- Indications
- Contraindications
- How labor is induced in the maternity hospital
- other methods
- Measures to be taken at home
- Complications
In obstetrics, situations often arise when induction of labor is necessary. It is carried out using various methods that enhance the contractile activity of the uterine muscles and lead to the onset of spontaneous labor. This measure is carried out with the aim of delivering a newborn naturally within the next 24 hours, reducing the frequency of cesarean sections without increasing the risk of complications for the mother and child. During the period from 1990 to 2006, labor stimulation began to be performed 2 times more often.
Indications
There are the following indications for induction of labor:
- post-term pregnancy (gestational age more than 41 weeks);
- arterial hypertension that developed before or during pregnancy;
- intrauterine fetal death;
- HELLP syndrome, preeclampsia, eclampsia;
- pathology of the placenta, accompanied by oxygen deficiency of the fetus;
- placental abruption;
- maternal diseases: diabetes, kidney disease, chronic lung diseases, antiphospholipid syndrome;
- chorioamnionitis;
- fetal pathology: growth retardation, Rh conflict, oligohydramnios.
Labor activity can be induced for other reasons, for example:
- risk of rapid and precipitate labor;
- a long distance to the hospital if the woman is not hospitalized;
- danger of weak labor forces and postpartum hemorrhage in the mother.
In this case, at least one of the following criteria must be present:
- An ultrasound done at 20 weeks gestation or later confirms a current gestational age of 39 weeks or more;
- listening to fetal heart sounds during the last 30 weeks;
- 36 weeks have passed since the positive pregnancy test (blood and urine tests).
That is, before starting the procedure, it is necessary to ensure the viability of the fetus and the normal gestational age.
The scary truth about obstetric forceps
If pushing is contraindicated for a woman, then surgical delivery is prescribed: vacuum, forceps, cesarean section.
In special cases, to make it easier for the baby to pass through the mother’s birth canal, special tools are used.
This shortens the duration of the second stage of labor and reduces the risk of complications from the mother and fetus.
There are many myths that obstetric forceps compress the child’s head and provoke the development of cerebral palsy.
Obstetric forceps must be used correctly and according to indications. They can be used if the woman is unable to push the baby out or to speed up the second stage process. In addition, they can change the child’s position, reducing the risk of injury.
Currently, forceps are rarely used when the opportunity for a cesarean section is missed.
Previously, they were used to remove a dead fetus from the uterus.
The first live baby was born using forceps in 1600 in England.
Since then, the tongs have gone through many stages of improvement.
Up to 10% of births end with surgical intervention: the use of forceps or vacuum extraction.
With the help of forceps, only two actions are performed: compression and extraction.
The forceps tightly grasp the fetal head, gently and effortlessly, the expelling force of the uterus is replaced by the force of the doctor. The forceps are designed in such a way that they cannot squeeze the head too much, thereby harming the baby.
Obstetric forceps are used in the following cases:
- when the second period is delayed (more than 1-2 hours);
- in cases of quick removal of the baby (weak, non-intense attempts);
- in case of bleeding as a result of premature placental abruption;
- in cases of threat to the baby’s life (hypoxia due to a short umbilical cord, entanglement of the umbilical cord around the neck);
- when the mother cannot push (comorbidities).
The use of obstetric forceps requires certain conditions and experience of the doctor.
Contraindications
Any methods of inducing labor are prohibited in the following situations:
- placenta or umbilical cord previa;
- previous caesarean section;
- transverse position of the fetus in the uterus;
- umbilical cord prolapse;
- active herpetic genital infection;
- invasive cervical cancer;
- previous myomectomy with opening of the endometrial (inner) layer of the uterus;
- previous uterine rupture;
- severe fetal heart rhythm disturbances.
A woman should understand that if stimulation is unsuccessful, she will need a cesarean section, and the process itself takes about a day from start to finish.
How labor is induced in the maternity hospital
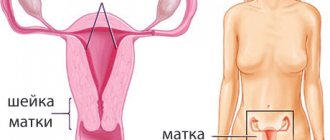
When a woman enters the prenatal department, the condition of her genital organs is assessed using the Bishop scale:
The cervix is considered not ready for labor induction when the Bishop score is 6 points or less. If labor is nevertheless induced artificially, the likelihood of a surgical completion (emergency caesarean section) increases. It is advisable to wait until the cervix meets the required parameters, and only then use stimulation methods.
If the Bishop score is more than 8, the cervix is well prepared for spontaneous or induced labor.
Cervical preparation
Artificial induction of labor begins with preparation of the cervix if the organ does not meet the norm on the Bishop scale. For this purpose, medicinal and mechanical methods are used.
Medications include the prostaglandins misoprostol (PGE1), dinoprostone - Prepidil and Cervidil (PRE2), the antigestagenic drug mifepristone (Ginestril, Miropriston, Pencrofton), as well as the hormone that directly contracts the uterus, oxytocin. In foreign practice, preference is given to prostaglandins - they are convenient to use (tablets and gel, rather than injections and infusions), they do not cause severe side effects.
Misoprostol
This is a synthetic analogue of prostaglandin E1, known as Cytotec. The drug is approved for the treatment and prevention of stomach ulcers. Induction with misoprostol is possible if there is no history of caesarean section.
The drug is available in the form of tablets of 100 and 200 mg. The tablets can be taken orally, buccally, sublingually, or vaginally. But most often, 25 mg of the drug is administered into the vagina every 3-6 hours.
How long does it take for misoprostol to work?
Contractile activity of the uterus begins in the near future, and its maximum occurs 10-16 hours after administration.
Dinoprostone
This is a prostaglandin E2 drug, available under the names:
- Prepidil: gel containing 0.5 mg of active substance in 2.5 ml of gel;
- Cervidil: vaginal suppositories or a special container system containing 10 mg of a slow-release substance (0.3 mg per hour).
Medicines are used to accelerate cervical ripening if the need to induce labor already exists or may arise in the near future.
How is the gel administered to induce labor?
Prepidil is administered every 6-12 hours up to a total dose of 1.5 mg (three injections) during the day. The Cervidil vaginal system is removed from the vagina and replaced with a new one every 12 hours.
Balloon catheterization
Using a Foley catheter to prepare the cervix for labor
This is a mechanical way of stimulating uterine contractility. It is carried out using the following devices:
- Foley catheter No. 16, into which 30-80 ml of saline is injected;
- double-balloon Cook catheter: one balloon is located intrauterinely and has a volume of 40-80 ml, the other is located in the vagina and has a volume of 20-60 ml.
A catheter for inducing labor is used in the following way:
- is installed in place using fingers or mirrors; if necessary, its position is controlled with ring-shaped forceps or ultrasound;
- can remain in the vagina for up to 12 hours;
- the balloon is filled with saline solution and placed over the internal os.
If sufficiently effective, after 12 hours the cervix will mechanically dilate so much that the catheter will be removed spontaneously. After this, an amniotomy is often performed, and if necessary, an oxytocin infusion is started.
The pros and cons of using prostaglandins and catheters are still being studied. So far, scientists have not found significant differences in the effectiveness and safety of both methods.
Mifepristone
In planned cases, labor can be stimulated with Mifepristone. This is an antigestagenic drug that increases uterine contractility. It is prescribed in tablet form - 200 mg per dose once.
How long does it take for Mifepristone to work?
The effect is assessed by the dilation of the cervix one day after administration. If labor is inactive, another tablet is prescribed. When self-opening the amniotic sac, in order to avoid a long water-free interval, the interval between taking tablets is reduced to 6-12 hours.
The final assessment of effectiveness is carried out after 2-3 days; if necessary, activation of labor is continued with prostaglandins or oxytocin.
Oxytocin
This is a synthetic analogue of the female sex hormone responsible for uterine contractility. It stimulates labor by activating receptors that cause calcium to accumulate inside the uterine cells, which increases the force of their contractions. Stimulation by oxytocin during labor also increases the production of its own prostaglandins. The drug is not administered in all cases. Usually, with a well-prepared neck, the process begins on its own. Oxytocin is prescribed for weak labor forces.
This is a less suitable method for women with an unprepared cervix, that is, with low scores on the Bishop scale. Before using oxytocin, it is necessary to use the means listed above to ripen the cervix.
The drug is administered intravenously through a drip or infusion pump until persistent uterine contractions are achieved every 2-3 minutes, that is, it is necessary for the development of contractions.
Is oxytocin dangerous?
Oxytocin (syntocinon) is a synthetic analogue of the hormone that is responsible for the contractile function of the uterus during childbirth and the secretion of breast milk.
Towards the end of pregnancy, the concentration of natural oxytocin reaches a high level.
The maximum concentration of oxytocin occurs at night, so labor often begins in the morning.
During the birth process itself, the concentration of oxytocin reaches its maximum towards the end of the second and third stages.
With the onset of contractions, natural oxytocin smoothes the muscular layer of the uterus and increases its tone. If there is a lack of natural oxytocin, contractions are weak and the birth process may be delayed or stopped. In this case, the doctor may begin stimulation with artificial oxytocin.
Indications:
- when labor is weak (the cervix opens less than 1 cm per hour, the baby does not move through the birth canal);
- in case of premature release of water, absence of contractions - to stimulate labor. A long dry period increases the risk of infection of the membranes and fetus;
- with progressive gestosis, Rh conflict - to speed up labor, provided that the cervix is ready (sufficiently open);
- in the postpartum period to prevent bleeding.
Oxytocin is administered intravenously in a certain dosage. At the same time, a CTG is performed to determine the baby’s condition and measure the strength of contractions.
It is believed that labor stimulated by synthetic oxytocin is more painful in women (contractions are more painful).
Oxytocin is administered when the cervix is short and soft, slightly dilated, and the membranes are broken.
If the drug is ineffective, the doctor may decide to perform surgery by caesarean section.
After taking oxytocin, there may be swelling and decreased urination.
There is an opinion that the administration of oxytocin has a bad effect on the baby (reducing the child’s adaptive capabilities).
Currently, doctors use oxytocin less frequently, or use a small dose or in combination with other drugs.
Oxytocin should not be used for:
- narrow pelvis;
- incorrect position of the fetus;
- complete placenta previa;
- presence of scars on the uterus;
- immature cervix;
- threat of uterine rupture.
Other methods of inducing labor
Hygroscopic (osmotic) dilators (expanders) are used - kelp and Dilapan. They are used mainly to terminate pregnancy, and not to pre-ripen the cervix. These substances are injected into the cervical canal, absorb fluid and mechanically push its walls apart. Compared to the use of prostaglandins, activation of labor in this way entails a risk of bacterial infections in the mother and newborn. In addition, the introduction of such drugs into an unprepared cervical canal is accompanied by unpleasant sensations for the patient.
Extra-amniotic administration of a sterile saline solution is carried out through a catheter inserted into the paravesical space. The method is quite effective, but without advantages over the use of a catheter or prostaglandins.
Amniotomy is the artificial rupture of the amniotic sac surrounding the fetus to induce or accelerate labor. During this procedure, it is necessary to control the flow of fluid with your hand to prevent the umbilical cord loops or parts of the fetal body from falling out.
During a manual examination, the doctor may use his fingers to expand the lower uterine segment, expose the membranes in a circular motion, and slightly separate them from the uterine wall. The procedure can be performed on an outpatient basis in women whose cervix has begun to dilate to speed up the onset of labor. Usually after this, labor begins in the next 2 days. A similar procedure is best performed for women who are 40 or 41 weeks pregnant. It is quite effective, but carries the risk of premature rupture of the membranes and infection of the fetus and uterine cavity.
Measures to take at home
Stimulation of labor at home can be carried out by mechanical irritation of the nipples. This causes a reflex contraction of the muscles of the uterus. Nipple massage should not be used on women with an unprepared cervix. This procedure is less effective than using oxytocin. Natural stimulation is best suited for patients with a prepared cervix, and labor begins within the next 72 hours.
On the recommendation of a doctor, a pregnant woman can use the drug Buscopan, suppositories with belladonna, or the well-known antispasmodic No-shpa (Drotaverine). They relax the muscles of the cervix and promote its opening.
Among the rare or even exotic methods of stimulating labor activity, the following can be noted:
- use of glucocorticoid hormones;
- using castor oil internally;
- administration of hyaluronidase, isosorbide dinitrate;
- acupuncture;
- evening primrose oil;
- herbal preparations;
- sexual intercourse;
- physical exercise.
Physical exercise
Exercises can be performed at home, preferably when precursor contractions or other signs of impending labor already appear, in order to speed up the entry of the baby’s head into the small pelvis. The following types of load are offered:
- walking in a straight line or on stairs;
- swimming;
- preferential squatting position;
- mopping the floor with a cloth;
- picking up matches or buttons scattered on the floor.
Sexual contact stimulates labor quite well. However, the partner must be absolutely healthy so that the infection does not enter the woman’s genital tract.
Why is amniotomy done?
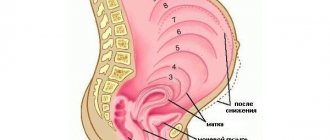
The child spends all nine months of intrauterine life in the amniotic fluid inside the membrane.
The part of the water that is located below the contact zone of the baby’s head with the mother’s pelvis is called the amniotic sac.
Normally, the bladder has a sufficient amount of water.
If there is not enough amniotic fluid (with oligohydramnios, a narrow pelvis), the bladder is called flat: the lower membrane of the bladder is adjacent to the fetal head.
Amniotomy is the opening of the amniotic sac.
A special long hook (amniotome) is used to hook the membrane of the bladder and tear it.
The procedure is painless, but unpleasant.
Apply:
- to stimulate labor;
- during childbirth to speed up labor (cervical dilatation 4-5 cm).
After the puncture, the water is released, the baby’s head drops and puts pressure on the internal os of the uterus, causing increased labor.
Possible complications:
- infection of the membranes, mother, fetus;
- injury to the baby with an amniotomy;
- loss of umbilical cord loops;
- fetal hypoxia.
Amniotomy can be:
- premature: to induce labor;
- early: with regular contractions and cervical dilatation up to 7 cm;
- timely: to accelerate the dilation of the cervix up to 10 cm;
- delayed: the amniotic sac has not opened during normal labor, full dilatation of the cervix, and lowering of the head into the pelvis.
Amniotomy can be prescribed according to indications (from the onset of labor to 6-7 cm of cervical dilatation) in the following cases:
- polyhydramnios - as a result of this, the uterus is overstretched, which leads to weakness of labor;
- weak labor activity due to various diseases (metabolic disorders, endocrine system disorders, obesity, thyroid diseases, abortions, inflammatory diseases of the genitourinary system, late age). Contractions do not intensify, on the contrary, they become less effective, and the cervix does not dilate;
- insufficient amount of water in front of the baby’s head, the membranes are in a tense state, which inhibits labor;
- diseases of the cardiovascular system, gestosis, high blood pressure;
- low location of the placenta as a result of pressing the edge of the placenta with the baby’s head;
- fetal hypoxia;
- Rhesus conflict pregnancy;
- post-term pregnancy;
- fetal death;
- exhaustion of the woman in labor after long contractions;
- flat amniotic sac.
Contraindications:
- placenta previa;
- presentation of umbilical cord loops;
- abnormal position of the fetus;
- presence of contraindications to natural childbirth.
Amniotomy can also be performed at the end of the first period, after the bladder has completed all its functions and its further creation can lead to complications (premature placental abruption).
Amniotic fluid is normally clear and odorless and is secreted until birth.