultation with a doctor and correctly prescribed treatment is a guarantee of success in the fight against cervical pathology. Be healthy!
What is dysplasia
Dysplasia is a pathological condition in the structure of the cells that make up the mucous layer of the cervix. The process of degeneration of healthy cells into atypical ones occurs gradually - first hyperplasia develops, then proliferation, and then cell differentiation is disrupted, which leads to a change in the number of epithelial layers.
Normally, the mucous layer of the cervix consists of three layers:
- basal;
- intermediate;
- superficial.
The formation of new cells occurs in the lowest (basal) layer. The cells that form there are round in shape and have one nucleus.
As the cell matures, it moves towards the surface layer, flattening slightly, while the nucleus becomes somewhat smaller. Thus, the superficial layer of the mucosa consists of flat epithelial cells, while the basal layer consists of round ones. This is how the mucous membrane is divided into layers.
In dysplasia, the basal cells do not flatten and the size of their nucleus does not change, resulting in the presence of identical cells in all three layers. In addition, some cells contain more than one nucleus, which leads to disruption of their functionality and the structure of the mucous membrane of the neck as a whole.
The cause of the pathological process in most cases is the human papillomavirus of highly oncogenic strains (16, 18).
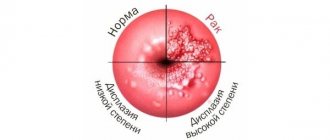
Dysplasia can have three degrees, which depend on the prevalence of the process - it looks like this:
- mild degree - the lesion covers a third of the basal layer of the mucosa;
- moderate degree – 70% of the mucous membrane is affected;
- severe stage - the last stage, which is also called non-invasive cancer. This form of cancer differs from invasive cancer in that the pathological malignant process does not involve muscle tissue, nerves and blood vessels.
IMPORTANT!
The earlier dysplasia is diagnosed, the higher the likelihood of complete relief from the disease.