Many women have heard the diagnosis fibromatosis more than once. What it is? Fibromatosis is the process of replacement of healthy tissue of the cervix with connective tissue, as a result of which the functions of the uterus are disrupted. If treatment is not started on time, fibroids may develop. This is a benign tumor that occurs in 35% of women. Outwardly, it looks like a ball of muscle fibers resembling a knot.
Nodes are in different places. They can grow into the uterine cavity. There is another localization - they can grow outward. As a result of the growth of nodes, the uterus increases in size.
Fibroids are a disease of women of reproductive age, and it depends on the level of sex hormones, which have a stimulating effect on the genitals and can provoke the growth of fibroids. Therefore, you need to pay attention to how to treat uterine fibromatosis, otherwise a more complex disease will appear.
Causes of uterine fibroids
Uterine fibroids are a neoplasm consisting of muscle and connective tissue in the structure of the uterine body, which is distinguished as benign and hormone-dependent.
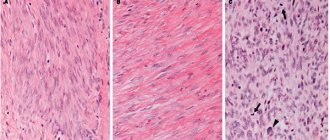
The predominance of muscular elements in it is defined as fibroids, and connective elements - as fibromyoma. Fibroids are diagnosed when the amount of connective tissue in the tumor exceeds the amount of muscle tissue by 2-3 times. If there is more muscle tissue (4-5 times), then fibroids occur. Fibroids consisting of smooth muscle cells of the myometrium are leiomyomas, and those consisting of cross-striated myometrial cells are rhabdomyomas. The pathological condition develops under the influence of many factors that in one way or another affect the functioning of the endocrine or reproductive system of a woman:
- disruption of hormone synthesis by the ovaries;
- imbalance in the number of myometrial cell receptors sensitive to estrogen and progesterone;
- disturbance of hemodynamics (blood flow) in the pelvis;
- inflammation of the internal genital organs;
- metabolic disorders;
- abstinence from sexual activity;
- dysfunction of the immune system, incl. immunodeficiency states;
- disorders of neurological origin, vegetative-vascular disorders;
- anovulation and infertility against its background;
- underdevelopment of the genital organs, infantilism;
- hereditary predisposition, incl. oncological diseases of the abdominal cavity and pelvis in family analysis;
The presence of one or more of the conditions described above does not at all mean the likelihood of a risk of developing fibroids; regarding the latter, several theories have been developed that describe the set of processes that accompany the occurrence of a neoplasm under the influence of just the above factors:
- hormonal theory - its adherents explain the neoplasm by a hormonal imbalance with an increased concentration of estrogen, follicle-stimulating and luteinizing hormones during each menstrual cycle, as well as the absence of an ovulatory peak; against this background, changes occur in the receptor apparatus of myometrial cells and the vascular system of the uterus and ovaries, ovarian function suffers, follicle maturation is disrupted, metabolism in tumor tissues and unchanged uterine tissues is disrupted;
- extramedin theory - hormonal imbalance stimulates epidermal, heparin-binding, transforming, vascular endothelial, insulin-like growth factors and extracellular matrix; the abundance of growth zones in the body of the uterus gives rise to the development and growth of myomatous nodes;
- the theory of myogenic hyperplasia - its adherents call fibroids not so much a tumor as myometrial hyperplasia, which usually occurs against the background of a normal menstrual cycle; The trigger mechanism is tissue hypoxia of the muscular elements of the uterus, which leads to impaired differentiation of myometrial cells that acquire the ability to proliferate.
The reasons for the occurrence of uterine fibroids in such an increased number compared to previous decades are said to be, firstly, the increase in aggressive gynecological interventions - abortions, hysteroscopies and laparoscopies, hysterosalpingographies, biopsies and coagulations of the cervix, diagnostic curettages, removal of the IUD. Secondly, the trend is associated with the active spread of sexually transmitted infections. The frequency of fibroids today is also associated with the improvement of diagnostic procedures, which makes it possible to detect pathology in the early stages and in the absence of characteristic symptoms, even in young women. It is noted that fibroids are typical for women of reproductive age, 20-40 years old, their share of the total number of gynecological diseases is 30%.
Fibroids go through three main stages in their development:
- formation of an active growth zone in the myometrium with acceleration of metabolic processes;
- intensive tumor growth without signs of differentiation of cellular elements;
- expansive growth of the tumor with its differentiation and maturation of cellular elements.
There are several types of uterine fibroids:
- submucosal - prone to atypical degeneration, may be complicated by bleeding and infection; the patients themselves often have metabolic disorders and reproductive function suffers;
- intermuscular - characterized by rapid growth, the shape is often asymmetrical or spherical, usually large in size; develops into degenerative tissues up to aseptic necrosis;
- cervical - characteristic of the area in the supravaginal segment of the cervix, contributes to the displacement of adjacent organs and disruption of their function; does not change in size, is accompanied by pain and menstrual dysfunction.
Fibroids that develop benignly, like muscular hyperplasia (with characteristic slow growth and without proliferative processes), are called simple. When mitotic activity and rapid growth are observed, but no atypical cells are observed, this is a proliferating fibroid. Presarcoma is a neoplasm with atypical phenomena and heterogeneous cell nuclei.
The symptoms of uterine fibroids are determined by the woman’s age, the duration of the pathological process, the localization of myomatous nodes, and the presence of concomitant genital or extragenital pathology.
The main symptoms of uterine fibroids include:
- uterine bleeding - more often in the reproductive period, heavy, prolonged menstruation, sometimes taking on the character of metrorrhagia with subsequent anemization;
- pain in the lower abdomen and lower back - more often in the postmenopausal period, as well as in young patients with a large tumor; may be accompanied by increased body temperature, pain, symptoms of peritoneal irritation, accelerated ESR, and an increase in the number of leukocytes; the pain itself can be of a very diverse nature;
- dysfunction of extragenital organs and systems - dysuric phenomena and constipation
Diagnosis of uterine fibroids
Often, uterine fibroids are detected by a specialist during an initial examination in a gynecological office. A two-handed examination of the vagina will allow you to determine the pathological enlargement of the uterus and study the features of its surface. Transvaginal ultrasound examination of the pelvic cavity organs makes it possible to track the location of the tumor and its size. It is this method that differentiates fibroma from ovarian cystoma. Ultrasound or X-ray hysterosalpingoscopy can reveal submucosal fibroids in the endometrial cavity. If the development of a fibrous tumor occurs with complications, and uncharacteristic discharge is observed between menstruation, the doctor may prescribe additional examination using curettage, endometrial biopsy, histological tissue analysis and MRI.
How to treat uterine fibroids?
To treat uterine fibroids, conservative and surgical treatment can be undertaken.
| Indications | |
| For conservative treatment | For surgical treatment |
| the patient's desire to maintain reproductive function | large uterus (more than 13-14 weeks) |
| course of the disease with mild symptoms | rapid growth (more than 4 weeks per year) or resistance to conservative therapy |
| uterine fibroids not exceeding the size of a 12-week pregnancy | presence of pain, bleeding, dysfunction of other pelvic organs |
| interstitial or subserous (wide-based) location of the node | signs of disturbance of the trophism of the node, necrosis of the node, fibroids with degenerative changes in the tumor |
| fibroids, which are accompanied by extragenital diseases with a high surgical risk | submucosal fibroids, accompanied by long and heavy menstruation, anemia; "nascent" fibromatous node |
| as a preparatory stage for surgery or rehabilitation therapy in the postoperative period | signs of torsion of the subserous node on the “pedicle” |
| fibroids combined with tumors of the genital organs of other localization, adenomyosis, chronic salpingoophoritis, hyperplastic processes of the endometrium | |
| cervical fibroids | |
Conservative treatment is complex and includes the following components:
- diet therapy - complete protein nutrition, improvement of liver function, consumption of foods containing iron;
- vitamin therapy - vitamin and mineral complexes, folic acid, iron supplements, ascorutin;
- use of sedatives - to prevent and eliminate vegetative-vascular disorders; for example, motherwort tincture;
- the use of drugs to normalize periodic blood flow;
- use of immunomodulators and immunostimulants;
- the use of antianemic drugs - to prevent anemia in the presence of bleeding;
- the use of drugs to normalize liver function - medications or choleretic herbs;
- use of hormones (usually for at least six months) - gestagens, estrogen, progesterone, GnRH agonists and antagonists, androgens;
Hormone therapy has a number of contraindications:
- the size of the uterus with fibroids exceeding those at 12 weeks of pregnancy;
- submucous fibroids and fibroids with interstitial localization of the node with centripetal growth;
- fast-growing uterine fibroids, incl. with suspicion of sarcoma;
- fibroids with bleeding and severe pain;
- fibroids in combination with other diseases of the genitals, for example, ovaries, endometrium, uterine appendages;
- somatic pathology, for example, hypertension, obesity, diabetes mellitus, varicose veins, hypercoagulation syndrome, etc.
As part of the treatment of fibroids, it is advisable to use physiotherapeutic techniques. in this case it is:
- electrophoresis of copper sulfate, zinc sulfate or zinc with iodine;
- radon baths;
- iodine-bromine baths;
- constant magnetic field on the pelvic area;
- low-frequency magnetic field on the pelvic area;
- autotransfusion of UV-irradiated blood;
- laser irradiation of blood.
Symptoms
At the early stage of node development, there are no signs. The main symptoms appear when the size of uterine fibroids reaches 5 cm or more.
- Cycle disorders. One of the first signs of the disease is the occurrence of menstrual abnormalities: periods become heavy and painful. This occurs because tumor growth promotes pathological growth of the endometrium. As the nodes enlarge, the tone of the uterus and its contractility decrease, causing menstruation to become longer and irregular, and intermenstrual uterine bleeding occurs.
- Bleeding. They can occur both as a result of menstrual disorders and as a result of tumor injury. Excessive blood loss leads to symptoms of anemia (dizziness, weakness, fainting, irregular heart rhythm).
- Pain in the abdomen and lower back. Twisting of the leg, its separation, compression of nerve endings and poor circulation lead to severe abdominal pain that is not associated with the onset of menstruation. The localization of pain, as a rule, depends on the location of the uterine fibroid nodes. In the presence of a subserous and interstitial tumor, a nagging pain is felt in the pubic area and in the lower back, which is associated with stretching of the uterine wall and peritoneum. Submucosal fibroma is characterized by the appearance of spasmodic pain in the lower abdomen, intensifying during menstruation, radiating to the bladder and rectum.
- The birth of a node. A large submucosal fibroid of the uterus enters the vagina through the cervix, which leads to tumor rupture and severe bleeding. Pain and inflammation occur.
- Impact on the pelvic organs. The pressure of the tumor on the bladder is manifested by difficulty urinating. An inflammatory process occurs that can spread to the kidneys. There may be an increase in temperature and the appearance of pus in the urine. If the node is located on the back wall, then it puts pressure on the rectum. This causes flatulence and constipation.
What diseases can it be associated with?
The progression of fibroids in its development entails the following functional disorders in the body:
- from the urinary system - expansion of the pyelocaliceal system up to hydronephrosis, which can also result in urinary incontinence;
- from the liver - disorders of hormonal metabolism, metabolism of proteins, fats and carbohydrates;
- from the cardiovascular system - myocardial dystrophy, anemia, hypoxia, hypovolemia, disorders of the coagulation system;
- from the nervous system – there is a tendency to hysteria, depression, psychasthenia;
- from the intestines - disturbances in the act of defecation (with so-called retrocervical fibroids).
Uterine fibroids are usually associated with the following diseases:
- glandular cystic hyperplasia;
- endometrial polyposis;
- endometriosis;
- endometrial cancer;
- hypertonic disease;
- obesity;
- cardiac ischemia.
Uterine fibroids are a predisposing factor in the development of primary and secondary infertility, which is associated not only with the size and location of fibroids, but also with impaired ovarian function, inflammatory diseases of the uterus and appendages, and concomitant endometriosis.
Reasons for appearance
According to experts, the cause of fibroma formation may be genetic predisposition and hormonal imbalances occurring in the body. Heredity is caused by changes in cells that later form a neoplasm.
With hormonal changes, an imbalance of estrogen and progesterone occurs. In this case, a neoplasm can develop due to excess estrogen content, or both. With the help of modern medications, it is possible to restore hormone levels and achieve tumor involution.
The causes of hormonal imbalance can be different. For example, weakened sensitivity of uterine receptors for the production of progesterone leads to a predominance of estrogen in the body.
Impaired functionality of the ovaries prevents the full production of hormones in them. Dysfunction can be provoked by inflammatory processes occurring in the ovaries or appendages, the presence of cysts and other pathologies.
Disturbances in the functioning of the central nervous system can also cause hormonal imbalance, and as a result, the development of fibroids. The functions of the nervous system are especially disrupted by frequent stressful situations, neurological diseases and head injuries.
Other provoking factors include:
- long-term use of hormonal contraceptives;
- damage to the uterus during abortion and curettage;
- absence of pregnancy and lactation up to 30 years of age;
- frequent and long exposure to the sun or solarium, negative effects of ultraviolet radiation;
- irregular or promiscuous sex life;
- disorders of the thyroid gland and endocrine system.
Overweight women with metabolic disorders are at risk. Chronic infectious and inflammatory diseases of other organs can provoke tumor growth.
Treatment of uterine fibroids at home
Treatment of uterine fibroids is possible at home if the choice falls on conservative therapy. However, the administration of medications often occurs on an outpatient basis, where the patient is under the constant supervision of specialists. To take medications and carry out physiotherapeutic procedures, a woman may be advised to regularly visit a medical facility, but the need for surgical intervention is a reason for full hospitalization.
The rehabilitation period after the elimination of fibroids can take place in a sanatorium-resort environment. Women with this diagnosis are recommended to undergo balneotherapy using radon and iodine-bromine waters. Subsequently, the woman needs regular follow-up.
Uterine fibromatosis: what is it, is the disease dangerous?
Uterine fibromatosis is a fairly common gynecological disease in women of reproductive age. This is a pathological process in which the acceleration of cell division in the muscle layer occurs and their replacement with altered connective tissue, which differs from a healthy one in a denser structure and reduced ability to contract.
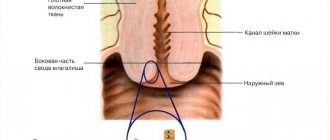
The diagnosis of uterine fibromatosis is established on the basis of ultrasound data and laboratory tests. Pathology is the initial stage of the development of myomas and fibroids. To understand about uterine fibromatosis and what it is, a photo of the development of the disease is presented below. Here you can see how fibromatous nodes affect the muscular layer of the uterus.
Modern medicine cannot say exactly why the disease develops. Research shows that there are several factors, the presence of which provokes changes in the myometrium:
- hormonal imbalances;
- viral and infectious diseases of the pelvic organs;
- trauma to the uterus (abortion, difficult childbirth, curettage, uterine surgery);
- heredity.
To say about fibromatosis of the uterine body that this disease is life-threatening is not true. The pathology is well treated and the development of the disease can be avoided. Fibromatous nodes are benign neoplasms, and the percentage of their degeneration into malignant tumors is almost zero. A complication of the pathology is the formation of large fibroids and myomas, which cause uterine bleeding, pain and discomfort in the abdomen and lower back, problems during pregnancy (prevent the attachment of a fertilized egg, provoke miscarriage). To treat fibromatous nodes, it is rational to use uterine artery embolization, which is a minimally invasive procedure, does not cause an allergic reaction, and acts quickly and effectively. Embolization of the uterine arteries restores reproductive function and after a short period of time a woman can plan a pregnancy. Uterine artery embolization is a treatment method recommended by the expert council of our site.
There are two types of fibromatosis:
- diffuse fibromatosis of the uterus: the area of pathologically changed cells does not have clear boundaries;
- nodular fibromatosis: more prone to developing fibroids.
Pathological areas are localized in various areas of the myometrium. They can grow towards the abdominal cavity, or the space of the uterus, or located within the muscle layer.
Treatment of uterine fibroids with traditional methods
As an independent measure, treatment with folk remedies is ineffective for uterine fibroids. However, it can be a successful addition during the recovery phase or as an adjunct to drug, often hormonal, therapy. Any prescription deserves discussion with your doctor, after whose approval they can be used:
- Arnica mountaina - alcohol tincture, bottles of 15, 25, 40 ml are sold in the pharmacy; take 30-40 drops three times a day;
- medicinal letter - 10 grams of dried herb, pour 100 ml of vodka, leave for 10-12 days in a dark place, strain; take 25 drops three times a day;
- intoxicating harelip - pour 20 grams of dried leaves with a glass of water, place in a water bath and, stirring regularly, leave for 15 minutes, strain after 45 minutes; take 1/3 cup three times a day;
- stinging nettle - 1 tbsp. Pour a glass of boiling water over the crushed leaves, cover with a napkin, leave until cool, then strain; take 1 tbsp. three times a day before meals;
- stinging nettle - 1-2 tbsp. pour a glass of boiling water over the crushed flowers, leave under a lid or a napkin for up to two hours, strain; take 2-3 tbsp. three times a day;
- gray alder - place 10 grams of alder fruits and bark in a thermos, pour a glass of boiling water, leave for 12 hours. then strain; take 3-4 times a day after meals;
- cotton - 10 grams of crushed dried cotton root, pour a glass of water, place on low heat and boil for 15-20 minutes, then cool and strain; take 1 tbsp. three times a day.
Reasons that provoke the formation of fibroids
Modern medicine carefully studies the exact causes and signs of tumor manifestation. Doctors were able to provide answers to some questions, but the reasons that will be discussed below can only be considered accurate with a big stretch.
Attention! Uterine fibroids often affect young women of reproductive age, since the development of fibroids is influenced by the active production of estrogen. But during menopause, a tumor can also develop and increase in size.
- Hereditary factor. The tendency to the disease is hereditary, so if your female relatives had such a disease, then you need to be especially careful and go to see a gynecologist as often as possible in order to know for sure that everything is fine with your reproductive system.
- Excess weight often provokes the development of tumor processes.
- It is generally accepted that the main function of a woman is childbearing, so if she decides not to give birth at all in her life, this can trigger the development of a tumor. In addition to the tumor, menopause in such women may occur much earlier than in those who have given birth at least once. However, if a woman has given birth frequently, more than 3 times, this also increases the risk of tumor development.
- The trend now is for girls to start menstruating earlier than their grandmothers. Both late and earlier onset of menstruation is not good, and if a girl begins menstruation before 10 years of age, then her female health needs to be monitored more carefully and risk factors excluded.
- The highest incidence of uterine fibroids is observed in women of African-American descent. Therefore, if you have such roots, then you need to be aware of the risk factors and visit a doctor.
- Psychosomatics also plays an important role in the development of tumor diseases. Therefore, if a woman is often exposed to stress, has sexual relationships that do not satisfy her, has fears and resentments, then a tumor disease may well appear.
- Often, uterine fibroids occur after an abortion or vaginal cleansing procedure.
- A long-term inflammatory process in the genital area, which has not been treated for a long time, also leads to tumors, including fibroids.
Treatment of uterine fibroids during pregnancy
Uterine fibroids, as experts note, are getting younger and today are diagnosed not only in women of late reproductive age, but also in young girls. This is largely determined by hereditary factors and the influence of various causes. Uterine fibroids are not malignant diseases, and therefore surgical intervention is not recommended. Against this background, doctors allow a woman to become pregnant, and therefore pregnancy and fibroids are completely compatible phenomena. Of course, you can’t expect your pregnancy to be worry-free.
The most common consequences of this combination are changes in myomatous nodes and changes in the placental bed and various morphological changes in the placenta. The most common complications include premature termination of pregnancy, isthmic-cervical insufficiency, and placental insufficiency. Therapeutic measures for uterine fibroids in a pregnant woman are aimed exclusively at the prevention or treatment of such complications.
It is recommended to continue pregnancy in patients with low-risk uterine fibroids. If there is a high risk of complicated pregnancy and childbirth, the issue of continuing pregnancy should be approached individually.
Contraindications to continuing pregnancy in patients with high-risk uterine fibroids are as follows:
- suspicion of a malignant tumor of any location;
- submucosal localization of the myomatous node, disrupting the condition and growth of the fetus; necrosis of the myomatous node and a high risk of spread of the inflammatory process throughout the uterus;
- cervical-isthmus localization of a large myomatous node, which means a real threat of miscarriage, the development of intrauterine infections of the fetus, and bleeding;
- large myomatous nodes (more than 15 cm in diameter), their low location and multiple numbers.
- large size of the myomatous uterus;
- critically late age of a primigravida (over 43-45 years old) in combination with high-risk factors;
- poor health of the patient.
The last resort for treating a tumor in a pregnant woman is myomectomy. This is a very unsafe operation during pregnancy. The technique in case of pregnancy differs from the same, but for a non-pregnant woman. Surgery is performed only when the leg of the subperitoneal node is torsed and the phenomena of “acute abdomen” occur. Very rarely, a rupture of a vessel on the surface of one of the fibroid nodes is possible with symptoms of acute intra-abdominal bleeding.
At 37-38 weeks, pregnant women with fibroids are hospitalized for examination, preparation for childbirth and selection of a rational method of delivery. Often this becomes a cesarean section, and in some indications, removal of the uterus after extraction of the fetus.
Leading clinics in Israel
Assuta
Israel, Tel Aviv
Ikhilov
Israel, Tel Aviv
Hadassah
Israel, Jerusalem
Uterine fibroids (fibroids) are divided into types, depending on the nodal location:
- Submucosal fibroids develop under the lining inside the uterine cavity;
- When fibroid nodes are located in the muscle tissue of the posterior wall of the uterus, it is called fibromatous interstitial myoma (intramural);
- In another type, nodular fibroids are located under the outer lining of the uterus, irritating the peritoneum and putting pressure on neighboring organs - subserous fibroids;
- Stem-shaped fibromas can form as a result of the appearance of a stalk in subserous tumors (the development of such a fibroma is accompanied by bending of the stalk and severe pain);
- Interligamentous fibroids are located between the supporting ligaments of the uterus (their removal carries a high risk of damage to other organs and blood vessels);
- If the nodes are directed into the uterine cavity and interfere with the bearing of the fetus, at the same time causing bleeding (due to detachment of the uterine mucosa), then this form is called submucous fibromatous. It doesn't happen very often.
This fibrous tumor grows quite slowly and usually does not cause discomfort due to its small size, but it can grow to be gigantic. The most correct name for fibroma is uterine leiomyoma (myofibroma), which is a variation of a mesenchymal tumor.
Treatment of other diseases starting with the letter - f
| Treatment of pharyngitis |
| Treatment of breast fibroadenoma |
| Treatment of pulmonary fibrosis |
| Treatment of liver fibrosis |
| Treatment of phimosis |
| Treatment of folliculitis |
| Treatment of yaws |
| Treatment of furunculosis |
The information is for educational purposes only. Do not self-medicate; For all questions regarding the definition of the disease and methods of its treatment, consult your doctor. EUROLAB is not responsible for the consequences caused by the use of information posted on the portal.
Clinical picture
Even if the tumor has reached a large size, there are often no symptoms of uterine fibroids. The tumor is often discovered during a routine examination by a gynecologist.
Main signs of the disease:
- Heavy menstrual bleeding (menorrhagia) with blood clots.
- Frequent urination or the urge to urinate, caused by pressure of the tumor on the bladder.
- Constipation due to compression of the rectum.
- Feeling of heaviness, fullness in the abdomen.
- Pain with uterine fibroids usually appears during menstruation; in the later stages it becomes constant, aching, in the lower abdomen or lower back.
- An increase in abdominal circumference, which sometimes requires changing clothing sizes while maintaining the same weight.
- Infertility or miscarriage.
- A mass in the uterine area discovered by a doctor during a two-manual gynecological examination or ultrasound.
With a small tumor, a normal pregnancy is quite possible. However, it happens that the disease causes infertility or miscarriage. When the node is located near the mouth of the tubes, a mechanical obstacle appears for the germ cells. A cervical node often causes miscarriage. A large formation can cause disruption of fetal development. Uterine fibroids usually do not change in size during pregnancy, but such patients need more careful monitoring.
The issue of delivery is decided in each case individually.
When do you need to see a doctor urgently?
Sometimes situations arise when you cannot do without urgent medical care. Is fibroid dangerous? Yes, in addition to problems with pregnancy, it can become a source of bleeding or death (necrosis) of the tumor node.
You should definitely contact a gynecologist if you have the following signs:
- irregular menstrual cycle, heavy periods, bleeding between periods;
- increasing pain in the pelvis or abdomen;
- fever or night sweats;
- increase in abdominal circumference;
- inability to get pregnant.
You need to call an ambulance in the following cases:
- menstrual bleeding requiring more than 3 sanitary pads per hour;
- severe or prolonged pain in the pelvis or abdomen;
- dizziness, chest pain and shortness of breath in combination with vaginal bleeding;
- bleeding from the vagina during actual or possible pregnancy.
To prevent serious complications from developing, timely diagnosis and treatment of uterine fibroids is necessary.