The group of ToRCH infections includes diseases whose infection during pregnancy poses a serious threat to the fetus and the health of the unborn child.
The abbreviation ToRCH is made up of the first letters of the names of the diseases:
- toxoplasmosis ( Toxoplasmosis
); - rubella ( Rubella
); - cytomegalovirus ( C
ytomegalovirus); - herpes ( Herpes
).
All ToRCH infections are widespread. You can get these diseases regardless of gender and age. These are completely different diseases. Their separation into a separate group is due to only one thing: primary infection of any of the ToRCH infections during pregnancy can lead to fetal death or make the unborn child disabled. Therefore, gynecologists pay special attention to them, and a woman planning a pregnancy must find out whether she is infected with the causative agents of these diseases or not - her further actions will depend on this.
To do this, it is necessary to undergo screening for ToRCH infections, that is, take tests to identify the causative agents of these diseases.
Toxoplasmosis (To in the abbreviation ToRCH infection)
Toxoplasmosis is a disease caused by an intracellular parasite, Toxoplasma.
Toxoplasma lives and multiplies in the body of a domestic cat. Together with cat feces, it ends up in the external environment, where it can persist for months. This leads to Toxoplasma infection of other species of animals and birds. Toxoplasma enters their muscle tissue and thus ends up in the meat that humans consume. Proper cooking kills Toxoplasma, but if the meat is poorly cooked or undercooked, Toxoplasma will persist.
Another way to become infected with Toxoplasma is through dirty hands. Therefore, toxoplasmosis is usually encountered in childhood.
If everything is fine with your immune system, you can get toxoplasmosis and not even know it. This is usually how it happens: the primary infection occurs without obvious symptoms. It is believed that in Russia, latent toxoplasmosis occurs in 30% of the population. Toxoplasmosis is not transmitted from person to person.
Toxoplasmosis poses a danger mainly to the fetus. If the primary infection occurs during pregnancy, the fetus may die, or the child will be born sick - with damage to the liver, spleen, lymph nodes and central nervous system.
Transmission routes
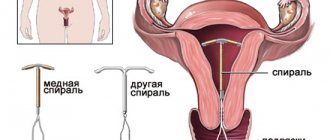
The placenta protects the unborn baby from negative influences. However, bacteria and viruses are able to penetrate this barrier. Most often, TORCH infections are transmitted transplacentally. This method of spread is characteristic of all viruses, as well as Listeria, Treponema pallidum (the causative agent of syphilis). toxoplasma
The causative agent of gonorrhea (gonococcus) is usually spread by an ascending route. First, this microorganism infects the amniotic fluid, and then the embryo becomes infected from it.
Infection of a child can occur at birth. This route of transmission is typical for chlamydia, ureaplasma, herpes virus and human papilloma (HPV). In very rare cases, a hematogenous route of transmission is possible, when the infection enters the embryo through the bloodstream from a source in the woman’s body.
Rubella (R for ToRCH infection)
Rubella is transmitted from person to person, usually through airborne droplets. The main manifestations of rubella are a small pink rash all over the body and an increase in temperature up to 38 ° C (observed more often in adults).
Rubella is most often contracted in childhood; it is a classic “childhood” infection. In childhood, the disease is usually easily tolerated. In adults, rubella is usually much more severe.
Rubella is dangerous for the fetus, especially in the first trimester of pregnancy. It affects the nervous tissue, eye tissue, and heart of the child and can lead to his death. In late pregnancy, the danger is much less.
Rubella is insidious in its own way. A person who has rubella may not yet have any symptoms (external manifestations) of the disease, but he is already contagious. Therefore, it cannot be guaranteed that you will be able to protect yourself from rubella simply by avoiding contact with those who are already obviously sick with the disease.
More about rubella>>>
Toxoplasmosis
Toxoplasmosis is a parasitic pathology caused by protozoan microorganisms. A woman can become infected with this disease from animals (most often from cats) or from eating undercooked meat. A pregnant woman's temperature rises, weakness, aching joints, general malaise, and enlarged lymph nodes appear.
If the mother is sick, the fetus becomes infected in about a third of cases. Toxoplasma is an intracellular parasite and easily penetrates the placenta. The unborn child develops damage to the brain, eyes, heart and liver. If the infection occurs in the early stages of pregnancy, the fetus most often dies and a miscarriage occurs.
When the embryo is infected in the later stages, the damage is not so pronounced. However, the disease can affect the baby's health several years after birth. This is expressed in endocrine disorders, deterioration of hearing and vision in the baby.
If a woman has had toxoplasmosis more than 6 months before pregnancy, then this will not affect the body of the unborn child.
Cytomegalovirus (C in abbreviation for ToRCH infection)
Cytomegalovirus was discovered only in the 20th century. The infection is transmitted sexually, with blood, through saliva (for example, through kissing), and also from mother to child during breastfeeding. It is currently believed that about 80% of women of childbearing age are carriers of this infection.
In most cases, cytomegalovirus is in a “dormant” state. Sometimes the infection appears as a common cold, but more often there are no symptoms of the disease. And only with a significant decrease in immunity does the threat of the disease progress to an acute form arise.
The greatest danger to the fetus is primary infection with cytomegalovirus. It is especially dangerous to become infected in the first trimester. This can lead to underdevelopment or hydrocele of the child's brain, jaundice, enlargement of the liver and spleen, the development of heart defects and congenital deformities.
What kind of infections are these?
The word TORCH is an abbreviation of English words that refer to various diseases:
- T (toxoplasmosis) - toxoplasmosis;
- O (other) - other infections;
- R (rubeola) - rubella;
- C (cytomegalia) - cytomegaly;
- H (herpes) - herpes.
In addition, the word torch translated from English means “torch,” which emphasizes the danger of these diseases.
The group “other infections” includes diseases such as chlamydia, syphilis, gonorrhea, listeriosis, hepatitis, influenza, chicken pox, papillomatosis, as well as pathologies caused by enteroviruses.
Herpes (H in abbreviation for ToRCH infection)
Today, several types of herpes virus are known. The most common types are herpes type I and herpes type II. Type I herpes manifests itself as a “cold on the lip” - in the form of characteristic rashes on the face and oral mucosa. Herpes type II is genital herpes, which is characterized by rashes on the genitals.
Herpes is transmitted in various ways, including household (through direct contact), airborne droplets, etc. However, herpes is typically transmitted through sexual contact.
According to some estimates, herpes occurs in 90% of the world's population. The virus can remain in a latent (“sleeping”) state for years, appearing only during periods of weakened immunity.
Primary infection with herpes during pregnancy is very dangerous for the fetus: in the early stages, the infection can lead to miscarriage; in the second half of pregnancy, it can cause congenital anomalies such as microcephaly, retinal pathology, and heart defects.
More about herpes>>>
Cytomegaly
If a woman becomes infected with cytomegalovirus during pregnancy, this can have extremely dangerous consequences for the fetus. The causative agent of the disease easily penetrates the placenta. An infected embryo may develop severe damage to the central nervous system and liver. Often such children suffer from deafness and delayed psychomotor development. They are born with congenital cytomegaly. The mortality rate for this form of the disease can reach 30%.
Often the consequences of intrauterine infection affect the child only at the age of 3-4 years. The baby begins to lag behind in development, his hearing and vision deteriorate sharply.
However, if a woman becomes infected with cytomegaly before pregnancy, the disease usually does not affect the health of the unborn child.
ToRCH infections and pregnancy: how to gain confidence and safety?
You should start taking care of protecting your unborn child from ToRCH infections at the stage of pregnancy planning. First of all, you should get diagnosed with ToRCH infections and find out whether you have already been infected or not.
If antibodies to any ToRCH infection are detected in your blood, this means that your body has already fought this disease and developed specific immunity to it.
If you have already had toxoplasmosis or rubella (the body contains antibodies to the causative agents of these diseases), you are not at risk of getting sick again.
If antibodies to Toxoplasma are not detected, you will need to be extra vigilant: you will need to carefully observe the rules of hygiene, make sure that the meat you are going to eat has undergone proper heat treatment, and stay away from cats.
If you do not have antibodies to rubella, you may be advised to get vaccinated. The rubella vaccine provides long-term immunity (up to 20 years). However, if you are already pregnant, you cannot get the vaccine.
If tests have shown that cytomegalovirus or herpes virus is present in the body, but they are in a “dormant” state, there is no direct threat to the unborn child. If you are a carrier of these infections and are carrying a child, you, first of all, need to take care of maintaining and strengthening the immune system, which will help avoid exacerbations of the disease. If an exacerbation does occur, treatment with antiviral drugs and immunomodulators is prescribed.
The absence of antibodies to cytomegalovirus and herpes virus means that primary infection is possible during pregnancy, which means that during this period you need to be especially careful about your health and contacts with other people.
Risk of infection and pathogenesis
TORCH infections in pregnant women can be mild or asymptomatic. However, in any case, they are very easily transmitted to the fetus. This is due to the following factors:
- Many bacteria and viruses are specifically directed against embryonic tissues.
- In the body of a human embryo, metabolism is accelerated, so its cells become a favorable environment for the development of microorganisms.
TORCH infections can have different development mechanisms. This depends on the severity of the symptoms of the pathology in the expectant mother, the form of the disease, as well as the duration of pregnancy.
If the fetus is infected from 1 to 8 weeks of pregnancy, then embryo death, miscarriage, and the formation of various developmental anomalies or fetoplacental insufficiency are possible.
Infection during 9-28 weeks of intrauterine development leads to disruption of organ formation. Hydronephrosis (enlargement and atrophy of the kidneys) or hydrocephalus (water on the brain) may occur.
At later stages of development, the fetus begins to develop immune defenses against pathogens. However, even during this period, infection of the embryo can lead to negative consequences. The baby may be born premature, with low birth weight and signs of infection.
Methods for diagnosing ToRCH infections
To diagnose ToRCH infections, you can contact Family Doctor JSC. The most convenient form of diagnosis is the laboratory profile “Diagnostics of the ToRCH infection complex,” which includes serological tests to detect antibodies to all pathogens included in the ToRCH infection complex.
Avidity tests will determine how long a particular infection has been present in the body.
Gynecologists at the Family Doctor will advise you on test results and give recommendations on how to ensure the safety of the fetus, carry and give birth to a healthy child.
Serological blood test
Serological analysis allows you to identify antibodies to the causative agent of a specific disease. In order to ensure the absence of ToRCH infections, it is necessary to conduct tests for antibodies to each of the four diseases included in this group.
More information about the diagnostic method
Determination of avidity to antibodies of ToRCH pathogens
The most dangerous infection with ToRCH infections is directly during pregnancy. ToRCH infections are widespread, therefore, if the presence of the corresponding antibodies in the blood is detected, this does not mean that the infection occurred during pregnancy. In order to find out whether there was an infection during this period, avidity is determined (an assessment of the strength of the bond between antibody and antigen). At the beginning of the disease, this connection is rather weak. Over time, the immune system produces antibodies with higher avidity. Therefore, the detection of low-avidity antibodies may indicate a relatively recent infection.
Sign up for diagnostics To accurately diagnose the disease, make an appointment with specialists from the Family Doctor network.
Rate how useful the material was
thank you for rating
Analysis transcript
How long does it take to test for TORCH infections? This depends on the clinical laboratory in which the study is performed. On average, processing of test results takes 1-2 days.
In the transcript of the analysis for TORCH infections, the first column of the table lists the types of pathogens. The second column indicates whether IgG class antibodies are detected, and the third column indicates whether IgM immunoglobulins are detected.
If class G and M antibodies are not detected in the blood, this means that the woman is healthy and has never had this disease in the past. However, this result also indicates a lack of immunity against such infections. In this case, the expectant mother needs to protect herself from possible infection and regularly take a blood test for TORCH infections.
If the patient has IgM antibodies, but no IgG immunoglobulins, this means that the woman has had this disease in the past and has developed immunity. In this case, there is no danger to the child.
If the transcript of the analysis for TORCH infection indicates that class G and M antibodies are present in the blood, this means an exacerbation of a chronic disease. There is a danger of intrauterine infection of the embryo. In this case, an additional test for immunoglobulin avidity is performed.
If a patient has class M antibodies, but no class G antibodies, this indicates that she was recently infected and is acutely ill. In such cases, the risk of infection of the fetus is very high. It is necessary to do an ultrasound of the embryo. If this examination shows the presence of pathology in the embryo, then an analysis of the amniotic fluid (amniocentesis or cordocentesis) is prescribed.
What infectious agents are dangerous during pregnancy and most often lead to IUI?
To be honest, any pathogens (viral, bacterial, parasitic) can be dangerous for a woman and an unborn child under certain circumstances at any stage of pregnancy. That is why, even at the planning stage, and, of course, in the first trimester of pregnancy, a woman is offered a blood test to determine HIV, hepatitis B, syphilis, gonorrhea, chlamydia, ureaplasma, mycoplasma, etc. But don’t get too carried away with diagnostics and forget that determining the state of a woman’s immune system requires a wise approach, taking into account the life history and medical history of the woman, the endemic zone in which she lives. And our reality shows that the most common cause of intrauterine infections in the fetus is TORCH infections, which is why research on TORCH infections has become so relevant recently. The sad thing is that doctors often refer patients for studies, but do not know how to correctly interpret (interpret) the results of these studies, as a result - unjustified terminations of pregnancy and “successful” prescription of drugs, the use of which is not only unnecessary, but in general, occur all the time. they have nothing to do with the treatment of these infections. It becomes even sadder when her husband is sent along with a woman to the TORCH test and senseless and unnecessary treatment is prescribed to a married couple, turning preparation for pregnancy into a pointless visit to doctors with endless waste of money. So let's figure out what is hidden behind this abbreviation TORCH? This abbreviation is made up of the initial letters of the Latin names of four infections with similar manifestations, including rash and ocular symptoms: TO - toxoplasmosis, R - rubella, C - cytomegaly, H - herpes. Recently, a slight change has been made in the interpretation of this abbreviation; O – “otros” (others) has been added separately. In addition, the word “torch” itself is translated from English as “torch,” emphasizing the danger and serious consequences of these diseases. Let's look at a brief description of the main representatives of TORCH infections.
The causative agent of toxoplasmosis
is a parasite that multiplies in the cells of various animals, birds and people during the acute period of infection.
Toxoplasmosis is often called the disease of “dirty hands”, since infection with toxoplasma often occurs through contact with the feces of infected with parasites
or with soil.
Infection is also possible through consumption of insufficiently heat-treated meat and other products of animal origin, unwashed vegetables and fruits; cases of infection through blood transfusions have been described. From person to person, toxoplasmosis is transmitted only (!)
transplacentally, that is, from a sick mother to the fetus. Toxoplasma is considered not dangerous for the unborn child if the infection occurred more than 6 months before conception; the likelihood of transmitting it to the fetus increases as the moment of conception approaches. About one third of women infected with Toxoplasma during pregnancy transmit the parasite through the placenta to the fetus, the remaining two thirds give birth to healthy, uninfected children. Since this parasitic disease can be identified and treated, it is advisable for a woman planning a pregnancy to be tested for toxoplasmosis, or rather to check whether there is immunity to toxoplasma (immunity to toxoplasma is persistent and lifelong). Since the development of IUI in a fetus with toxoplasmosis is possible only with primary infection of the mother during pregnancy, it is necessary to determine in advance whether the expectant mother is at risk for toxoplasmosis. It is very important to teach a woman who does not have specific immunity to Toxoplasma a lesson on preventing Toxoplasma infection. If a woman does not have immunity, then in the first trimester of pregnancy she must be tested for toxoplasmosis again. Even if a primary infection occurs during pregnancy, there is no need to be sad, since there is a specific treatment that can reduce the risk of infection of the baby to 1%. The safest in this case are drugs based on spiramycin, an antibiotic from the macrolide group (for example, rovamycin).
In most countries of the world, an analysis to determine immunity to rubella is desirable during preparation for pregnancy. Since fetal infection occurs only when a woman is initially infected with rubella during pregnancy, and there is no effective treatment for this viral infection, 100% screening of all women planning pregnancy is desirable. At the same time, all women at risk who are negative for IgG before pregnancy, and therefore do not have immunity to the rubella virus, need vaccination. You can become pregnant after vaccination after three months, since by this time post-vaccination immunity will have already been formed. At the same time, a vaccination accidentally given during the conception cycle is not an indication for induced abortion, since the risk of infection of the fetus after vaccination is only theoretical. If the test result for rubella is positive, during the period of preparation for pregnancy, it is important to take into account that this may be a good immune defense of the body as a result of a disease suffered in childhood (more than 90% of children suffer from rubella asymptomatically) or a vaccination given in childhood. Such a woman does not need treatment in any way.
Cytomegalovirus is very common among the adult population; according to some estimates, from 90 to 100% of this population are infected with the virus and are its carriers. Reactivation of CMV infection occurs infrequently and is usually asymptomatic. If a woman is diagnosed as carrying the cytomegalovirus virus, then there should be no panic, much less hasty treatment. Since antiviral drugs used to treat active cytomegalovirus infection are contraindicated in pregnant women, it is necessary to simply monitor the condition and development of the fetus, without raising unnecessary anxiety and without being needlessly frightened by thoughts of the birth of an unhealthy child. In case of chronic viral carriage of cytomegalovirus, the chance of the fetus being affected by an infection and developing abnormalities is several times less than the chance of spontaneous development of defects, for example, as a result of chromosomal or genetic abnormalities. The risk of intrauterine infection and the nature of damage to the fetus depend on the presence of antibodies in the mother and the period of infection of the fetus. With primary maternal infection, the probability of infection of the fetus is 30%. Therefore, women who are at risk due to the lack of antibodies to CMV need special educational work during pregnancy; monthly monitoring of antibodies to CMV and indicators of infection activity is also desirable, especially if pregnancy falls in the autumn-winter period.
Herpes simplex virus is no less common than CMV, and most of the world's adult population carries this virus. The first type of herpes occurs in almost 100% of the adult population, and most often (in 95% of cases) it causes colds. The second type of this type of virus causes genital herpes, but in most cases a genital rash never appears, and the person does not even realize that he is a carrier of the genital herpes virus.
Naturally, such a person does not need treatment. It must also be remembered that activation of herpes infection with clinical manifestations occurs only in 25% of infected people; in the remaining 75%, the activity of the virus can only be determined by laboratory tests. Therefore, diagnostic tactics in preparation for pregnancy and during pregnancy do not differ from those for CMV. Women who have had elements of a herpetic rash on the skin of the perineum and in the vagina, or whose body is completely unfamiliar with the virus, are usually at risk even before pregnancy, and they are allowed to become pregnant. These women are observed no more often than other pregnant women, especially if there are no signs of reactivation of the infectious process, laboratory tests are carried out to determine the herpes condition at least 2-3 times during pregnancy. Such women give birth naturally, i.e. through the vagina, but only if there are no signs of active infection on the skin of the perineum and in the vagina. If a woman has a herpetic rash on the external genitalia often, before pregnancy it is necessary to undergo a tablet course of antiviral treatment, which will not get rid of the virus, but will suppress the activity of the infection.
Treatment
Treatment of TORCH infections depends on the woman’s condition. It is important to clarify whether the patient is currently pregnant or is just planning to conceive a child. If the examination reveals a disease at the stage of pregnancy planning, then a full course of antibacterial or antiviral therapy is carried out.
The situation becomes much more complicated if the analysis shows infection during gestation. If the disease is detected in the first trimester and poses a serious danger to the development of the child, then doctors most often recommend terminating the pregnancy.
If the infection occurred in the second or third trimester, then consultation with an experienced infectious disease specialist is necessary. The doctor will help you choose the most gentle antibacterial and antiviral drugs that have a minimum of side effects. It is very important to treat the child after birth. It includes the prescription of antimicrobial agents, as well as the correction of developmental abnormalities and dysfunctions of internal organs.
This is the main thing.
But today there is not a single TORCH infection due to which an infected woman could not give birth to a healthy child. Today, say, with hepatitis C, the risks of giving birth to an infected child are 1-2%, no more, and 98% of women infected with the hepatitis C virus give birth to healthy children. However, if the level of virus activity is high, it is better to deliver by caesarean section. The same applies to toxoplasmosis, hepatitis B virus, and herpes virus. With the right approach to controlling TORCH infections, any woman can give birth to a healthy child.
What is the danger
The fact is that if the mother’s body has not previously been infected with a torch infection, which is the danger, then it has not developed immunity. And during primary infection, many microbes begin to circulate in the blood and can penetrate the child’s body, disrupting its development.
The important thing is that the symptoms of the disease may not be expressed or may be insignificant. Thus, even without suspecting an infection, a woman will not be able to recover in time. And the infection at this time will negatively affect the pregnancy and the condition of the fetus.
An encounter with any of these infections can have a detrimental effect on the fetus. The virus is capable of infecting all systems of a small organism, and especially its central nervous system. Therefore, the detection of Torch infections is very often an indication for artificial termination of pregnancy. Otherwise, there is a risk of giving birth to a defective or dead child, and the child may also have developmental defects and even disabilities.
In this situation, it is the primary infection with the virus that is very dangerous, since the woman’s body does not have immunity to it and will not be able to cope with the disease. A secondary encounter with the virus is not so dangerous, for the reason that the body has already produced antibodies to it before and has a developed immunity.