In oncogynecological practice, ovarian cystadenomas are divided into two large groups: serous and mucinous. Serous cystadenoma is a fairly common cystic formation of the internal female reproductive system. It is a true tumor and is characterized by a benign course. However, a distinctive feature of cystadenoma is the high risk of degeneration into a malignant neoplasm. According to statistics, it is diagnosed in 65-71% of cases.
Reasons for the development of cystadenoma
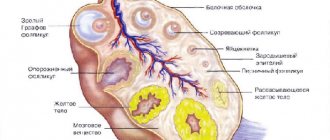
The cause of the development of cystadenoma has not yet been precisely established. The prevailing opinion is that the main reason for the development of cystic ovarian tumors is a disruption of the healing process of functional cysts formed as a result of ovulation. Normally, a follicular cyst formed at the site of the follicle undergoes reverse development and disappears; in the presence of risk factors, the outflow of fluid from the cyst cavity is disrupted, and thus a benign neoplasm is formed. It has been noted that in women who have previously undergone surgery on the ovaries, benign neoplasms are more common, which may be associated with compensatory ovarian hypertrophy.
Risk factors for the development of cystadenoma, in addition to previous surgery, include:
- Concomitant gynecological pathologies, primarily of an inflammatory nature,
- Early menarche
- Late menopause
- Early onset of sexual activity
- Genetic predisposition,
- Hormonal disorders, for example, excess production of estrogen by the body or diseases of the thyroid gland, accompanied by disturbances in the secretion of its hormones,
- Chronic inflammatory processes in the pelvis,
- High-calorie diet, bad habits.
Causes and symptoms of cystoma
Doctors have not yet established the exact cause of the cystoma, however, there are certain theories associated with the appearance of the tumor. These include:
- hormonal imbalance. Since ovulatory proliferation occurs every month, hyperplasia develops over time. Taking coc and frequent pregnancies reduce the likelihood of tumor growth;
- hereditary factors. This parameter is considered fundamental because mutations of the BRCA1 and BRCA2 genes occur;
- ovarian diseases. We are talking about corpus luteum cysts and PCOS;
- menopause. During this period, hormonal changes occur, which serves as a provocateur for cystadenoma.
As for general symptoms, as a rule, they do not appear if the size of the cyst is less than 3 cm. In this case, the patient is under observation and OK is prescribed to her. If the “dropsy” does not decrease, more serious treatment is prescribed. Complaints appear if the size of the cystadenoma is 5-7 cm.
The clinical picture here is as follows:
- constipation;
- pain localized in the lower abdomen and lower back;
- difficulty urinating;
- bloating;
- When a tumor is torsion, acute pain may occur, even to the point of fainting.
A serous cystoma in the right ovary compresses the kidneys, as a result, the outflow of urine is disrupted. The cystoma of the left ovary puts pressure on the intestines.
Types of cystadenomas
There are several types of cystadenomas according to their structure:
- Simple serous cystadenoma. The frequency of occurrence is 10% of all types of cystic neoplasms and about half of serous neoplasms. Single-chamber cystadenomas are predominantly found, but cystadenomas with two or more chambers can be detected. The left ovary is more often affected, since eggs mature in it more often during the reproductive period, but in approximately 10% of these neoplasms are bilateral.
- Papillary serous cystadenoma. The main distinguishing feature of this species is the presence on the inner surface of papilloma-like outgrowths that grow from the walls to the center of the cystadenoma. Although papillary cystadenomas grow more slowly than simple ones, they have a tendency to become malignant. According to the potential for malignant transformation, serous papillary cystadenomas are divided into benign, malignant and borderline.
- Mucinous cystadenoma. A separate type of benign epithelial mucinous tumor, the peculiarity of which is the high content of mucus and mucin protein in the fluid contents of the cyst. Makes up to 30% of all benign ovarian tumors. More often (in 50-70% of cases), these tumors are unilateral, multi-chamber due to the growth of numerous septa, reaching large sizes - up to 10-50 cm. Mucinous cystadenomas, unlike serous ones, appear at an older age - 50-60 years. Characterized by rapid growth. When the wall of the formation ruptures, ascites and pseudomyxoma peritonei occur.
What it is?
Cystadenocarcinoma of the ovary is a malignant neoplasm, which is also called glandular cancer. The oncological process develops on the surface of the epithelium lining the organ, and due to the proliferation characteristics of this type of tissue, the disease in question is more common than other tumors of glandular origin.
Important! Cystadenocarcinoma is a bubble that is filled with liquid contents. Its contours are smooth and clear, its walls do not stretch. The capsule may have one or more chambers, and the size can range from 3 to 12 cm.
Symptoms of ovarian cystadenoma
Cystadenoma, like any other ovarian tumor, may not manifest itself in any way for a very long period of time. The symptoms that appear as the cystadenoma grows are nonspecific and can be as follows:
- an increase in the volume of the abdomen (with unilateral lesions - asymmetrical), a feeling of fullness or bloating;
- feeling quickly full when eating or loss of appetite;
- chronic pain or pulling sensations in the abdomen, especially in its lower parts;
- foreign body sensation
- frequent urination or false urge to urinate,
- constipation,
- pain during sexual intercourse,
- menstrual irregularities, the appearance of dysfunctional uterine bleeding.
In case of complications, such as torsion of the legs, rupture of the cystadenoma, hemorrhage into the cyst cavity, suppuration, symptoms of “acute abdomen” occur - sharp pain in the lower abdomen, aggravated by palpation, a slight increase in temperature, the appearance of a large number of leukocytes in the blood. The development of Meigs syndrome is possible - the appearance of ascites or hydrothorax (effusion in the abdominal and thoracic cavities, respectively).
Possible complications from resection
Even laparoscopic resection (partial excision) of ovarian tissue can be accompanied by complications:
- intolerance to anesthesia;
- accidental damage to blood vessels, intestinal wall, bladder;
- addition of infection;
- bleeding;
- accumulation of fluid or blood at the site of tumor removal;
- adhesive process in the abdominal cavity.
Their risk is much lower than with open surgery, but it cannot be completely eliminated. Most are detected already in the hospital (before discharge) during a control ultrasound, and some can appear at home.
Adhesive process after removal of the ovary
Reasons for an immediate visit to a gynecologist are:
- increased pain in the lower abdomen or constant aching;
- increased body temperature;
- general weakness for 2 or more weeks;
- difficulty and pain when urinating or defecating.
Diagnosis of ovarian cystadenoma
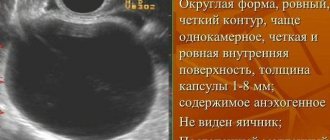
Diagnosis begins with a detailed history taking, with special attention to family history, since there is a genetic predisposition to the development of cystadenomas. Speculum examination and bimanual rectovaginal examination are indicated. A transvaginal ultrasound examination is performed; if a large tumor is detected, it is supplemented by a transabdominal examination. It is also possible to perform a CT or MRI of the pelvic organs in case of suspicion of a malignant process or if the ultrasound data is of little information.
Puncture of cystic ovarian formations, which include cystadenoma, is not recommended for diagnostic purposes, since, according to modern literature, false negative results are quite common; in addition, the development of complications associated with this manipulation is possible.
To exclude a malignant process, a blood test for tumor markers, primarily CA125 and CA19-9, may be prescribed. However, it should be remembered that an increase in the CA125 marker does not always clearly indicate the development of cancer - the level can also increase in the presence of an active inflammatory process.
Gastroscopy and colonoscopy should be mentioned as additional examination methods. Performing a gastroscopy will exclude gastric cancer, since it is characterized by metastasis to the ovary (the so-called Krukenberg metastasis).
A colonoscopy will help rule out damage to the lower intestine if malignancy of the cystadenoma has occurred.
TNM classification
The TNM classification is based on three components:
- T – Tumor – translated from Latin means “tumor”. The indicator determines the quantitative and qualitative characteristics of the neoplasm, and also reveals the degree of its penetration into nearby tissues. The number next to the letter gives the doctor additional information.
- N – Nodus – translated “node”. Indicates the presence or absence of metastases in regional lymph nodes, and also provides information about the prevalence of this process.
- M – Metastasis – “movement”. Information is provided regarding distant secondary foci of the malignant process.
The classification of malignant ovarian tumors according to the TNM system is as follows:
T – original primary tumor:
- T0 – there are no manifestations of the primary tumor,
- T1 – one ovary is affected, its mobility is preserved,
- T2 – both ovaries are affected, they remain displaced,
- T3 – a malignant process affects the reproductive organ and tubes,
- T4 – oncology spreads to organs located nearby.
N – regional lymph nodes:
- N0 – there are no signs of lymph node damage,
- N1 – presence of metastasis to lymph nodes.
M – calving metastasis:
- M0 – there are no signs of distant metastases,
- M1 – presence of distant metastases.
Treatment of cystadenomas
Cystadenoma, being detected at an early stage of its development, can be left under observation, since ovarian cysts spontaneously regress. Typically, expectant management is used when the tumor size is less than 10 cm and without obvious signs of a malignant tumor according to ultrasound results. Control is carried out by ultrasound.
If there is no positive dynamics during observation or larger cysts are detected, conservative therapy is prescribed, primarily the use of hormonal contraceptives, to reduce the size of the cyst or prevent its further growth. The mechanism of action is to reduce estrogen levels and suppress ovulation. Additionally, vitamins (A, E, C, B1, B6, folic acid) and restorative drugs (schisandra, eleutherococcus), and physiotherapy may be prescribed.
If conservative therapy has not had a significant effect on the growth of the cyst over 2-3 menstrual cycles, as well as in the case of an initially large cyst (5 cm or more), surgical treatment is indicated. At the moment, such operations are performed predominantly laparoscopically due to its less traumatic nature, but giant-sized cystadenomas require standard laparotomy. During the operation, enucleation of the cyst or resection of the affected area of the ovary is performed with the maximum possible preservation of healthy tissue in patients of reproductive age. In women with a cystadenoma larger than 3 cm or who are postmenopausal, the entire ovary can be removed, with or without the corresponding fallopian tube. During surgery, regardless of the approach, a thorough examination of the adjacent peritoneum is required, since its damage may be a sign of the presence of a malignant component.
In case of cystadenoma, which is manifested by pain, impaired ovarian function, which persists for more than two menstrual cycles, is single-chamber and has no signs of a tumor process, puncture and aspiration of its contents are possible under ultrasound control or under visual control with laparoscopic access. Using a vaginal ultrasound sensor and a puncture nozzle, a needle is inserted into the cyst cavity. The contents of the cyst are aspirated and sent for cytological examination, and 10-15 ml of ethyl alcohol, which has a sclerosing effect, is injected into the cavity. The aspiration technique is intended primarily for women of reproductive and premenopausal age; in postmenopause, it is used only to relieve symptoms with an accompanying high operational risk. Although this operation is undoubtedly less traumatic, it has a significant drawback - the risk of cystadenoma recurrence is very high.
If a papillary serous cystadenoma is detected, the removed formation is subject to urgent histological examination. If a borderline tumor has been identified, the ovary is removed along with the fallopian tube from the cyst side, a biopsy of the second ovary is performed, and part of the peritoneum is removed.
In some cases, mucinous cystadenoma of the ovary is not an independent disease, but a metastasis of well-differentiated mucinous adenocarcinoma of the appendix, which was not previously diagnosed. Therefore, the clinical guidelines recommend mandatory urgent histological examination of the removed cystadenoma in order to decide whether appendectomy is advisable.
The development of complications is an indication for emergency surgery due to their life-threatening nature.
Treatment to increase your chances of conceiving
After removal of the cystadenoma, hormonal contraceptives are prescribed for 2-3 months when planning to conceive. They create a period of rest for the ovaries, and after they are discontinued, pregnancy often occurs. If there is no fertilization for six months without protection, then use:
- methods of hormonal stimulation of ovarian function;
- physiotherapy for resorption of adhesions in the abdominal cavity (ultrasound, enzyme electrophoresis);
- normalization of weight (low-calorie diet with increased physical activity);
- restoration of patency of the fallopian tubes.
If there is no effect, artificial insemination is performed.
Features of treatment of cystadenomas during pregnancy
Serous ovarian cystadenomas, especially small ones, are not an obstacle to conception and gestation, and therefore can be an accidental finding when performing a screening ultrasound as part of pregnancy management.
The incidence of cystadenomas during pregnancy is low and is about 2%. In most cases, formations are detected during the first trimester and are capable of spontaneous regression in 80-95% of cases.
Cystadenomas themselves do not harm pregnancy, but, firstly, if they are large in size, they can become a mechanical obstacle during the birth process, and, secondly, although the incidence of complications is low, such a risk exists. Therefore, when deciding on the treatment tactics for cystadenoma, it is necessary to compare the risks of complications from the operation and the risks of complications from the cyst.
The operation is performed using laparoscopic access; during its implementation, monitoring of the fetal heartbeat is required. Indications for removal with cystandene during pregnancy are:
- Cystadenoma persisting after 16 weeks of pregnancy,
- The size of the formation is no more than 12 cm,
- No signs of malignancy,
- Damage to both ovaries
- High risk of cyst pedicle torsion or capsule rupture.
Contraindications, respectively, are a gestational age of more than 18 weeks, a tumor size of more than 12 cm, and signs of malignancy of a cystadenoma.
Classification: types and types
The classification of a pathological formation is based on its histological composition.
So, based on tissue composition, they distinguish:
- serous cystadenocarcinoma of the ovary;
- mucinous cystadenocarcinoma of the ovary.
Serous ovarian cystadenocarcinoma is formed from a cilioepithelial cystoma through malignancy. It is more often diagnosed in middle-aged women – 40-50 years old. Often the disease occurs against the background of infertility (primary and secondary), as well as chronic inflammation of the fallopian tubes. This formation makes up the majority (about 70%) of all malignant tumors of the female reproductive glands.
The macroscopic structure is characterized by the presence of papillae on the surface or inside the cystic cavity. Sometimes several pathological formations may occur.
The altered epithelial cells multiply rapidly. Low differentiation of tumor cells is characteristic.
Mucinous cystadenocarcinoma of the ovary is formed from a pseudomucinous cyst. This is a rarer cancer, occurring in approximately 10% of malignant neoplasms.
The macroscopic structure is characterized by the presence of densely located papillary growths on the wall of the primary cyst. Using an electron microscope, you can see highly differentiated mutant cells, differing polymorphism, forming glandular and lattice organelles.
Depending on the type of disease, the form of determinism is determined. Thus, according to the maturity of tumor cells, they are distinguished:
- highly differentiated pathological formation;
- low differentiated.
The lower the differentiation of tumor cells, the more aggressive their behavior and faster their development.
Forecast
Since ovarian cystadenoma is a benign neoplasm, the prognosis in the vast majority of cases is favorable. Borderline papillary serous cystadenomas require close monitoring, as they have the potential for malignant transformation. In addition, cystadenomas have a tendency to recur, especially if the risk factors that contribute to their formation are not eliminated. Therefore, women who have been diagnosed with benign ovarian tumors need not only regular observation by a gynecologist, but also therapy aimed at correcting concomitant diseases: taking combined oral contraceptives, treating chronic inflammatory diseases of the pelvic organs, normalizing the diet.
Until recently, the presence of an ovarian mass, which includes cystadenoma, was an indication for its surgical removal. At the moment, clinical situations have been identified in which active follow-up or conservative treatment is preferable. Thus, a competent risk assessment and the development of individualized tactics for managing patients with cystadenomas are very important, and this is exactly what the doctors at the European Clinic are ready to offer you.
Book a consultation 24 hours a day
+7+7+78
Bibliography:
- Diagnosis and treatment of benign ovarian tumors from the perspective of cancer prevention. Clinical guidelines, 2018.
- Tsareva E.V. et al. Ovarian tumors (clinical case). Bulletin of Medical Internet Conferences. 2021, volume 7, no. 6. P. 802.
- Shavladze Z.N. et al. Borderline serous papillary tumor of the ovaries: personal observation and a brief review of the literature. Tumors of the female reproductive system. 2012, No. 1. P. 117-120.
- Kedrova A.G. et al. Clinical and molecular aspects of mucinous ovarian tumors: etiopathogenesis, individualization of treatment. Clinical practice. 2010, No. 3. P. 20-31.
- Grebenkin B.E., Palakyan L.P. Minimally invasive methods of treating patients with ovarian tumors. Perm Medical Journal. 2008. Volume 25, No. 1. P. 45-48.
Stages
Cystadenocarcinoma also has 4 stages of development. Each of them is characterized by certain symptoms. But it is possible to determine the degree only after surgery to remove the tumor.
Stage 1
The tumor spreads only to the tissue of the affected organ and does not go beyond its boundaries.
Detection of pathology at this stage most often occurs by chance, since there are practically no symptoms of the pathological process.
Stage 2
Specific symptoms begin to appear in accordance with the localization of the focus of the oncological process.
By providing medical care and undergoing surgery to remove the formation, a complete recovery can be achieved.
Stage 3
Metastatic lesions begin to form in neighboring organs. They also affect regional lymph nodes.
The clinical picture is clearly expressed. But even with the necessary treatment measures, it is not possible to achieve complete recovery.
Stage 4
Metastases affect distant organs. The patient's condition deteriorates significantly, most often critically.
At the fourth stage, the tumor begins to disintegrate and becomes inoperable, which makes it impossible to remove it. Only supportive therapy aimed at alleviating the condition is provided.