Hysterectomy, or hysterectomy, is a gynecological operation in which the uterus is removed along with the cervix and appendages (ovaries and tubes).
- Indications
- How is hysterectomy performed?
- Extended hysterectomy
- What other types of operations are there?
- What types of operations are most often performed in oncology?
- Which method of hysterectomy is better?
- Possible complications
Operations to remove the uterus: types and indications
Removing the uterus is a very risky step for a woman, since such an intervention completely eliminates future childbearing. That is why to perform an operation there must be strict indications, which can be divided into absolute and relative.
Absolute indications for surgery are a malignant tumor of the female genital organs, uterine prolapse, incessant postpartum bleeding (this is an emergency indication). Absolute indications imply that it is impossible to cure the disease in any way other than surgery. Such operations are performed on women (sometimes teenage girls) regardless of age and number of children born, since this is the only way to save the patient’s health and life.
Relative indications are large or multiple fibroids that progress rapidly, endometriosis, adenometriosis, inflammatory diseases of the female genital organs, frequent and heavy menstrual bleeding. In all these cases, we talk about removal only when conservative treatment methods are ineffective. In some cases, removal of the uterus for the listed conditions is performed on postmenopausal women or those who already have two children (at the patient’s request), even if the woman’s condition is not so critical.
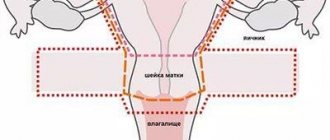
There are several main types of hysterectomy. The choice of a specific type remains with the doctor. The two main types are amputation (the neck of the tag remains in place) and extirpation (the uterus is removed along with the cervix and part of the vagina). Both of these types of operations may affect the appendages (fallopian tubes and ovaries), or may leave them intact.
Since during extirpation the cervix is completely removed, in the future we will only talk about amputation of the uterus. In terms of volume, this intervention can be of two types - subtotal and total amputation. The first type is the most sparing, while the vagina, cervix up to the internal os, fallopian tubes (sutured) and ovaries are preserved. In the second case, the uterus is completely removed along with its appendages, but the vagina and cervix remain in place.
According to the method of carrying out, uterine amputation can be hysteroscopic, laparoscopic and laparotomic. Hysteroscopic is the most gentle option, performed under local or subdural anesthesia. The instruments are inserted through the vagina, leaving no scars on the skin. Laparoscopy is a surgical procedure performed through a small puncture in the skin, if there is a need to perform a large volume. Transsection is used in severe cases, for example, postpartum hemorrhage.
In addition to indications, there are also contraindications to hysterectomy. These include the serious condition of a woman caused by decompensation of a chronic pathology - in this case, the operation is performed after stabilization of the patient’s condition. Acute infectious diseases are also a contraindication for intervention - they need to be cured before surgery. And the third absolute contraindication is cancer of any organ, including the uterus, stage 4.
What determines the cost of the operation?
Surgical intervention is prescribed when conservative treatment methods do not bring satisfactory results, or their use may cause harm to the patient. The price for the procedure to remove the affected organ depends on the following factors:
- On the volume of tissue removed.
- Depending on the type of procedure chosen.
- The number of days spent in the hospital after surgery.
What is a cervical stump?
A stump is the remnant of an organ left after its removal. In the case of the cervix, this is a fragment from the internal os (sutured during surgery) to the external os (vaginal part). The vagina remains completely intact. The stump of the cervix is a consequence of a previous operation - amputation of the uterus (with or without appendages).
The absence of a uterus and the presence of a stump in no way affects the appearance (especially if the operation was performed using the hysteroscopic method) or the woman’s quality of life. Patients who have undergone uterine amputation continue to live a full sexual life, experiencing no less vivid sensations. However, after removal of the uterus, reproductive ability is completely lost, so in young women who do not have children, doctors are extremely reluctant to prescribe this operation if there are no vital indications.
There is a widespread belief that the consequences of uterine amputation have a significant impact on the female body - for example, that a woman ages much faster or has an increased likelihood of other gynecological diseases. Here it should be clarified that the changes that occur depend on the volume of the operation.
If a woman has only her uterus removed, but the ovaries and fallopian tubes remain, then her hormonal levels after the operation remain normal, she looks healthy and feels good. Therefore, this type of intervention is preferable in young women.
If a total amputation of the uterus and appendages was performed, then in the absence of female sex hormones, menopause actually occurs earlier. If a woman is postmenopausal, then these changes do not affect her, but if before the operation she had a stable menstrual cycle, then the symptoms of premature menopause are eliminated with the help of hormonal therapy.
As for the likelihood of developing gynecological diseases, in particular breast cancer, in this case the connection is not with the operation itself, but with the reasons that caused the disease. In particular, the likelihood of breast cancer is higher in women who have been diagnosed with fibroids (if conservative therapy is ineffective, this disease is an indication for uterine amputation).
The most noticeable change in a woman’s lifestyle after surgery is the disappearance of menstruation. Many patients consider this feature to be rather positive, especially if during the illness they suffered from heavy and painful periods. However, if the intervention is performed incorrectly or in insufficient volume, and the factor causing the disease is not completely removed, complications in the late postoperative period are possible - prolapse and cancer of the cervical stump.
Preparation
Before cutting out this organ, a woman must undergo certain training, which will confirm that she has no contraindications for the intervention. The following diagnostic procedures are carried out:
- General and biochemical blood test;
- General clinical urine analysis;
- Coagulogram;
- Blood test for HIV, hepatitis, syphilis;
- Vaginal microflora smear;
- Ultrasound;
- ECG;
- Consultations with a therapist and gynecologist.
Of course, in some cases such studies are neglected, for example, when intervention is urgently needed. But if the operation is carried out as planned, then such preparation is necessary.
Postoperative period and its complications
Adaptation to the cervical stump begins immediately after the manipulation. Rehabilitation is divided into early (in hospital) and late. Early rehabilitation can last from a day to 12 days, depending on what type of surgery was performed on the patient (abdominal, laparoscopic, hysteroscopic). Late rehabilitation includes a long period after discharge from the hospital.
At an early stage, the patient needs medical supervision to prevent bleeding and complications from internal organs. Therefore, a woman needs to be attentive to her condition and promptly inform the doctor that she has a stomach ache or experiences any other unpleasant sensations.
In the early postoperative period, bleeding and inflammation in the area of the sutures are possible, affecting both the cervix and vagina, and neighboring abdominal organs. If a diagnostic error was made when determining the extent of the operation, and the woman had cervical cancer at an early stage, tumor symptoms may appear in the early postoperative period.
The late rehabilitation period is a rather lengthy event that allows a woman to return to a full life. That is why this period needs to be given no less attention than treatment in a hospital. It is recommended to wear a bandage that supports the abdominal muscles. The woman will have to limit physical work, especially heavy lifting, swimming in open water and sexual activity for 2 months after discharge from the hospital.
If the sutures were applied incorrectly, they will contribute to the formation of a cyst. Most often, such a disease is a consequence of many factors, among which may be a violation of the technology of surgical intervention. Photos of the cyst can be found on the Internet; as a rule, this condition is asymptomatic and with minimal risk to health.
Normally, scar and then fibrous tissue forms at the site of the suture, which isolates the vagina and cervix, prevents communication of the genital organs with the abdominal cavity, prevents the spread of infections, as well as the accidental entry of sperm and the associated risk of developing an ectopic pregnancy.
Recovery after discharge
After the woman is discharged home, the late stage of recovery begins. If the procedure went without complications, it lasts about a month, otherwise it is extended to 1.5 months.
A woman must follow these rules:
- wear a support bandage until the abdominal muscles are restored;
- reduce physical activity, avoid active training, sudden movements;
- do not lift loads over 3 kg;
- do not visit saunas and baths, do not take a bath with hot water until rehabilitation is completed;
- do not swim in open waters;
- attend physical therapy classes to restore muscular activity of the pelvis and vagina.
During this postoperative period, the patient’s general condition improves, damaged tissues are completely restored, the psychological mood returns to normal, performance is restored, and the immune system is strengthened.
Prolapse of the cervical stump
This is a fairly rare condition. Most often, its reason is that before the operation there was uterine prolapse or prerequisites for it, which were not completely eliminated. The reasons for this condition are a history of traumatic childbirth, connective tissue diseases, and improperly performed amputation of the uterus.
Prolapse of the cervical stump develops rather slowly and rarely tends to correct itself. Patients report a feeling of a foreign body, abdominal pain, which intensifies when coughing, sneezing, or lifting heavy objects. Urination and defecation are also impaired.
Treatment for this condition is fixation of the cervix using special materials. In this case, transsection is most often performed to provide the greatest scope for the surgeon’s actions. The cervix may be artificially attached to the uterosacral or other ligaments that support the uterus.
Cervical stump cancer
Cervical cancer is a common oncological pathology in gynecological practice. After amputation of the uterus, the likelihood of developing a malignant process in the cervix remains. Moreover, there are situations when, at the time of making a decision on intervention for fibroids or endometriosis, a woman already has a cancerous tumor at an early stage, but doctors mistake the symptoms of cancer for symptoms of uterine disease and ignore them. This leads to the fact that instead of extirpation, a more gentle intervention is performed, and the cancer remains and progresses.
Symptoms of the disease are vaginal discharge, which in the early stages is brownish, then becomes bloody, with an unpleasant odor, and its abundance can vary. The appearance of discharge should especially alert a woman who has had her uterus removed, because normally after this all discharge stops or becomes insignificant.
Later, abdominal pain, urination and defecation problems, and general toxic syndrome appear. A peculiarity of cervical cancer and its stump is the development of metastases to the pelvic lymph nodes. This leads to swelling of the lower extremities and external genitalia, a little later swelling of the fingers and hands occurs, swelling of the veins in the neck are symptoms of late stages with extensive metastases.
Treatment of stump cancer after removal of the uterus is carried out in several ways. Radiation therapy with a maximum dose in the affected area is considered preferable. Chemotherapy is rarely prescribed because it is not always effective. If radiation therapy is ineffective, they resort to surgical intervention - removal of the cervical stump.
Dangerous symptoms, or when to see a doctor?
Both of the above conditions significantly threaten the health and life of the patient, so it is important to recognize dangerous symptoms in time so that the treatment measures taken are effective. You should consult a doctor immediately if:
- Pain appeared in the lower abdomen;
- Any discharge from the genital tract has appeared, especially if the vagina is bleeding;
- Urination and defecation are impaired.
These symptoms occur with both prolapse and cancer of the cervical stump; it is impossible to distinguish these diseases at home without being a specialist. To make a diagnosis, it is necessary to undergo a series of procedures, starting with an examination in a gynecological chair. It should be remembered that one of the diseases does not exclude the other; both diagnoses can accompany each other.
Reviews from various sources
Kristina, 34 years old, Omsk
My second birth was difficult - there was bleeding, the doctor says that they could barely pump it out, although I myself don’t remember that day well at all. Due to bleeding, I had to have my uterus removed, but the cervix was left in to avoid any side effects. Three months have passed, the tears have healed safely, the baby is healthy. Everything is fine with my husband, too, although at first I felt strange. In general, I wouldn’t say that life has improved, but it hasn’t gotten any worse.
Anastasia, 48 years old, Kemerovo
14 years ago I was diagnosed with ovarian endometriosis. Two years of treatment, different medications, the result is quite weak. I wanted a third child, but the gynecologist said that with my illness I would not be able to get pregnant. But I couldn’t recover, it only got worse. Together with the doctor, we made the difficult decision to remove the uterus and appendages. After the operation I had to take hormones, but overall I felt good. I am seeing a gynecologist, and in the near future I will have to stop taking hormones in order for menopause to occur.
Daria, 46 years old, Novosibirsk
It’s been three years since I had my uterus removed. Before the operation, I read reviews, and they said that there was nothing wrong with the operation, they would live a normal life. But that was not the case, after six months some unpleasant sensations began in the stomach, as if the uterus was starting to grow back. Then discharge appeared, it was very unpleasant, my stomach hurt. And only a month ago I went to see a gynecologist, she diagnosed “prolapse of the cervical stump.” Now another operation is needed to restore it all.
Diet in nutrition
For general recovery of the body in the postoperative period, it is necessary to organize a balanced, proper diet. Products are selected with a laxative effect to reduce the load on the abdominal muscles when the urge to defecate occurs.
Healthy products allowed after hysterectomy surgery:
- boiled meat and fish of low-fat varieties;
- vegetable puree;
- low-fat fermented milk products;
- porridge from oatmeal, buckwheat, pearl barley;
- vegetable fats;
- Green tea or lightly brewed black tea is preferable.
It is recommended to exclude from the diet:
- strong coffee or tea, cocoa, chocolates;
- alcoholic drinks;
- sweet pastries made from butter dough;
- carbonated sweet drinks;
- spicy, salty, fatty, fried foods;
- cabbage, legumes;
- smoked meat and fish;
- fat cottage cheese, sour cream, milk.
Dietary recommendations should be obtained from your doctor.