Kuveler's uterus is a symptom complex that occurs as a result of premature detachment of a normally located placenta and saturation of the myometrium with blood. The condition is manifested by acute abdominal pain and symptoms of massive internal bleeding, leading to intrauterine fetal death. Diagnosed intraoperatively during emergency caesarean section. Treatment of Kuveler's uterus consists of stopping bleeding through a radical operation - extirpation of the uterus while preserving the ovaries and tubes. Methods of organ-preserving operations have been developed and applied.
General information
Couveler's uterus, or uteroplacentral apoplexy, was first described in 1911 by the French gynecologist Alexandre Couveler. He characterized the apoplectic uterus as blood-soaked, cyanotic and incapable of contraction, with pinpoint hemorrhages on the serosa. This condition is a rare complication of premature placental abruption, which occurs in 0.4-1.4% of all pregnancies. Of all cases of abruption, Kuveler's uterus develops in 3.4-6.4%. Maternal mortality from this complication reaches 5%. The fetus most often dies in utero.
How to prevent the appearance?
There is no specific prevention for the development of Couveler syndrome. All measures are aimed at preventing premature placental abruption. Since abruption is most often provoked by impaired blood circulation between the fetus and the pregnant woman, prevention includes:
- Timely treatment of gestosis;
- Therapy of vascular diseases;
- Limitation of physical activity;
- Refusal of sexual contacts;
- Regular visits to the gynecologist, pregnancy screening.
If the risk factor for the development of gestosis is high, the doctor prescribes an individual plan to prevent complications, prescribing the following medications:
- To improve metabolic processes;
- Antihypertensive drugs;
- Sedatives;
- Vitamins.
At the first signs of dysfunction of the placenta in the form of tachycardia in the fetus, a set of measures should be taken to prevent a threatening development of the situation.
Couveler's uterus is a complex of symptoms that poses a threat to the life of a pregnant woman, associated with the development of bleeding as a result of weakening of the placenta and blood entering the uterine muscles.
This type of pathology occurs with a frequency of 0.5-1.5%.
Couveler's uterus is otherwise called uteroplacental apoplexy. This syndrome was first described by A. S. Couvelaire, a French gynecologist, in 1912. Hence the name.
Symptoms of Couveler's syndrome
This syndrome is manifested by rapidly increasing pain in the lumbar region, which is similar to pushing, anxiety, nausea, and mild bloody vaginal discharge.
This condition is also characterized by sudden and strong movements of the fetus, changes in the quality of heartbeats; over time, they lose their rhythm and are almost not audible. It is impossible to feel the fetus in the uterus.
In addition, toxic damage to the vascular system occurs, which results in hemorrhages in the muscle of the uterus, genitals and beyond.
Due to the high level of risk of developing hypovolemic shock, atonic bleeding, and sepsis, the situation of uteroplacental apoplexy has an unfavorable prognosis, since it threatens the woman’s life. Therefore, it requires immediate surgical delivery.
Causes of premature placental abruption
As a rule, this syndrome develops in cases of late gestosis in pregnant women, especially in the presence of pyelonephritis, hypertension, diabetes mellitus, acute viral infections during pregnancy, liver and heart diseases.
During childbirth, Couveler's syndrome develops with discoordinated labor, a short umbilical cord, abdominal trauma, late rupture of the membranes, rapid rupture of water in case of polyhydramnios, chronic fetoplacental insufficiency, location of the placenta on fibromatous nodes.
Prevention of the development of this syndrome comes down to timely treatment of pregnant women with somatic diseases and late gestosis; as well as careful attitude to the process of childbirth.
Causes
The cause of the development of Kuveler's uterus is placental abruption and internal bleeding. Normally, separation of the placenta from the decidua occurs in the third stage of labor. If the process starts during pregnancy, this threatens the development of acute fetal hypoxia and its death. The following factors predispose to detachment:
- Arterial hypertension. If hypertension existed at the time of conception, improper formation of placental vessels occurs. During pregnancy, placental insufficiency is observed, and gestosis may develop. Frequent increases in blood pressure and severe gestosis can lead to abruption.
- Pathology of the uterus . Chronic inflammatory processes, complicated childbirth, operations and consequences of abortion lead to microdamage and changes in the structure of the endometrium. In pregnant women, the formation of the placenta is disrupted. When combined with additional factors, the likelihood of placental abruption increases.
- Coagulopathies . Diseases that increase the risk of thrombosis worsen during pregnancy. Microthrombi clog the vessels of the placenta, which causes its detachment and abdominal bleeding. Pathology of blood coagulation and a tendency to microthrombosis is observed in autoimmune pathologies: systemic lupus erythematosus, antiphospholipid syndrome.
- Uterine fibroids . Nodes located in the thickness of the myometrium change the nature of blood flow and nutrition of the endometrium. Attachment of the chorion in the projection of the nodes increases the risk of circulatory disorders during late pregnancy, leading to feto-placental insufficiency and fetal hypoxia.
- Extragenital diseases. The likelihood of impaired formation of placental vessels increases with diabetes mellitus, hypothyroidism, and anemia. The pathology may be associated with the effects of smoking, alcohol abuse in the early stages of pregnancy, when the formation of the chorion occurs.
The presence of predisposing factors does not always mean that placental abruption will occur. Producing causes include polyhydramnios, carrying twins, blunt abdominal trauma and premature birth.
Kuvler's uterus and pregnancy, what kind of pathology, how dangerous it is, treatment
Uteroplacental apoplexy sounds ominous. Couveler's uterus and pregnancy are classified as a complication that provokes placental abruption prematurely. Kuveler's uterus is a detachment of an embryonic organ, which is accompanied not only by heavy bleeding, but also by the formation of blood stagnation in the abdominal area.
Culever's uterus is a whole group of pathologies that are accompanied by complications and bleeding that are diagnosed only during gestation.
This syndrome does not appear very often in pregnant women. In this case, the uterus stops contracting and becomes saturated with blood, sometimes turning blue with pinpoint bruising.
Causes
Any pathology during pregnancy occurs during a malfunction in the human body.
Occurs during the development of various pathological processes and leads to circulatory disorders. Let's analyze the most common pathologies:
- toxicosis in late pregnancy. Most often it is provoked if a pregnant woman does not receive proper medical care;
- a sharp increase in blood pressure;
- swelling, loss of protein in urine and cramps;
- hypotension;
- for chronic diseases of the cardiovascular system;
- with kidney pathology;
- pelvic inflammation;
- endocrine disorders;
- diabetes;
- pathology of the structure of the uterus;
- deformation of the uterus during childbearing;
- difficult childbirth or complications after surgery;
- incompatibility of the Rh factor of the blood of the woman and the fetus;
- autoimmune disease;
- poor blood clotting;
- rapid outpouring of water;
- irregular contractions of the uterus;
- incorrect selection of medications during pregnancy;
- bad habits: smoking and alcohol;
- pathogenesis.
The causes of development may arise due to deterioration of blood flow in the subplacental zone. The villi that connect the uterus and placenta cease to perform their function.
The connection weakens and the vessel bursts. The placenta stretches, cracks form in it, and the process of detachment begins.
Symptoms
If the expectant mother feels discomfort, then she should consult a doctor immediately. With the help of modern equipment, he will be able to determine the severity of the situation.
A deformed or short umbilical cord is the first sign of the development of pathology. Sometimes it occurs when a woman does not carry the fetus to term or carries the fetus beyond term.
If the child is large, polyhydramnios or oligohydramnios may occur, which will provoke this disease.
Abdominal trauma or gross obstetric intervention.
Manifested by the following symptoms:
- lower back pain;
- bleeding;
- nausea;
- vomit;
- convulsions;
- panic fear;
- constant anxiety and sleep disturbances;
- strange fetal behavior;
- fetal heart rhythm disturbances;
- severe pain between contractions.
Diagnosis is based on clinical symptoms or examination.
The doctor will immediately notice that the fetus is difficult to palpate.
An ultrasound will be prescribed, which will show thickening and neoplasms between the wall of the uterus and the placenta, and destruction of blood vessels.
It would also be advisable to prescribe CTG.
Treatment
Can only be treated through surgery. The attending physician most often prescribes an emergency caesarean section under full anesthesia.
https://www.youtube.com/watch?v=OAHZdFrgOOE
The decision is not influenced by the duration of pregnancy.
After the baby is born, the surgeon evaluates the condition of the uterus and placenta.
If the damage to the vessels is not severe, it becomes possible to bandage them. But more often than not, the uterus is removed immediately to avoid complications after surgery.
Not only the uterus is removed. Extirpation is also carried out. In the postoperative period, blood transfusions and infusion therapy are prescribed.
The doctor prescribes medications that will restore blood circulation if the uterus has been preserved.
Sometimes doctors have to remove the ovaries and tubes. In this case, hormone replacement treatment is prescribed.
Important! According to statistics, if you do not see a doctor in time, about 20% of women die along with the fetus. Death is caused by bleeding and hemorrhagic shock. If measures are taken on time, the child is born healthy and the mother remains alive, then the uterus is completely removed.
Preventive actions
Due to the fact that Couveler's uterus is a rare syndrome, doctors have not identified any special preventive measures.
The fact is that specialists act according to the situation and a general analysis of symptoms already adjusts the treatment. The main thing is to prevent premature placental abruption.
It is worth conducting a thorough examination to determine whether there is a deficiency in the circulatory process.
Diagnosis is carried out in the fetus-placenta-mother chain.
If you study extragenital pathologies in time and carry out timely therapy for gestosis, you can significantly reduce the risk of symptoms.
A specialist can detect already in the first weeks of pregnancy the danger and the presence of factors that may be provoking.
In this case, preventive measures are prescribed according to an individual plan for each woman in labor.
The most commonly prescribed medications are:
- improve metabolism;
- contain the necessary complex of vitamins.
Based on the cardiogram and the behavior of the fetus in the womb, the first signs of hypoxia will be immediately identified and preventive measures will be taken that will stop the development of the syndrome in the bud.
In order not to put yourself and your baby at risk, it is worth undergoing a comprehensive examination in the first weeks of pregnancy.
On a note! Doctors advise limiting sexual contact with a partner if there is a risk of pathologies and contacting doctors at the first sign of an unfavorable condition of the fetus or mother.
Pathogenesis
The placenta is attached to the decidua of the uterus by anchor villi. Rupture of the vessel in them leads to bleeding and the formation of small hematomas. Gradually they merge into a large one and peel off the placenta from the muscle layer. If the rupture occurs along the edge, external bleeding begins. Otherwise, a retroplacentral hematoma will form.
Continued bleeding leads to blood saturation of the placenta and myometrium. The wall of the uterus becomes overstretched and cracks appear. They receive blood, which can reach the serous cover, and after its rupture, exit into the parametrium and abdominal cavity. A large amount of thromboplastin is formed at the site of placental abruption. It penetrates the systemic bloodstream and leads to the development of DIC syndrome. The bleeding intensifies, causing severe hemorrhagic shock, and can result in the death of the woman.
Limiting physical activity
Expectant mothers who have problems with the cardiovascular system, as well as those who have placenta previa, should completely limit physical activity. Otherwise, sudden force may cause vascular damage and a hematoma may appear between the uterus and placenta.
If bleeding occurs during pregnancy, which is caused by placenta previa or low position of the placenta, then you should be especially careful about yourself. Your doctor may recommend bed rest. Listen to the advice of a specialist.
Symptoms of Cuveler's uterus
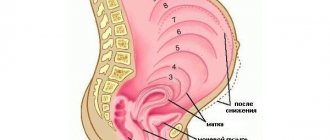
The pathology is manifested by symptoms of placental abruption in severe form. Suddenly, acute pain appears in the abdomen, with no external bleeding or minor discharge. The location of pain depends on the placenta insertion site. If the fetal site is located along the back wall, pain radiates to the lower back and sacrum. Abruption of the placenta, attached along the anterior wall, causes acute pain below the navel and the formation of local swelling. Contractions may occur. When the volume of the hematoma reaches 150 ml, uterine hypertonicity occurs, the myometrium does not relax, and the abdomen becomes rocky to the touch.
The fetus is in a state of acute hypoxia, which is manifested first by a sharp increase in its activity, followed by a complete lack of movement. The child dies when 1/3 of the placenta is detached. When a woman loses 300 ml of blood, hemodynamic disturbances appear and symptoms of hemorrhagic shock appear. She feels weak, dizzy, tachycardia occurs, the skin turns pale and sweat appears. Breathing becomes rapid and shallow. Loss of consciousness may occur.
Why might a complication occur, and how to recognize it?
During the normal development of pregnancy, the placenta maintains its position throughout the entire period of gestation. She begins to be rejected after the actual delivery. If this phenomenon occurs prematurely, there is a risk of hypoxia when the fetus experiences oxygen starvation. The initial causes that constitute the prerequisites for the appearance of pathology are still not fully understood by doctors. At the same time, they identified the main factors that determine the group of predispositions to the development of uteroplacental apoplexy. These include:
- addiction to alcohol, drugs, smoking;
- multiple pregnancy;
- hypertension;
- preeclampsia;
- diabetes;
- toxicosis in the third trimester of pregnancy.
Diagnostics
Couveler's uterus is confirmed intraoperatively during caesarean section. The main diagnosis before surgery is aimed at establishing the fact of placental abruption. Clinical symptoms, medical history, and obstetric examination are taken into account, which is supplemented with instrumental diagnostics. Laboratory methods are necessary to clarify the severity of the condition.
- Examination on the chair. Bloody discharge is noticeable in the genital tract, but it may be absent if central detachment occurs. The cervix is closed; for a short period of time there are no signs of cervix maturation. The amniotic sac is intact, but tense, and no water is leaking. The presenting part of the fetus is above the entrance to the pelvis.
- External obstetric examination . Characterized by hypertonicity of the uterus, its increase in size, and severe pain. If the placenta is located anteriorly, the uterus may be deformed by local protrusion. In the case of antenatal death, there is no fetal movement, and the heartbeat cannot be heard with an obstetric stethoscope.
- CTG . According to cardiotocography, fetal hypoxia is diagnosed, the heartbeat is weak, and bradycardia is characteristic. CTG Fisher score is less than 5-6 points. There is no fetal movement. In case of antenatal death, the heartbeat is not audible on CTG.
- Ultrasound of the uterus . An echo-negative zone is determined between the placenta and myometrium. You can approximately calculate the area of the separated area of the placenta. The fetal heartbeat continues until its death, but motor activity is reduced. The cervix is closed and of normal length.
In the presence of bloody discharge from the genital tract, differential diagnosis is carried out with bleeding associated with placenta previa. It is also necessary to differentiate the condition from uterine rupture based on the scar. In the latter case, the history indicates a previous cesarean section or plastic surgery on the uterus.
Treatment of Cuveler's uterus
The gynecologist's tactics depend on the severity, complications in the form of DIC or hemorrhagic shock. Conservative therapy or expectant management for severe detachment leading to the Couveler uterus is not used. The purpose of surgical intervention is to save the life of the mother, since the child often dies on the way to the maternity hospital.
Drug therapy
Before the operation, hemodynamic correction, blood loss compensation, and treatment of disseminated intravascular coagulation are performed. For this purpose, transfusion of fresh frozen plasma, cryoprecipitate, platelet concentrate, administration of recombinant factor VIIa, and antifibrinolytics are carried out. Whole blood is prohibited for use in DIC. Intravenous infusion of colloid and crystalloid solutions is continued after surgery, their ratio and volume are calculated individually. Narcotic analgesics are used for pain relief in the first few days.
Surgery
In the practice of most obstetric hospitals, premature detachment with the formation of the Couveler uterus is regarded as an indication for cesarean section. This is one of the few cases where surgery is performed on a dead fetus. In other situations, when a child dies in utero, childbirth is carried out through natural means. Caesarean section is the initial stage of surgical treatment of the Couveler uterus. After removing the fetus and assessing the contractility of the uterus, a decision is made to extirpate the organ along with the cervix while preserving the appendages.
Experimental treatment
In Western Europe and the USA, Couveler's uterus is not considered an absolute indication for radical surgery. Organ-preserving techniques have been developed and are being successfully used, which are becoming increasingly widespread in gynecological hospitals in the CIS countries. The main condition for their use is the absence of DIC syndrome and stable hemodynamic parameters in the mother. After the fetus is removed, the following can be done:
- Seam according to B – linch . This is a compression suture that is placed through the fundus, similar to the straps of a backpack. It leads to compression of the arcuate arteries, the largest vessels arising from the uterine artery. The effectiveness of the technique is 90%.
- Omentouteropexy . The first stage of the operation involves ligating the uterine arteries at three levels on both sides to stop bleeding. The second stage involves suturing the omentum to the myometrium for its revascularization and the formation of vascular anastomoses.
- Embolization of the uterine arteries . The operation is performed by a vascular surgeon. A gelatin sponge is passed through the femoral vein to the arteries supplying the uterus. It stops the bleeding, and after a month it completely resolves.
Organ-sparing operations allow women who were diagnosed with abruption during their first pregnancy, complicated by Kuveler's uterus, not to lose the chance to have children in the future. Statistics show that with the right tactics, patients can have a normal pregnancy after treatment.
Symptoms of the syndrome
Couveler's syndrome is not asymptomatic. This pathological condition progresses rapidly. The main symptom of uteroplacental apoplexy is external bleeding.
Attention! Bleeding is not always the main sign of pathology; often all the blood accumulates in the uterus, so vaginal bleeding is not significant.
Placental abruption is manifested by severe pain in the lower abdomen and lower back, which resembles pushing. Kuveler's uterus also causes the following symptoms:
- nausea occurs, in rare cases it turns into vomiting;
- the woman begins to panic, worry about the health of the baby, this leads to a rapid heartbeat;
- due to the lack of oxygen and substances necessary for the child, the fetus becomes too mobile, movements are sudden, and the baby also experiences a heart rhythm disturbance;
- symptoms of internal bleeding, up to the appearance of acute vascular insufficiency, characterized by a sharp drop in arterial and venous pressure.
The appearance of such signs cannot be ignored. Uteroplacental apoplexy threatens the life of the child. If you find signs of placental abruption, immediately call an ambulance and do not self-medicate. Only an experienced doctor will be able to make a diagnosis and prescribe appropriate therapy.
Prognosis and prevention
The prognosis depends on the severity of the pregnant woman’s condition and the level of equipment of the medical institution. The question of the birth of a living fetus is not raised; in most cases, with a Kuveler uterus, the child dies. Medical actions are aimed at preserving the life of the mother. With timely assistance and the availability of drugs to correct DIC, the chances increase. Therefore, the appearance of bloody vaginal discharge during pregnancy is an indication for an emergency visit to an obstetrician-gynecologist. Prevention consists of careful preconception preparation and correction of extragenital pathologies that can cause placentation disorders.
| Literature1. Organ-preserving tactics for Kuveler’s uterus / Einish E.A., Krot I.F., Vakulchik I.O., Kiryanova V.L. - 2013.2. The problem of premature abruption of a normally located placenta / Amanzholova Z.D., Kobzar N.N., Bizhanova M.O.// Materials of the X Anniversary All-Russian Scientific Forum “Mother and Child”, Moscow, September 29. – 2 Oct. 2009.3. Omentouteropexy for Kuveler's uterus: a clinical case / Evseeva M.P., Ivanyan A.N., Kirakosyan L.S. // Scientific bulletins of Belgorod State University. Series: Medicine and pharmacy. – 2021. |
VKontakte
LiveJournal
Basic definitions
During pregnancy, a woman may encounter various complications and anomalies that can negatively affect the progress of pregnancy and the health of the patient and her child. These include Couveler's uterine syndrome. It was identified by the gynecologist Kuveler, in whose honor the syndrome received this name, in 1911, and the following year it was described in his work.
Uteroplacental apoplexy, as a characteristic type of uterus, is a condition in which the placenta is rejected prematurely. In this case, the deviation is accompanied by severe bleeding with a high probability of penetration into the uterine cavity lined with muscle tissue and into the peritoneum.
This complication is dangerous not only for the mother, but also, first of all, for the baby in the womb. The fact is that the placenta plays the role of lungs, and its detachment earlier than expected causes hypoxia, as a result of which the fetus is deprived of oxygen and suffocates. In situations where Kuveler's uterus appears directly during the period of gestation of the embryo before delivery, this can threaten the woman in the situation with disability.
Pathology identified by characteristic symptoms in the early stages of development is subject to treatment. At the same time, the tactics of pregnancy change. Treatment is prescribed by a doctor, taking into account the physiological and individual characteristics of a pregnant woman. Most often, treatment of uteroplacental apoplexy involves keeping the patient under constant observation in a hospital. In this case, doctors will be able to promptly identify abnormalities and provide professional assistance.
Identification of the pathological symptom complex of Kuveler's uterus in the later stages of formation increases the risk of a retroplacental hematoma (extensive). In most cases, under such circumstances, the fetus cannot be saved, and the woman in labor may experience complications due to the large volume of lost blood. Treatment in such situations is long-term therapy under the supervision of a physician to eliminate negative consequences.
Disturbances during pregnancy when uteroplacental apoplexy occurs occur in 1 case out of 100. Knowing the symptoms of the condition and promptly seeking medical help increases the likelihood of preserving the fetus and avoids adverse consequences for the woman and her baby.