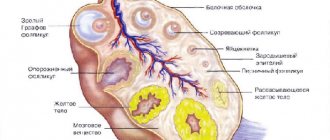
Some women believe that the ovaries play a purely reproductive role. Indeed, this paired organ is a kind of storage of eggs, which in some way are still unconceived children. But the list of functions of this reproductive organ is not limited to this.
The ovaries are involved in the production of a huge amount of steroid sex hormones, which determine many processes in our body.
Hormonal levels have a key influence on the general health of all systems, as well as on the psycho-emotional state of women. We also owe our grace, sophistication and beauty to estrogens. However, there are situations in which the only salvation for the patient is removal of the ovaries.
This operation is inevitable in some cases, for example, with breast cancer or dangerous diseases such as polycystic ovary syndrome or cyst rupture.
Some inflammatory diseases affecting the pelvic organs lead to irreversible pathologies in the tissues, which also entails oophorectomy.
When is an oophorectomy necessary?
Ovariectomy refers to a surgical procedure during which a paired organ is removed. The operation involves general anesthesia and preliminary hospitalization of the woman. Sometimes the ovary and tube are removed.
Ovariectomy is recommended for large endometriotic cysts that interfere with the functioning of the ovary. Often this intervention is indicated for menopausal women. However, if oncology is suspected, for some types of cysts it is possible to remove the ovary during reproductive age.
Indications
Removal of the ovaries in women of the childbearing cycle causes significant hormonal changes, since the organ produces hormones necessary for the functioning of the female body. Ovariectomy at a young age leads to the need to take hormonal drugs (as part of HRT).
General indications for oophorectomy include:
- premenopausal and menopausal age (45-50 years),
- predisposition to the development of hereditary malignant tumors.
Bilateral oophorectomy is prescribed in the following cases:
- ovarian cysts in combination with fibroids,
- oncological processes of the reproductive organs,
- adenomyosis and endometrioid cysts,
- purulent pathologies in the appendage area.
Unilateral removal is indicated for the following pathologies:
- inability to remove an ovarian cyst without damaging organ tissue,
- malignant tumor,
- severe inflammatory process, accompanied by a risk of necrosis or sepsis,
- advanced stage of PCOS,
- intense pain syndrome,
- ectopic pregnancy,
- extensive endometriosis,
- apoplexy,
- organ torsion.
Removal of the ovary along with the tube is recommended for these diseases:
- threat or rupture of a pipe,
- neoplasms of unknown etiology,
- ectopic pregnancy,
- adhesive process,
- complications that developed as a result of adnexitis,
- obstruction of pipes.
The extent of surgical intervention depends on the specific clinical situation.
Possible complications
Side effects of this safe procedure are minimized. However, in addition to the appearance of pathological discharge, a woman may experience other symptoms:
- temperature increase;
- general weakness and fatigue;
- loss of consciousness;
- decreased appetite;
- bloating;
- frequent urge to empty the bladder;
- nausea, even vomiting;
- increased pain in the abdomen;
- swelling and hyperemia of suture areas;
- bleeding from wounds;
- pneumonia;
- stroke.
To relieve pain, painkillers are prescribed; medications containing Simethicone can eliminate flatulence. At the end of all the above information, I would like to add that in order to avoid all the unpleasant manifestations of the postoperative period, the patient must follow all the recommendations of the attending physician. In addition, approach the choice of a medical institution and specialist who will perform laparoscopy with all responsibility. And if all the rules of the rehabilitation period are followed, the woman will quickly return to her previous shape and active life without consequences for her health.
“>
Contraindications
The operation is not always advisable. In some cases, there are contraindications to oophorectomy:
- serious pathologies of the cardiovascular system,
- bleeding disorders,
- renal or liver failure,
- hemorrhagic shock,
- peritonitis,
- pregnancy 2-3 trimesters,
- pronounced adhesions,
- obesity (stage 3-4),
- intense intra-abdominal bleeding,
- intolerance to anesthesia,
- poor regenerative processes.
For urgent interventions, the list of contraindications is much smaller. This is due to a threat to the life and health of the patient.
Preparing for surgery
Preparation for surgery is not much different from that for other types of interventions. When the question of the feasibility of resection has been decided, the patient will have to undergo the necessary preoperative studies:
- Take a general blood and urine test, a biochemical blood test, and possibly blood tests for sex hormones and tumor marker CA-125;
- Undergo a blood clotting test (coagulogram);
- Be screened for infections (HIV, hepatitis, syphilis, sexually transmitted diseases);
- Visit a gynecologist to take a smear from the vagina and cervical canal;
- Perform an ultrasound of the pelvic organs;
- Undergo fluorography and, if indicated, an ECG.
Emergency operations involve a minimum of studies, which begin in the emergency room from the moment the patient is admitted and include general clinical blood and urine tests, a coagulogram, ultrasound of the pelvic organs, and examination by a surgeon to exclude acute surgical pathology of the abdominal cavity.
When all the necessary diagnostic procedures have been completed before the planned resection, the woman goes to the therapist, and he, based on the presence or absence of concomitant diseases, gives his permission to perform the operation. All concomitant pathology must be cured as much as possible or brought to such a state that the intervention becomes safe.
If you need to take any medications on a regular basis, you must inform your doctor about this. Before surgery, anticoagulants and other drugs that cause blood thinning are discontinued. Diabetes may require a switch to insulin, even if the patient is quite helped by glucose-lowering pills. When all risks have been excluded, the gynecologist sets a date for arrival at the hospital with the results of all examinations completed.
On the eve of the operation, the woman is advised to refrain from eating large meals, to exclude all those foods that will cause gas formation or fecal retention (chocolate, legumes, cabbage, baked goods, etc.). 12 hours before the intervention, food and water are taken for the last time; if any medications need to be taken, the woman discusses this point with her doctor.
In the evening before the resection, you need to take a shower and change clothes, the pubic area and lower abdomen are shaved during the planned laparotomy. If there are problems with stool, a cleansing enema will be offered. This is not only a measure to facilitate the operation, but also the prevention of postoperative complications, in particular constipation. In case of severe anxiety, sedatives or mild sleeping pills are prescribed at night.
Types and performance of oophorectomy
There are several options for surgery to remove the ovaries:
- One-sided. The intervention is indicated for malignant tumors, serious infectious processes, and cysts.
- Double-sided. This operation is recommended for organ damage by endometriosis, infectious processes, and oncology in the pelvis.
- Salpingo-oophorectomy. The term implies removal of the ovaries and tubes. Usually, removal of appendages is advisable in case of damage to the tubes or their obstruction.
Bilateral removal of the ovaries can be combined with hysterectomy, which involves amputation of the cervix and uterine body.
The duration of the intervention is 2-4 hours. Ovariectomy can be performed in two ways:
- Laparotomy method. This is an abdominal operation, which is performed using a traditional incision on the abdominal wall (vertical, horizontal). A horizontal cut leaves virtually no traces. However, a vertical incision provides good access for visualization of internal organs.
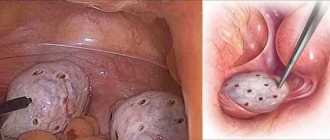
- Laparoscopic method. During the intervention, the doctor makes incisions in the abdomen to place instruments. This is a gentle option that allows you to reduce the recovery period and postoperative risks.
Most operations are performed through laparoscopic access.
Before oophorectomy, the patient undergoes an examination, including:
- UAC,
- OAM,
- blood for biochemistry,
- smear on flora,
- determination of hormonal levels, sexually transmitted infections,
- Rh factor,
- blood type,
- ultrasound examination of organs located in the pelvic area,
- colposcopy for cervical pathologies,
- consultation with a therapist (fluorography, ECG).
A few days before the intervention, you must refrain from taking medications not prescribed by a doctor, drinking alcoholic beverages, and smoking. A woman should include foods rich in vitamins and minerals in her diet.
The patient is hospitalized in the hospital one day before the oophorectomy. The operation is performed strictly on an empty stomach. Before the intervention, it is necessary to take a hygienic shower, remove hair in the pubic area, groin, and abdomen.
Carrying out an oophorectomy involves performing a cleansing enema.
Bed rest after surgery is prescribed for at least a day. For intense pain, painkillers are recommended. Then the woman is allowed to get up and move carefully. Moderate physical activity normalizes the functioning of the intestines.
Discharge takes place a few days after oophorectomy, and the sutures are removed on days 8-14. You cannot be sexually active for 2 months. Physical activity should not be intense.
Types of surgical intervention and indications for them
The operation to remove the ovary can be performed either laparoscopically or laparotomically. The choice of technique depends on the reason for the intervention. If we are talking about a malignant neoplasm, abdominal removal surgery is often performed, since it is often necessary to undergo extirpation (removal of the uterus and appendages).
In the case of twisting of the ovarian pedicle, apoplexy, rupture of the cyst, or simply its progressive growth, gynecologists more often use gentle laparoscopic techniques. Ectopic pregnancy is also a reason for laparotomy access.
Features of partial resection of the ovary
This procedure involves partial excision of damaged ovarian tissue. The operation can be performed abdominally or laparoscopically. The main indications are pathological processes in which only a certain anatomical area of a given organ is involved. Most often this is polycystic ovary syndrome.
Such a surgical intervention in the laparoscopic version is a minimally invasive procedure. Compared to how long rehabilitation takes after removal of the ovary, a day in hospital after the intervention is a good result. A high safety profile and a low risk of adhesive disease are all advantages of this modern technique. The only disadvantage is the high cost of the operation.
What is wedge resection of the ovary
Wedge resection is a basic organ-sparing operation for polycystic ovary syndrome. Its essence is to perform a laparoscopic approach and excise part of the ovarian capsule with a small area of tissue of the organ itself. The purpose of the invasion is to create the opportunity for a mature egg to leave the ovary for fertilization.
Since recovery after abdominal surgery is accompanied by possible inconvenience in the selection of hormonal drugs, the development of adhesions and a long early postoperative process, doctors prefer wedge resection as a quick way to solve the problem of infertility in patients with polycystic ovaries.
Ovariectomy – complete removal of the ovary
Removal of the ovary is indicated for patients with a high degree of damage to the function or structure of this organ, an episode of ectopic pregnancy with a risk of hemorrhage, or ovarian apoplexy. In all these cases, the threat to the patient’s life is extremely high, and therefore doctors perform radical surgery. Having chosen the access option, surgeons excise the ovary, suturing the end of the broad uterine ligament to the defect.
Rehabilitation after abdominal surgery to remove the ovary is accompanied by a week of ward stay in a gynecological hospital, taking antibiotics and high doses of female sex hormones. Hormonal drugs are taken for a long time, and their dosage is revised in the event of menopause.
Most experts are inclined to believe that any ovarian tumor is an indication for its removal, since the nature of the tumor can only be reliably assessed after a histological analysis
Consequences of surgery to remove the ovary
If oophorectomy was performed after the onset of menopause, no serious consequences are noted, since hormonal changes have already occurred. Removing the ovaries after 40 years has the following consequences:
- bleeding,
- thrombosis,
- psycho-emotional disorders,
- decreased sexual desire (libido),
- frequent urination,
- headaches (migraines),
- cardiovascular pathologies,
- osteoporosis,
- hypertension,
- atherosclerosis,
- weight gain,
- premature aging,
- vaginal prolapse,
- adhesive process,
- peritonitis.
Depression
Depression is caused by both physiological and psychological reasons. Hormonal levels influence the appearance of emotional lability, irritability, and nervousness. Women may experience inadequacy, which leads to the development of severe depression.
Hormonal disorders
After removal of the ovaries, there is a drop in estrogen levels and an increase in the secretion of gonadotropins (FSH and LH). Androgen production also decreases. In 60% of cases, the syndrome has a severe course, which is manifested by various disorders.
Consequences of ovary removal after 50 years
Most women over the age of 50 are in menopause. This means that serious long-term consequences are minimized. Adaptation of the body to functioning without sex hormones usually begins after 45 years. It is in this age group that surgical interventions for oophorectomy are most often recorded.
Effect on the heart and blood vessels
The cardiovascular system depends on the level of sex hormones. After bilateral oophorectomy, headaches, heart pain, and pressure changes are observed.
Condition of the genital area
Ovariectomy leads to a decrease or complete cessation of the production of sex hormones (bilateral version) produced by the ovaries. Thus, menopausal symptoms develop, affecting the genital area. A woman notes a decrease in libido, dryness in the vagina, which prevents her from having a full sex life. When one ovary is removed, the hormonal levels are partially preserved.
Duration and features of the recovery period
The recovery period depends on the volume of intervention. The age of the patient is essential. Complete rehabilitation of the body usually takes 1.5-2 months. Recovery after removal of the ovary and tube has the same duration. During this time, the woman observes a protective regime, which involves a gentle diet, limited physical activity and the exclusion of sexual activity.
During the first 24 hours, pain and bleeding may occur. And weakness and nausea are also noted. After a few days, the patient's condition returns to normal.
Early postoperative complications
Surgical complications in the early period include damage to internal organs, which often occurs during laparotomy. Bleeding is possible, which is less treatable by laparoscopy.
If the rules of asepsis are not followed, an infection may develop and peritonitis may develop. To prevent these complications, antibiotic therapy is prescribed.
Late postoperative complications
When an ovary is removed, the consequences and condition of the body depend on many factors. Long-term consequences develop due to a sharp cessation of the production of sex hormones. First of all, disorders of the cardiovascular, musculoskeletal and nervous systems are observed. Psycho-emotional disorders are registered.
The essence of surgery
If a laparoscopic technique is chosen, holes are made in the patient’s abdominal cavity, with the help of which manipulators are inserted into it, after which the necessary areas are resected and sutured. With a laparotomy approach, the surgeon cuts through the anterior abdominal wall, gains access to the ovary and the ligament that holds it, and then fixes the uterine ligament.
The rehabilitation period after removal of the ovaries depends on the surgical technique. In the case of laparoscopy, the patient leaves the hospital within 24 hours. After the laparotomy operation, she remains in the hospital for a week.
Consequences of oophorectomy
Having lost the sources of production of sex hormones, a woman needs their immediate artificial supply in the form of medications. In the early stages, it is not always possible to properly select the required dose, so the patient may feel general malaise, tremors, or, conversely, lethargy. In addition, blood pressure problems and sleep disorders may occur. The patient may also experience endocrine disorders, including hirsutism (excessive growth of unwanted hair) and dysmenorrhea (pain during menstruation).
The main condition for achieving a high quality of life in patients who have undergone ovarian removal is constant monitoring of the doses of steroids used and treatment of concomitant pathological conditions, the course of which can be aggravated as a result of changes in hormonal levels
Treatment after surgery
The scope of treatment depends on the specific situation. All patients are prescribed prophylactic antibacterial drugs to prevent infection and sepsis. NSAIDs are recommended to eliminate pain.
In case of oophorectomy during reproductive age, it is necessary to take hormonal therapy, which is of a replacement nature. Hormonal medications support endocrine function due to ovarian loss.
Life without ovaries
Hormonal treatment is usually recommended after bilateral oophorectomy, especially in patients who have not reached menopause. This is due to a sharp drop in the level of sex hormones, which negatively affects the functioning of internal organs. Taking HRT allows the patient to lead a normal life, including intimate ones.
Life with one ovary
Removal of the right ovary, for example, is easier for a woman to tolerate than a bilateral oophorectomy. That is why such operations are more preferable. The hormonal balance is maintained by the remaining organ. If the left ovary and tube are removed, the consequences are a decrease in reproductive function. The issue of postoperative therapy (hormonal) is decided on an individual basis.
Life after hysterectomy
Features of the postoperative period after removal of the appendages and uterus depend on the age of the patient. Many women perceive the uterus as a sign of femininity. Accordingly, the loss of an organ can be psychologically difficult. To prevent unpleasant consequences, appropriate therapy is prescribed.
What diseases can cause specific discharge
Vaginal discharge is detected during genitourinary infection, which was not cured in time, or the course of which was chronic. It could be:
- mycoplasmosis;
- ureaplasma;
- chlamydia;
- trichomoniasis;
- other infections.
The presence of bacteria causes itching and burning. But their occurrence after removal of non-infected appendages may be associated with a weakening of the body’s general immunity. They are not always specific: for example, with trichomoniasis they are gray and foamy. If they smell fishy, it's a bacterial infection. Such discharge is rare, because after the removal of one or two appendages, antibiotics are prescribed, and they prevent the development of bacteria.
Another thing is thrush, candidiasis. It occurs after removal of the uterine appendages, when antibiotics are prescribed, and in this case white discharge appears. Some describe them as cheesy.
If the removal of the appendages is performed on both sides, the woman should have no discharge after the operation, except for brown, spotting discharge. This is due to the fact that the lack of hormones causes menopause, which is usually accompanied by dry mucous membranes. If strange discharge appears at this time, this indicates an infectious lesion in the body or a complication.
Color, smell, consistency, and other characteristics of discharge can tell a lot about their etiology. If discharge appears after removal of the appendages, you need to contact your treating gynecologist to provide adequate treatment.
Today, the medical industry has fundamentally new technologies for surgical interventions. One of these achievements of modern science is laparoscopy - a safe, low-traumatic and short-term operation that does not require a long recovery period. Laparoscopic interventions are carried out using probes that are equipped with a camera and special lighting that allows you to examine all the details of the operated area. They are inserted through small (no more than two centimeters) incisions on the skin.
This surgical technique is widely used in gynecology - after such an operation there are no noticeable cosmetic defects left on the skin of the abdomen, moreover, rehabilitation proceeds quickly and without any serious complications. In some cases, after laparoscopy, women note the appearance of discharge - this can be either a natural phenomenon or a sign of a pathological process.
In our article we want to talk about the specifics of laparoscopic surgery, the rules of preparation for the procedure, the characteristics of the rehabilitation period of the female body and explain whether brown discharge after laparoscopy is a pathology.
Sex after removal of appendages
Usually, oophorectomy does not lead to disturbances in intimate life. Sexual relations are permitted in the absence of complications after 7-10 weeks. As a rule, there is no physical discomfort after the intervention.
However, changes in hormonal levels, if bilateral removal was performed, can lead to decreased libido, vaginal dryness, and depression. These factors adversely affect the quality of intimate life. In such cases, hormonal therapy is recommended, including in the form of ointments for topical use. In case of psychological disorders, a woman can turn to a psychologist or sexologist.
Methods of ovarian resection
As a rule, resection of the left or right ovary is performed under general anesthesia, which largely determines the importance of preoperative preparation and attention to the general condition of the woman. In some cases, local anesthesia can be used (if there are contraindications to anesthesia, allergies to certain drugs, etc.).
ovarian resection
The operation can be unilateral or resection of both ovaries is performed. The need for bilateral intervention is dictated by diagnosed polycystic disease or neoplasms or cysts on both sides at once.
Removal of the ovarian fragment can be performed laparoscopically and by standard laparotomy. Laparotomy was until recently the main method of access to the pelvic organs, but today it is confidently being replaced by laparoscopy, which has a number of significant advantages:
- Minor tissue trauma;
- Faster recovery and easier course of the postoperative period, which shortens the period of disability to a minimum;
- Excellent cosmetic result;
- Lower incidence of complications after intervention.
Laparotomy access is mainly used for emergency interventions, when there is no time for adequate preparation and examination of the pelvis. In addition, in such situations, the nearest hospital may not have the necessary equipment or trained specialist. If there is a strong adhesive process in the pelvis, laparoscopy is completely contraindicated, so the gynecologist has no choice - the operation is performed through open access through a wide skin incision.
After processing the surgical field, the surgeon begins to perform the stages of the operation:
- An incision in the suprapubic area in the transverse direction or along the midline of the abdomen, going from top to bottom;
- Penetration into the pelvis, examination of the appendages, isolation of the ovary, dissection of adhesions if present;
- Applying a clamp to the ovarian pedicle carrying the feeding arteries;
- Economical excision of damaged parenchyma with maximum preservation of healthy tissue;
- Suturing the ovarian wound with absorbable threads, stopping bleeding and ligating blood vessels;
- Inspection of the abdominal cavity for bleeding, unligated vessels;
- Suturing the skin wound in the reverse order.
Suprapubic laparotomy is more cosmetic and is indicated for small ovarian masses; midline laparotomy is used for large cysts or tumors. If a purulent focus is found in the ovary, then rinse with chlorhexidine solution and install drainage tubes to drain the discharge. Drainage is also indicated for inflammation in the pelvis or abdominal cavity.
Wedge resection of the ovary involves excision of its part in the form of a wedge, with its base facing the periphery (capsule) of the organ. In this case, the surgeon dissects the parenchyma deeply in the direction of the ovarian gates, but without reaching them, so as not to cause circulatory problems in the remaining part of the organ. The resulting defect is sutured using thin needles so as not to injure the very fragile tissue. The threads should not be tightened too tightly as this may cause them to break through with the risk of complications. Bleeding vessels are bandaged.
wedge resection of the ovary
Resection of an ovarian cyst can be performed through a similar approach. After removing it into the wound, the cyst is delimited using a napkin. The ovarian incision is made at the border between the cystic cavity and healthy parenchyma, carefully so as not to damage the tissue. The cyst is separated from the ovary without much effort, and the thin bridge that connects it to the organ is crossed.
When resecting a cyst, it is important to act extremely carefully, since a large cavity can push the ovarian tissue to the periphery and make it look like a thin plate, and then there is a risk of removing such a changed, but still functioning, organ simultaneously with a pathological formation.
After excision of the cyst, the integrity of the remaining fragment of the ovary is restored, sutures are placed on the vessels, the pelvic cavity is examined and the abdominal wall is sutured in the same way as with wedge resection.
Resection of the ovary for polycystic disease is one of the main methods of treating the pathology, since conservative therapy does not always bring at least some effect. The operation is performed on two ovaries at once, removing at least two-thirds of each organ. Its technique does not differ from that of wedge resection.
The purpose of surgical treatment of polycystic disease is to remove sclerotic tissue and follicles “walled up” in them and, thereby, provoke normal maturation of eggs. This method allows you to achieve ovulation and conception in case of infertility due to polycystic disease, as well as normalize a woman’s hormonal levels.
Laparoscopic resection of the left ovary or a fragment of the right ovary takes approximately the same time as open surgery, and also requires general anesthesia. The main difference between laparoscopy and laparotomy is the absence of a large incision and scar in the future, that is, a very good cosmetic result, which is achieved through the use of special instruments.
Preparation for laparoscopy is the same as for open surgery, but the patient pays special attention to the condition of the intestines and its careful emptying. Filled intestinal loops during laparoscopy can complicate the process of pumping gas into the abdominal cavity and impair the surgeon's visibility.
After placing the patient under anesthesia, the surgeon makes three small incisions (about 2 cm) in the anterior abdominal wall, through which he inserts instruments, a video camera, and a light source into the abdomen. To improve visibility and raise the abdominal wall, carbon dioxide is injected into its cavity.
laparoscopic ovarian resection
Dissection of the ovarian parenchyma and removal of the fragment is performed using an electrocoagulator, through which a high-frequency electric current flows. The coagulator does not damage the surrounding tissue, but “cuts” the area where the surgeon directs its action. In addition, the high temperature created in the area of action of the coagulator promotes sealing of the lumens of small vessels, minimizing the risk of bleeding.
After the desired section of the ovary is cut off, the surgeon removes it and examines the pelvic area using a video camera for bleeding or other pathological changes. If everything is in order, the instruments are removed and the small skin incisions are sutured.
Reviews
Ovariectomy has a significant impact on the condition of the female body. Removal of the ovaries after 60 years has less pronounced consequences, as evidenced by patient reviews. However, one should not refuse surgical intervention if necessary, despite conflicting reviews. Sometimes removing the ovaries for breast cancer helps stop the progression of the tumor. Unilateral oophorectomy allows partial maintenance of hormonal levels. Otherwise, the woman is prescribed medications to prevent the development of unpleasant symptoms.
Radiation therapy (radiotherapy)
Controlled doses of radiation are directed at the tumor to kill cancer cells. Typically, radiation therapy is used after surgery, as well as chemotherapy to kill surviving cancer cells. Typically, radiation therapy occurs about a month after surgery or chemotherapy. The session takes a few minutes, and the patient may require three to five sessions per week for three to six weeks. The woman will need to decide what type of radiation therapy she can have. In some cases, radiation therapy is not needed.
Types of radiation therapy include:
- Radiation therapy to the breast after lumpectomy, radiation is injected into the remaining breast tissue.
- Radiation therapy to the chest wall - this is used after a mastectomy.
- Breast Augmentation - High dose radiation therapy is used where the tumor has been surgically removed. The appearance of the breasts may change, especially if the patient has large breasts.
- Radiation therapy of lymph nodes.