An ovarian cyst of the paraovarian type is a single-chamber capsule that is filled with fluid. It appears between the ovary and the fallopian tube. The amount of fluid in the cyst gradually increases, causing it to begin to grow. This pathology is usually diagnosed in women whose bodies are ready to conceive and bear a child. This problem can also affect teenage girls.
Description
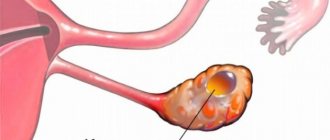
Paraovarian cyst.
A tumor-like cavity formation that forms from the epididymis. A paraovarian cyst may be asymptomatic or cause periodic pain in the abdomen and lower back; Sometimes the cyst is accompanied by menstrual irregularities and infertility. Complications may include suppuration of the parovarian cyst, torsion of the pedicle, or rupture of the capsule. A paraovarian cyst is diagnosed using a vaginal examination and ultrasound. Treatment consists of enucleating the cyst while preserving the ovary and fallopian tube.
How does a paraovarian cyst occur?
Both men and women have organs that are formed during embryonic development, but do not fully develop. They are vestigial, or have lost their meaning. In women, near each ovary, both on the right and on the left, in the broad ligament of the uterus there is a formation related to rudimentary organs - this is the periovarian appendage, or paraophoron. It is represented by a network of thin, disconnected tubules that end blindly. It is from the paraophoron tubules that paraovarian cysts arise when embryonic development processes are disrupted.
Formation mechanism
The growth of true cystic tumors occurs due to the division of epithelial cells lining the inner surface of their capsule. These cells are capable of pathological degeneration. A paraophoron cyst is not a true cyst, since it is formed in a completely different way: the tubules produce fluid that has nowhere to go, it accumulates, forming a cavity. The increase in volume occurs due to the stretching of the walls by the liquid contents. Due to this mechanism of occurrence, the formation does not become malignant.
Reasons for development
The basis for the appearance of cystic formation of the paraophoron is a violation of tissue differentiation at the stage of embryonic development. Contribute to its occurrence:
- menstrual irregularities;
- premature puberty;
- endocrinological diseases (hyperfunction, hypofunction of the thyroid gland, etc.);
- chronic inflammatory processes of the female genital area;
- uncontrolled use of hormonal contraception;
- spontaneous miscarriages;
- artificial termination of pregnancy;
- prolonged sunbathing, passion for artificial tanning;
- excessive thermal procedures (hot baths, warming applications);
- sudden weight loss;
- obesity.
A balanced diet, adequate sleep, and an active lifestyle weaken the effect of provoking factors. Excessive emotional and physical stress and bad habits lead to the opposite effect.
Additional facts
The paraovarian cyst is located intraligamentally, in the space limited by the leaves of the broad uterine ligament, between the ovary and the fallopian tube.
This is a single-chamber cavity formation that occurs when embryogenesis is disrupted from the tubules of a rudimentary formation - the periovarian appendage (paraovary). A paraovarian cyst is usually detected during puberty, between the ages of 20 and 40, and less often during puberty. In gynecology, paraovarian cysts occur in 8-16% of all detected additional ovarian formations.
Paraovarian cyst
During pregnancy
Pregnancy causes natural hormonal changes in the body. This can provoke a sharp growth of the cyst. At the same time, the growing uterus will put pressure on it, which threatens to rupture the formation.
A woman should undergo all examinations during pregnancy planning, trying to exclude such a problem in the future.
Characteristic
A paraovarian cyst is a smooth-walled formation of oval or round shape, tight-elastic consistency, located on the side or above the uterus. The walls of the paraovarian cyst are thin (1-2 mm) and transparent, inside they are lined with single-row squamous, cubic and columnar epithelium. A parovarian cyst contains a homogeneous, transparent, watery fluid with a large amount of protein and a low content of mucin. An enlarged fallopian tube runs along the upper pole of the paraovarian cyst; The ovary is located at the posterior-inferior surface. The blood supply to the cavity formation is carried out by the vessels of the mesentery, fallopian tube and the own vessels of the cyst wall. The pedicle of a paraovarian cyst is formed by a leaf of the broad ligament, sometimes by the ovarian ligament and the fallopian tube. The paraovarian cyst is inactive, grows slowly and can remain small for a long time. The enlargement of the cyst occurs due to the accumulation of contents and stretching of its walls. The average size of symptomatic paraovarian cysts is 8-10. In rare cases, the size of the cyst can reach the head of the newborn. Paraovarian cysts never become malignant. The enlargement and growth of paraovarian cysts can be facilitated by inflammation of the ovary and uterine appendage (oophoritis, adnexitis), endocrine diseases (including hypothyroidism), early puberty, repeated surgical termination of pregnancy, STIs, uncontrolled hormonal contraception, insolation (tanning in a solarium or under sun), local hyperthermia (hot general baths, warming up). A tendency towards an increase in paraovarian cysts is observed during pregnancy.
Methods of classical medicine
If a paraovarian ovarian cyst has already been found, treatment without surgery is impossible. Pills that normalize the endocrine system do not work, since the cyst does not depend on its functioning in any way. This also applies to the treatment of ovarian cysts with contraceptives when the paraovarian ovarian cyst grows. Reviews about drug treatment are mostly negative. No one has yet been able to completely cure a cyst with pills. Without surgery, therapy boils down to monitoring the cyst and controlling its growth.
Usually small capsules are not operated on if they are growing slowly. A large paraovarian ovarian cyst is removed. Treatment is carried out using laparoscopy. This is the main method for removing benign tumors in modern practice. You need to carefully prepare for it, as this is a full-fledged operation. Failure to take the procedure seriously can cause a whole bunch of problems.
When a paraovarian ovarian cyst is removed, laparoscopy may be delayed for several months. The main obstacle to recovery is often excess weight. Obesity not only hinders access to pathology, but also “pulls” a whole bunch of diseases. Such as problems with blood pressure, shortness of breath, improper functioning of the pancreas and thyroid glands. All this increases the risks of surgery, so you must first carry out a set of procedures that will remove concomitant diseases.
Contraindications include:
- bronchial asthma and other respiratory system problems;
- too high or low pressure;
- hernias in the abdominal area;
- malignant tumors;
- adhesions in the area of the cyst.
When the patient is ready for surgery, the procedure itself does not take much time. During the recovery period, the patient is monitored and her condition is assessed. If necessary, support the body with medications. If the operation went well, the patient quickly returns to normal. The cyst does not recur, so the patient can be considered completely healthy.
Diagnostics
Detection of a paraovarian cyst often occurs during a routine ultrasound or consultation with a gynecologist, sometimes during diagnostic laparoscopy for infertility. During a bimanual gynecological examination, a unilateral painless tumor-like formation is palpated on the side or above the uterus, having smooth contours, elastic consistency, and limited mobility. During transvaginal ultrasound, a round or ovoid thin-walled formation with homogeneous anechoic content, less often with a fine suspension inside, is determined. An echoscopic criterion for a paraovarian cyst is the visualization of an intact ovary. A paraovarian cyst is differentiated from an ectopic pregnancy, an ovarian cyst, and true ovarian tumors.
Symptoms
Cavity formation can be completely asymptomatic and detected by a gynecologist during routine preventive examinations or an ultrasound examination of the pelvic organs for another reason. Clinical manifestations are usually due to the large size of the formation and complications such as:
- leg torsion;
- capsule rupture;
- suppuration.
In this case, complaints signaling a catastrophe in the abdominal cavity come to the fore. These include:
- cramping abdominal pain;
- weakness;
- nausea and vomiting;
- dizziness;
- feeling of fear;
- chills;
- drop in blood pressure;
- decreased intestinal motility;
- hyperthermia.
When the formation of the periovarian appendage reaches a significant size, and in some cases its diameter can reach 20 centimeters, symptoms of compression of neighboring organs come to the fore.
Organ that has been compressed
Bladder, ureter
Frequent urination, often accompanied by pain of varying intensity, false urges, and a feeling of incomplete emptying of the bladder.
Intestinal bloating, discomfort, pain during bowel movements, tendency to constipation or increased bowel movements.
Pain in the right or left iliac region, depending on the location of the formation, often aggravated by sexual intercourse or physical activity; disturbance of the rhythm of the menstrual cycle.
Cavity formation of the periovarian appendage does not respond to fluctuations in the level of sex hormones; its characteristic feature is the absence of dependence of the intensity of pain on the phase of the menstrual cycle.
Treatment
Unlike functional retention formations of the ovary (corpus luteum cyst, follicular cyst), paraovarian cysts do not disappear on their own. An asymptomatic small paraovarian cyst can be kept under dynamic observation. However, due to the fact that paraovarian cysts are diagnosed in patients of reproductive age, are often complicated and are not always correctly differentiated, the preferred surgical tactic for them is enucleation of the cyst. Also, planned removal of a paraovarian cyst is required before planning pregnancy or IVF. Removal of a paraovarian cyst is usually performed during surgical laparoscopy, or less commonly, laparotomy. In case of an uncomplicated course of the paraovarian cyst, during the operation the anterior layer of the broad uterine ligament is dissected, and the cyst is removed from the intraligamentary space. The ovary and fallopian tube are preserved during enucleation of a paraovarian cyst. After removal of the paraovarian cyst, due to its retraction properties, the deformed fallopian tube contracts and takes on its previous shape. In exceptional cases, it is possible to perform a targeted puncture of a paraovarian cyst with aspiration of the serous contents and the simultaneous injection of alcohol into it, which promotes obliteration of the cavity.
Symptoms
Small cysts can be in the body from birth. Until the capsule grows, it does not interfere and does not give obvious manifestations. A paraovarian ovarian cyst on the right, for example, often becomes an incidental finding when a woman undergoes an ultrasound with complaints of appendicitis.
Paraovarian cyst of the left ovary does not cause any hormonal disorders, such as acne, weight changes and other manifestations of malfunction of the endocrine system. It is easy to notice that the ovary is a paired organ. Both of them work in the same way and consist of the same tissue, therefore diseases on each of them develop in the same way. A paraovarian ovarian cyst on the right will appear similarly.
Symptoms directly depend on size. If the cyst grows more than 4-5 centimeters, then women complain of the following symptoms:
- pain that appears and goes away without a system and does not depend on the cycle;
- intestinal disorders;
- frequent trips to the toilet;
- sex causes pain and discomfort;
- aching in the stomach during exercise and active movement.
A paraovarian ovarian cyst on the left or right grows slowly, but once growth begins, the disease does not go away on its own. Doctors cannot predict to what size the tumor will grow - this is the main danger of this pathology. The cysts grow really big. But, unlike a tumor, the increase in size does not occur due to cell proliferation. The walls of the cyst stretch due to the accumulation of fluid. Accordingly, the larger the cyst, the thinner the walls and the higher the likelihood of their rupture.
Possible complications
With intense physical activity, sudden changes in body position, excessive insolation or local hyperthermic effects, a paraovarian cyst can be complicated by torsion of the pedicle, suppuration of the contents, or rupture of the capsule. When the pedicle of the cyst is torsed, the uterine ligament, nerve and vascular trunks, and often the fallopian tube are compressed. In this case, necrosis of the paraovarian cyst develops, which is accompanied by a sharp deterioration in health: cramping pain throughout the abdomen that is not relieved by taking analgesics; tension in the anterior abdominal wall, gas retention, tachycardia, drop in blood pressure, pale skin, sticky cold sweat. Suppuration of a paraovarian cyst is caused by lymphogenous or hematogenous introduction of pathogenic microflora. This complication is manifested by fever with a temperature of up to 38-39 ºС, intoxication, sharp diffuse pain in the abdomen, and vomiting. When a paraovarian cyst ruptures, general symptoms of shock, sharp pain, and signs of internal bleeding are observed. All complications of a paraovarian cyst require emergency surgical intervention in the amount dictated by the clinical situation (for example, oophorectomy, adnexectomy).
Methods of therapy: are medications and folk remedies effective?
Treatment tactics depend on many factors:
- size of education;
- presence of symptoms;
- condition of a woman.
If a small cyst is found that does not cause negative feelings in the woman, the doctor will recommend monitoring the pathology. The patient needs to come for a preventive examination every 5-6 months.
If the tumor is large in size or tends to enlarge, it is recommended to resort to surgical intervention.
Since the paraovarian cyst is not able to resolve, treatment with medications or folk remedies will not bring the desired result. This tactic will delay the operation and can provoke a number of serious complications.
Lifestyle
Those with small lesions who are not offered surgical intervention need to reconsider their lifestyle.
Physical activity for paraovarian cysts is not contraindicated, but the types of exercises should be discussed with your doctor
Doctors advise adhering to the following rules:
- Adequate physical activity. Intensive exercise is not advisable at all. It is recommended to exclude exercises associated with sudden changes in the body or straining (somersaults, rotational movements, falls, jumps). Sports activities must be coordinated with your doctor.
- Exclusion of thermal measures. A woman is advised not to take hot baths (water should not exceed 38 C). You should not visit baths and saunas.
- Limit exposure to ultraviolet radiation. It is not advisable for a patient who has a paraovarian cyst to sunbathe excessively in the sun. Visiting a solarium will not be beneficial either.
- During sex, it is necessary to choose comfortable positions that do not cause pain in the woman.
A paraovarian cyst is not a contraindication to the installation of an intrauterine device.
Surgical intervention
Surgery is the only method that can rid a woman of a paraovarian cyst.
Indications for surgery
The main indications for surgical removal of a paraovarian cyst are the following conditions:
Recent Entries
Is it possible to give a mirror: how to protect yourself from bad omens It became known about the influence of cell phone towers on human health Is it possible to eat bananas bought in Russia?
- The woman experiences pain and discomfort caused by the large size of the formation.
- Rapid increase in cyst size.
- The occurrence of complications (torsion of the legs, suppuration, rupture of the capsule).
The only way to treat a paraovarian cyst is surgical removal of the formation.
- The inability of a woman to become pregnant naturally. Sometimes a paraovarian cyst can cause infertility in a patient.
- Planning pregnancy (naturally or using IVF). Doctors recommend removing the cyst so that during pregnancy there is no need for emergency surgery due to possible complications.
Types of surgical interventions
The operation is performed (depending on the presence of complications and the size of the formation) in two ways:
- Laparoscopy. This operation is possible for small cysts. In this case, an instrument and a special telescopic tube are inserted into the peritoneum through small punctures. Carefully monitoring all manipulations using a camera, the surgeon excises the cyst. The ovary is not affected during the operation. This is a low-impact intervention. The woman recovers quickly after it (within 3–5 days).
For small cysts, laparoscopic surgery is used
- Median laparotomy. If the cyst has reached a large size, then laparoscopy cannot provide normal access to the formation. In this case, an incision is made along the midline. This intervention is more traumatic. In some cases, it is possible to save the ovary, but sometimes this organ is removed along with the cyst. Rehabilitation of a woman after laparotomy can take 10 days.
Reviews from women about cyst removal
In the spring I had an ultrasound and didn’t notice anything, but in the fall pain appeared and I went for an ultrasound again; they diagnosed a 7 cm cyst. They prescribed hormonal pills - it didn’t help.
sent to the lapara. I was very freaked out at first and in the end there were three small scars (where the ovaries are, and next to the navel), similar to cat scratches and almost invisible)). Only after the operation it turned out that I have a paraovarian cyst, which can only be removed surgically, and when removing it the ovary is not affected! the doctor even said that I was lucky that it was this type of cyst))) Guest
https://www.woman.ru/health/woman-health/thread/3995956/
I was also diagnosed with a paraovarian cyst measuring 29 by 18, my gynecologist first prescribed me hormonal pills, nothing helped ((now the question is about removal, but for now I will be under observation and there is no talk about urgent surgery. This type of cyst does not resolve. My friend I walked with this cyst for 3 years, had a laparoscopy and have been walking happy for 2 years now. This operation is considered gentle, and you can get pregnant later.
Olga
https://www.woman.ru/health/woman-health/thread/3995956
I had a laparoscopic procedure to remove a steam cyst on 02/03/2012….
It didn’t bother me at all and it was discovered in me back in 2006. But since I am planning a pregnancy, they suggested that I have it removed, because it is unknown how it will behave during pregnancy (it may twist and burst)... Almost 3 months have passed, but after the operation I am bothered by pain in the ovarian area. On May 5, I will go to the gynecologist, who sent me for laparoscopic surgery, and I will consult about these pains ((((...And so I decided to have the operation only because I want a healthy child and a pregnancy without problems...... Victoria
https://www.woman. ru/health/woman-health/thread/3995956/
I had a paraovarian cyst several years ago... they did a laparoscopy. I went to the hospital for 3 days: 1st day - they prepare me, 2nd - surgery (3 punctures in the stomach), 3rd day - examination and send home. not scary! Only the cyst was removed, everything else (in the feminine sense) is in place...
after some time she gave birth to 2 children.
Alanta
https://eka-mama.ru/forum/part16/topic208372/message4690807/?PAGEN_1=2
At 6 weeks of pregnancy, I was discovered with this 5 cm cyst, the doctor said it was nothing to worry about. It doesn’t affect the pregnancy in any way, aside from that, it can form due to the accumulation of fluid in the places of adhesions. During the CS, the cyst was cut out and they showed me. looks like some kind of fatty deposits. But it’s not liquid, but like a sponge..
5 years later, during the second ultrasound, they found the same one, only on the other side. I don’t plan to specifically cut it out, it doesn’t bother me at all yet
Nataletta
https://www.babyplan.ru/blog/17238/entry-66452-paraovarialnaya-kista-vo- vremya-beremennosti/#ixzz4PsbQaKXB
Forecast
Conception against the background of a paraovarian cyst is quite likely, however, with the enlargement of the uterus and its extension beyond the pelvis, the risks of torsion of the cyst pedicle increase. Management of pregnancy in patients with a paraovarian cyst requires constant dynamic monitoring of the condition of the formation. After surgical treatment of a paraovarian cyst, no relapses are observed, since the rudimentary tissues from which the formation is formed are completely removed. Modern gynecology recommends planning a pregnancy no earlier than 3-4 menstrual cycles after the operation.
Preventive actions
Prevention is based on simple and accessible recommendations:
- Timely diagnose and treat any inflammatory or infectious pathologies of the pelvic organs.
- Strictly observe hygiene rules.
- Avoid frequent visits to the solarium. Prolonged exposure to the sun is not recommended.
- Avoid casual sex or use a condom.
- Visit your gynecologist regularly (2 times a year).
A paraovarian cyst does not pose a threat to a woman in terms of cancer. However, it can become a source of serious consequences. That is why it is necessary to constantly be observed by a gynecologist and strictly follow all his recommendations. This will allow for a timely operation in which the ovary will be preserved. And conditions that threaten the health and life of the patient simply will not arise.
Reasons for the development of pathology
Cysts from the tissues of the ovarian appendages are formed for various reasons. Sometimes the basis may be the negative influence of drugs, tobacco, experienced in the prenatal period. There are also provoking factors:
- inflammatory diseases of the reproductive organs (adnexitis, salpignoophoritis);
- pathologies of the thyroid gland, other endocrine problems;
- abortions;
- chronic stress;
- frequent infections, affecting not only the reproductive organs.
From the entire list of probable causes, it is clear that the formation of the capsule occurs against the background of hormonal imbalance. Therefore, they may occur during adolescence, pregnancy and menopause, when the concentration of substances changes naturally. So these conditions can also become precipitating factors in some way.
A paraovarian ovarian cyst during pregnancy does not affect the development of the fetus. But if it is large, there is a risk of rupture or torsion. A woman feels worse because she is forced to carry double weight; she may have problems with urination and constipation. Childbirth will also require more careful management, since careless movement does not exclude rupture of the capsule. The tumor can be treated only after them, unless there is a need for emergency help.
Paraovarian ovarian cysts in menopause are less common, but require special vigilance. There is no talk of its degeneration into cancer, but this capsule may not be the only gynecological problem. The possibilities of its growth are limited by a reduced level of sex hormones. But there may be jumps in it that will push the development of the cyst.
Presence of paraovarian formation and pregnancy
If there is a cystic formation of the paraophoron, it is necessary to decide what to do with it, and only then plan a pregnancy. If the cyst is 1-2 cm in size, surgery may not be performed; if larger, laparotomy is indicated. It is better to plan conception no earlier than 3 months after surgery.
The discovery of a paraophoron cyst in a pregnant woman is not a contraindication to pregnancy. It is necessary to regularly visit an antenatal clinic and follow the recommendations of an obstetrician-gynecologist.
The small diameter and lack of growth of the cavity formation allow us to limit ourselves to ultrasound monitoring during pregnancy and with the exception of:
- excessive physical activity;
- sexual intercourse in the presence of discomfort, pain during or after intimacy;
- thermal procedures (sauna, hot bath, etc.).
It is necessary to observe a work-rest schedule and wear a bandage in late stages of gestation.
The rapid growth of the cyst and the development of complications are not compatible with conservative tactics. Modern technologies make it possible to perform operations without disrupting the course of pregnancy.