To maintain health, a woman is recommended to carry out timely preventive diagnosis and treatment of gynecological diseases with regular visits to the gynecologist. In the absence of complaints and chronic pathologies, a preventive visit to the doctor is recommended annually.
A gynecological examination is the basis for determining the normal microflora of the vagina and the cellular composition of the cervix.
One of the standard gynecological procedures is the examination of the contents of the vagina and urethra for flora and oncocytology. Smears are taken from each woman.
A smear for oncocytology and flora is carried out annually in the absence of pathology, and an additional smear for flora in women with complaints from the reproductive organs.
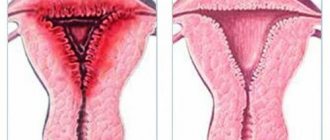
Leukocyte infiltration of the cervix
The diagnosis of leukocyte infiltration frightens women.
Ignorance about the disease terrifies any person, especially if it concerns the reproductive system or cardiac activity. Therefore, doctors often hear the question: “Leukocyte infiltration: what is it?” You should consider the issue from all sides to understand what kind of condition it is. This condition means that there are too many white blood cells in the epithelial cells, according to the norm. These cells appear white and their role is to protect the body from infections. That is, leukocytes are cells of the human immune system.
They are also responsible for:
- immunity in general;
- absorption of foreign agents;
- combating particles that carry allergens;
- detection of foreign agents in the blood.
According to this information, it becomes clear that leukocyte infiltration of the cervix is a condition that develops in the presence of an inflammatory process in the tissues. Most often occurs with cervicitis and vaginitis.
Cytology smear: interpretation
Oncocytology involves microscopic analysis (study of the cellular composition and state of cell organelles) of material suspicious of an oncological process and taken from any accessible place.
In this regard, patients should not be surprised by smears for oncocytology, prepared not only from scrapings of the female genital organs, but also fine-needle aspiration biopsy (FNA):
- Enlarged regional lymph nodes (cancer of the larynx, nasal cavities and paranasal sinuses, salivary glands, penile cancer, eye tumors, etc.);
- Tumors of the pancreas, liver, gallbladder and extrahepatic bile ducts;
- Seals and nodes of the mammary and thyroid glands.
Analysis
The diagnosis of leukocyte infiltration is made to women who have had a smear taken during a gynecological examination. The resulting material is sent to the laboratory for examination under a microscope. A smear is obtained using a Volkmann spoon after inserting a speculum into the vagina.
Where does the research material come from? The doctor takes tissue from the places where he sees pathological changes. The resulting material is applied to a glass slide and dried, only then the smear is checked in the laboratory.
Preparation
If a woman visits a gynecologist according to her schedule, she should know that before coming to the doctor she should prepare for tests. Twice a year, the doctor examines the vagina and cervix to rule out various diseases.
The day before visiting the doctor, you should not douche, use vaginal suppositories or local contraceptives. You should also avoid sexual contact for 2-3 days before taking the test.
A smear is taken from women who have toileted the external genitalia. In this case, you cannot use hygiene products and you must wear clean underwear. If you are taking any medications, be sure to tell your doctor.
Decoding
Leukocyte infiltration means an increased number of white blood cells. In this case, you should immediately sound the alarm. After all, this condition means an inflammatory process of the cervix, the cause of which should be established and eliminated.
The norm of leukocytes in the cervix is no more than 15. If it is exceeded, it means the woman has an inflammatory disease. The greater the deviation from the norm, the more serious the inflammatory process in the cervix and the sooner it is necessary to start treatment.
After receiving the tests, the result is difficult to decipher on your own. Only a doctor can do this. But women get worried and start looking for answers in other sources. The table below shows two examples of leukocyte infiltration. These examples are the results of real tests, and from them you can learn about the cause of the disease.
Gynecological smear
The first thing to pay attention to is the number of leukocytes in a gynecological smear. These white blood cells provide antibacterial and antiviral protection. They also fight any antigenic structures that cause the inflammatory process.
Leukocytes migrate in large numbers to the microbial focus and concentrate around it. They tend to increase in size and break down over time. These processes cause signs of local inflammation:
- Swelling of the affected area.
- Hyperemic reaction, localized rash.
- The temperature in the pathological focus increases.
Upon examination, the gynecologist discovers hyperemic and pasty mucosa of the external genital organs. Women may complain of itching and burning in areas of inflammation.
Every representative of the fair sex should see a gynecologist at least once every six months, unless she has an obstetric-gynecological pathology. If you become infected with a bacterial or viral infection, it is advisable to identify the microbe and receive etiotropic treatment from a doctor. A smear is also taken during routine examinations of pregnant women, during preconception preparation, and in the postpartum period. Courses of broad-spectrum antibiotics can change the microflora of the genital organs, which is also detected when taking a smear.
Symptoms
Different diseases may have different symptoms. A more detailed clinical picture will allow the doctor to reduce the number of examinations, this will save the patient’s time and money, and will also bring him closer to identifying the cause.
We will consider the symptoms of inflammatory diseases of the cervix in the presence of leukocyte infiltration below.
Polyps
If the polyp is mechanically damaged, bloody discharge from the vagina appears during or after sexual intercourse, as well as before or after menstruation. With large formations on the cervix, pain appears in the lower abdomen and lower back.
There is a disturbance in the menstrual cycle due to increased levels of estrogen. The cycle is shortened, the duration of critical days increases. With heavy bleeding there is a risk of developing anemia. Chronic fatigue, drowsiness and weakness sets in. A woman may periodically lose consciousness. The main complication is infertility.
Treatment
Therapy for leukocyte infiltration depends on the cause of its occurrence. To correctly draw up a treatment regimen, you will need to undergo urine and blood tests, do an ultrasound examination of the pelvic organs and PCR for hidden sexually transmitted infections, and also carry out bacterial culture and colposcopy.
Only a comprehensive examination will allow us to detect the cause of leukocyte infiltration and cure the changes occurring in the cervix. An increased number of leukocytes is treated with antiseptic and antibiotic drugs, as well as with lacto- and bifidobacteria.
Treatment of leukocyte infiltration also depends on the cause itself. Having gotten rid of the disease, the level of leukocytes in the epithelium of the cervix will be restored. It is possible to be sexually active in this condition if additional tests do not reveal a specific infection.
Cytology results
Good day! Please help me decipher the cytology results. After 3 weeks, stimulation followed by incision is planned. All the tests are excellent and the last one came back like this:
Cytological examination of biomaterial from the cervix using the Papanicolaou method (PAP test)
1. Quality of the drug:
Exocervix - the quality of the drug is adequate.
Endocervix - the quality of the drug is adequate.
2. Cytogram (description).
Exocervix - the resulting material contained cells of superficial and intermediate squamous epithelium
Weak, sometimes moderately pronounced leukocyte infiltration.
Endocervix - elements of peripheral blood and squamous epithelial cells were found in the obtained material
superficial, intermediate layers and columnar epithelium.
Squamous metaplastic epithelium.
Moderate, sometimes pronounced leukocyte infiltration.
3. Additional clarifications.
In the obtained material, cells with signs of malignancy were not identified.
What is leukocyte infiltration of the cervix
To maintain health, a woman is recommended to carry out timely preventive diagnosis and treatment of gynecological diseases with regular visits to the gynecologist. In the absence of complaints and chronic pathologies, a preventive visit to the doctor is recommended annually.
A gynecological examination is the basis for determining the normal microflora of the vagina and the cellular composition of the cervix.
One of the standard gynecological procedures is the examination of the contents of the vagina and urethra for flora and oncocytology. Smears are taken from each woman.
Indications for taking a smear
If a woman has no complaints, the indications for analysis include:
- annual preventive examination;
- registration for pregnancy;
- 18, 30, 36, 40 weeks of gestational age;
- cervical erosion;
- ectopia of the cervix;
- ectropion of the cervix;
- cervical dysplasia;
- cervical stump after surgery.
If there are complaints, a smear is taken for examination when:
- changes in the color or consistency of vaginal discharge;
- the appearance of an unpleasant odor of discharge;
- violation of the act of urination in the form of discomfort, pain;
- itching in the genital area;
- burning sensation;
- painful sensations in the lower abdomen;
- discomfort or pain during sexual intercourse;
- changes in the nature of discharge or discomfort while taking medications.
Normally, if a woman has complaints, a smear for flora is taken at the first visit to the antenatal clinic. During pregnancy, vaginal examinations and smears are performed more frequently if indicated.
Leukocytes and the cervix
Leukocytes are considered one of the main components of the human body, belonging to the white line of blood. The main function of white blood cells is to protect against harmful pathogens entering the body from the outside.
The protective function of leukocytes is:
- specific – from certain pathogens;
- nonspecific or general.
When inflammatory reagents enter the body, an inflammatory response develops, which is normally characterized by an increase in the concentration of leukocytes.
Leukocytes digest foreign agents. Normally, with a high concentration of pathogens, leukocytes begin to destroy, which is accompanied by an inflammatory reaction with the development of characteristic changes in the form of:
- hyperemia, or redness;
- swelling;
- local temperature rise.
A flora smear is a microscopic examination of scrapings from the urethra, cervix and vagina using bacterioscopy. To carry out the analysis, a disposable spatula with a rounded end is used.
The slide has 3 stroke designations:
- U – from the urethra;
- V – from the vagina;
- C – from the cervix or cervix.
In the laboratory, the dried smear is examined under a microscope, after which a conclusion is given about the composition of the microflora. The conclusion has visibility symbols:
- L – number of leukocytes;
- Ep – amount of squamous epithelium;
- Gn – the presence or absence of gonococci, the causative agents of gonorrhea, in the smear;
- Trich - the presence or absence of trichomonas in the smear, which are the causative agents of trichomoniasis.
Cytological examination in gynecology
Cytological analysis in gynecology refers to microscopic examination of samples taken from the vagina and cervical canal to determine the typical cellular composition. This diagnosis allows doctors to draw conclusions about the presence of inflammatory processes, precancerous diseases or cancer in the patient’s reproductive organs.
Unlike histological examination, the cytological method is non-invasive. That is, when taking biological material there is no need to perform a biopsy or puncture, and the integrity of the tissue is not compromised at all. Samples taken using a fingerprint or swab are analyzed. To obtain accurate results, you must carefully follow the rules for preparing for the examination. It is also very important that the analysis is deciphered by the woman’s attending physician, who will take into account her complaints and data from other diagnostic methods.
Cytological analysis usually takes no more than a day to complete. If a precancerous condition or an oncological process is discovered, invasive diagnostic techniques are used to clarify the diagnosis - biopsy.
Cytology is especially important when biopsy is contraindicated and when examining a large number of patients (when it is necessary to identify women at risk for developing malignant pathology).
A smear cytology (Pap test, Papanicolaou test) is a microscopic examination of a smear from the cervix for the purpose of early detection of cancer. This analysis is also called a hytological smear or oncocytology smear. This examination is easily tolerated by patients because it is completely painless and does not take much time.
A cytological smear not only makes it possible to timely diagnose cellular abnormalities, but also helps to identify the presence of unwanted microflora in the vaginal environment. At the same time, the test does not provide accurate data on the detected pathologies, and if an unfavorable result is obtained, the patient is sent for additional examination (smear for flora in women) and for testing for STDs.
Using the cytological method, which has been successfully used in gynecological practice for decades, it is possible to identify 5 types of changes in the cells of patients. Moreover, the research is very simple and affordable. Doctors advise all women aged 18 to 65 to undergo it at least once a year. Based on the results of the analysis, it is possible to reliably establish the presence or absence of any pathology.
Preparation and execution
To obtain a reliable result of a smear examination, it is necessary to properly prepare for a visit to the gynecologist. No special preparation required. However, simple rules should be followed.
- Avoid sexual intercourse for 48 hours before the smear test.
- Do not use lubricant gels, vaginal suppositories or creams 24 hours before the test.
- It is forbidden to douche 24 hours before seeing a doctor.
- On the day of the smear test, do not use any intimate hygiene products when washing your genitals.
- After the last day of taking antibacterial drugs, 10 to 14 days should pass.
- It is not recommended to do the test during menstruation. Particular attention is paid to heavy bleeding.
- The last act of urination before visiting a gynecologist should be performed 2 hours before the appointment.
Sexual activity, topical products, and douching can distort the reliability of the result due to changes in the microbiocenosis.
If there is bloody discharge, there will be red blood cells in the field of view of the microscope. With heavy discharge, other elements and pathogenic microorganisms may not be detected.
During the act of urination, urine can wash away cellular elements and microorganisms.
The research is carried out as follows.
- A woman is on a gynecological chair.
- The doctor inserts speculum into the vagina and exposes the cervix.
- A smear is taken from the cervix, urethra, and vagina for flora.
- A thin layer of material is applied to a glass slide under the designations: C, V, U.
- The material is sent to the laboratory, where it is stained with special dyes and examined under a microscope.
How many days does a smear cytology test take?
Cytological analysis of a smear usually takes from 1 to 5 days.
It is important to remember that the oncological process does not occur in a few days. Quite a long time passes from the first pathological changes to malignant degeneration. Therefore, timely detection of atypical cells in a woman’s body makes it possible to prevent the development of cervical cancer. For these purposes, an accessible and simple method for the early diagnosis of malignant cells was introduced everywhere - a cytological examination of a smear.
A smear is taken during a gynecological examination using a cytobrush, and then the material is placed on glass (for liquid oncocytology, a removable cytobrush is used, which, together with the material, is immersed in a bottle with a special medium).
Oncocytology of the cervix, as a rule, is not limited to one smear (vaginal portion of the cervix), since there is a need to study the epithelium of the cervical (cervical) canal. This is because the most problematic area in relation to the oncological process is the junction zone (transformation zone) - the place of transition of the multilayered squamous epithelium of the vaginal part of the cervix (ectocervix) into the single-layer prismatic (cylindrical) epithelium of the cervical canal (endocervix).
Of course, it is unacceptable to “slap” both smears on one glass during diagnosis (this is only possible during a medical examination), because they can get mixed up and the smear will turn out to be inadequate.
In a smear from the cervix of a young healthy woman, you can see cells of the superficial and intermediate layer (in various proportions) of non-keratinizing four-layer squamous epithelium growing from the basal cell, which is normally located deep and does not enter the smear, as well as cells of the prismatic epithelium of the cervical canal.
The PAP test is a fast, inexpensive, informative method for diagnosing diseases of the vagina and cervix.
The main task of cervical smear cytology is: - identification of atypical cells; - diagnosis of precancerous changes (dysplasia) and cervical cancer (CC).
Cervical screening (mass examination of cervical smears) is a method of secondary prevention of cervical cancer.
Primary prevention of cervical cancer is vaccination against the human papillomavirus HPV.
Read more about the symptoms of human papillomavirus infection in women and the treatment of HPV here: Condylomas acuminata.
The main task of cytological analysis of cervical smears is to identify atypical cells.
Atypical cells are morphologically altered cells: precancerous, cancerous.
- In malignant atypical cells, oncogenic mutations affect both the nucleus and the cytoplasm.
Cytological signs of malignant atypia: - increase in nuclear size; - change in the shape and color of the kernel; - abnormalities in the cytoplasm of cells.
The severity of atypia can suggest the level of precancerous changes (degree of dysplasia) of the cervix. But! Cytology does not determine the depth of tissue damage and does not distinguish dysplasia from non-invasive cancer (carcinoma in situ) or invasive microcarcinoma. Histology solves these problems.
White blood cell counts are normal
Normal leukocyte counts depend on the location of the material taken and are determined in the field of view of the microscope.
- Vagina or V. Leukocytes – 0 – 15, epithelial cells – 5 – 10, mucus – moderate. Gram-positive flora in the form of bifidobacteria and lactobacilli can be detected.
- Cervix or C. Leukocytes – 0 – 30, epithelial cells – 5 – 10, mucus in moderate quantities.
- Urethra or U. Leukocytes – 0 – 5.
Normally, the number of leukocytes does not exceed 15 per field of view. When their number increases, one can judge the nature of the inflammation: the higher the concentration of leukocytes is determined, the more pronounced the inflammatory reaction.
Squamous epithelium is the superficial layer of cells that is found at the entrance to the cervix and lines the vagina. Normally, it is always determined during childbearing age. As estrogen levels decrease, their quantity decreases.
Mucus is detected in material from the vagina. If it is found in material from the urethra, diseases of the genitourinary system should be differentiated.
Doderlein rods are lactic acid bacteria that create the normal acidic flora in the vagina. If there are enough of them, they speak of normal microflora.
Normally, the smear does not contain pathogenic microflora in the form of gonococci, trichomonas, chlamydia, gardnerella, yeast, and cocci.
During pregnancy and depending on the phase of the cycle
The number of leukocytes in a smear varies depending on the phase of the menstrual cycle and during gestation, which is due to hormonal fluctuations.
Normally, the number of leukocytes is higher in the cervical canal compared to the vagina.
The concentration of leukocytes increases in the middle of the menstrual cycle and increases before the onset of menstruation. To correctly interpret the result obtained, it is necessary to compare the ratio of leukocytes to squamous epithelium. Normally, there are 10 polymorphonuclear leukocytes per 1 cell of squamous epithelium.
In the case of high white blood cell values during gestation, this may indicate a risk of gestational complications in the form of:
- IUI or intrauterine infection of the fetus;
- premature birth;
- spontaneous miscarriage;
- weakness of labor.
Reasons for the increase
Among the main reasons that lead to an increase in leukocytes in a smear are:
- colpitis or inflammatory lesion of the vagina;
- cervicitis or inflammatory disease in the cervix;
- endometritis or damage to the endometrium of the uterus;
- salpingoophoritis or inflammation of the uterine appendages;
- urethritis or inflammation of the urethra;
- malignant processes of the reproductive organs;
- STI;
- bacterial vaginosis;
- hormonal imbalance;
- immune disorders;
- severe stressful situations;
- frequent douching;
- anatomical features of the vulva;
- intestinal dysbiosis.
Etiology of leukocytosis
Elevated white blood cells can be detected in the cervical canal due to failures of the reproductive sphere and failure of any other organ of the female body. High white blood cell counts are most often found when:
- Active inflammation of the cervical canal – cervicitis. The process may be limited to only a given area, or it may be widespread. Thus, the internal genital organs as a whole can be inflamed: tubes and ovaries, uterine lining, vagina.
- A clinical picture somewhat similar to inflammation can be observed by a doctor during a tumor process of the urinary tract and genital organs. Leukocyte infiltration often occurs here, as these cells seek to neutralize agents with an abnormal antigenic structure. In addition, the destruction of healthy tissue by a tumor also gives inflammatory symptoms, which form the causes of an increase in leukocytes in the cervical canal.
- Deviations from the norm of leukocytes directly in the cervical canal also occur in conditions such as intestinal or vaginal dysbiosis. An increased number of white blood cells forms an infiltrate that suppresses the action of opportunistic microorganisms.
- Hidden sexually transmitted infections, as well as sexually transmitted diseases with pronounced symptoms, directly mediate an increase in leukocytes in the cervix.
Various modifications of microorganisms currently make their detection a complex and time-consuming process. A smear from the cervix or other anatomical area is not always indicative.
Elevated white blood cells are found in women outside the bacterial flora, which requires more accurate methods of recognizing microbes. In such cases, the improved polymerase chain reaction comes to the rescue, the complex mechanism of which makes it possible to detect in smears most of the pathogenic bacteria that cause inflammation of the cervix. These include mycoplasmas, gonococci, treponemas, trichomonas, amoebas, herpes virus, cytomegalovirus and many other microorganisms.
How to detect the condition?
You can find out about the pathology after the results of a vaginal smear or from the cervix. It is taken using a Volkmann spoon.
A gynecologist examines a woman in a gynecological chair and inserts special speculums. It is at this moment that the material is collected. Afterwards, the results are sent to the laboratory, where they will determine whether there is a pathology.
To clarify the diagnosis, the doctor has the right to give a referral for liquid cytology. This type of research is more informative. In this case, the material is collected with a special brush, which the doctor rotates in the cervix. Thus, it is impossible to miss the disease.
Preparing for the study
Before the test, a woman needs to thoroughly wash her external genitalia and dress in clean clothes. There is no need to take any special events.
For personal hygiene purposes, you should not use scented soaps or intimate deodorants.
You cannot douche, use vaginal suppositories, tablets, ointments, creams or insert tampons the day before. It is advisable to refuse sex two days before taking a smear. The procedure is not carried out during critical days. The woman should be warned several days before the procedure.
Methodology
The results of a smear give a reliable result when the testing technique was correct. The material is collected during examination in a gynecological chair using a mirror. First, the doctor conducts an examination, after which:
- Removes all secretions from the mucous membrane.
- Armed with a Volkmann spoon, the doctor takes a scraping. Typically, a cytological smear is taken from 3 areas (vaginal vault, in the area of the vaginal exocervix and the cervical canal).
- Afterwards, the material is placed on a piece of glass, which the laboratory assistants have previously disinfected and degreased. All three samples can be applied to one glass. To prevent the material from drying out, it is covered with ethyl alcohol. If there is a special aerosol, then use it.
- Then take a brush (endobash). It can be replaced by a stick with a tampon, which has been pre-treated with sodium chloride. A smear is taken from the desired area and is painless.
- After the manipulations, the collected materials are transferred to the laboratory. Using a microscope, specialists examine smears and determine the pathologies present.
If you need to take liquid cytology, then the material that the doctor collected is mixed with a special solution and applied to a piece of glass. This is followed by the distribution of leukocytes and mucus.
Bloody discharge may be present after cytological smears. This is not a deviation. They go away in 4-6 days and do not have an unpleasant odor. If any deviations from the norm appear, this is a clear reason to contact a specialist.
What can the research show?
Tests make it possible to determine the presence or absence of infections; after seeing the results, the doctor can evaluate the woman’s hormonal background and the condition of the vagina. If a woman is carrying a baby, according to the data, miscarriage can be prevented.
When laboratory workers examine smears, they will definitely pay attention to white blood cell counts. Leukocytes protect the body from pathological microorganisms. If there are a lot of them, then there is an active inflammatory process. The more there are, the more severe the stage of the disease.
In the case of 25-30 leukocytes in the cervical canal, about 5 in the urethra, in the vagina - 8-10 - this is the norm. These indicators are present in all women who have regular sexual intercourse.
If the indicators are much higher than those indicated above, then there is a pathology. Only a doctor can determine the main reason for the strong increase in white blood cells. An accurate diagnosis is established after bacterial culture, PCR (polymerase chain reaction) and immunological analysis.
Less common causes
White blood cells in the cervical canal differ from the normal value for some other less common reasons. Thus, dysbiosis of the genital organs described above may be a consequence of general somatic and autoimmune pathologies:
- Leukocyte infiltration of the cervical canal or cervicitis occurs during hormonal imbalances in girls during puberty, as well as during the decline of reproductive reproduction or menopause. Endocrine imbalance mediates pregnancy, as well as its spontaneous or forced termination. Increased or decreased production of hormones by some organs becomes an impetus for an increase in leukocytes in the cervical canal against the background of activation of the opportunistic microflora of the endocervix.
- Elevated white blood cells are found in women in a smear from the cervix after a sharp drop in general immunity. The reason for this may be hypothermia, taking broad-spectrum antibiotics.
- Exposure to chronic stress causes significant damage to a woman's health. It can also be reflected by leukocyte infiltration of the endocervix, a general imbalance of the vaginal microflora. Overwork and heavy physical labor may also be accompanied by this symptom.
- Elevated leukocytes in smears from the cervix can also occur after intense sexual intercourse. Hard copulation causes microtrauma and cracks in the vagina, to which white blood cells quickly react.
- If a woman often changes sexual partners, this can also affect the cellular composition in the cervical canal. A large number of leukocytes neutralizes the constant change of bacterial flora.
- Leukocyte infiltration in the endocervix can be a side effect of chemotherapy or radiation treatment.
- Excessive enthusiasm for hygiene rules, as well as their complete absence, harms the microflora of the genital organs. The use of douching changes the cellular composition of the internal environment, sometimes not for the better, causing inflammation and migration of leukocytes. Neglect of basic hygiene procedures causes the proliferation of opportunistic microorganisms, which white blood cells also seek to neutralize.
- Some barrier concentration agents cause leukocytosis in the cervix. Various spermicides in the pharmacological forms of suppositories or ointments disrupt the existing balance of the sexual environment. Inflammation and leukocytosis in the genitals also occur as allergic reactions to male sperm.
- The anatomical structure of the genital organs can be changed by congenital deformities, during pathological childbirth, or surgical interventions. This leads to shifts in the cellular environment in the cervical canal and adjacent areas, where white blood cells tend to increase.
- Foreign bodies also lead to cellular-bacterial imbalance of the genital organs. The norm of leukocytes in the cervical canal is never observed in women who use hygienic tampons.
- Temperature changes, prolonged hypothermia or overheating of the female body harm the cellular composition of the endocervix. An imbalance is also caused by tight underwear, panties made of synthetic fabric and thongs.
Conclusion
Leukocyte infiltration of the cervix is detected after receiving the smear results. What this is is already clear from the above information, and the doctor will tell you how to treat the pathology after the diagnosis has been established. The essence of treatment will depend on the severity of the disease and the pathology itself. Self-medication is unacceptable, as it can lead to serious and irreversible consequences.
Sources:
https://uterus2.ru/disease/lejkotsitarnaya-infiltratsiya-shejki-matki-chto-eto-takoe.html https://ginekola.ru/ginekologiya/shejka-matki/chto-takoe-lejkotsitarnaya-infiltratsiya-shejki-matki .html https://vashamatka.ru/zabolevaniya/lejkotsitarnaya-infiltratsiya-shejki-matki.html