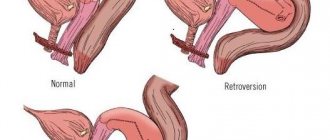
Anatomical features of the organ
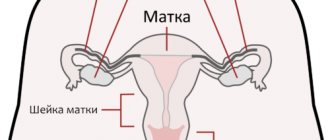
The uterus is an unpaired hollow muscular organ that is located near the bladder and rectum. The fallopian tubes are hollow, paired organs that are an important part of the female reproductive system. They are located in a horizontal plane and originate from the lateral surfaces of the uterine fundus. Their length is up to 11-13 cm. The tubes are located in the folds of the peritoneum and are narrow cylindrical channels, which are covered from the inside by ciliated epithelium, and from the outside by a connective tissue membrane.
According to static data, the length of the left pipe is slightly less than the right one. The fallopian tubes are such tiny structural elements of a woman's reproductive system that most modern ultrasound machines simply cannot visualize them. These organs are in a constant “floating” state, which also makes it difficult to examine them in detail using ultrasound. In most cases, if the pipes are not visible, this indicates the absence of pathological changes.
Physiological features
The main functions of the fallopian tubes are the movement of eggs and sperm; these organs create the most favorable conditions for successful fertilization, the development of zygotes and their further transportation to the uterus. Each tube begins in the uterine region, enclosed in the myometrium and reaching a length of up to 25 mm. From the uterus, the tubes pass into isthmuses - thin horizontal canals up to 35 mm long. The isthmus passes into the ampullary section - the longest section of the tubes. At the end of the pipes there are peculiar funnels covered with narrow, long fibers - fimbriae. They are the ones who capture the eggs and transfer them to the tube area.
Brief anatomy and mechanism of fertilization
The fallopian tubes are paired tubular formations. The average length of each of them at reproductive age is from 10 to 12 cm, and the diameter of the lumen in the initial section does not exceed 0.1 cm. There is liquid in the lumen of the tubes. Anatomically, they are divided into three sections:
- Interstitial, located in the thickness of the muscular wall of the uterus (1-3 cm) and communicating through its lumen with its cavity.
- Isthmus (3-4 cm), which passes between the two layers of the broad uterine ligament.
- Ampullary, ending in a funnel, the lumen of which (orifice) communicates with the abdominal cavity. The mouth of the funnel is covered with fimbriae (villi, thin threads), the longest of which is fixed to the ovary located under the ampulla. The remaining fimbriae, with their vibrations, capture the matured egg released from the ovary and direct it into the lumen of the tube.
Structure of the fallopian tube
The walls of the fallopian tube consist of three membranes:
- External, or serous.
- Internal, or mucous membrane, in the form of branched folds. The inner layer of the mucous membrane itself is ciliated epithelium with villi (outgrowths). The thickness of the shell is uneven, and the number of folds is unevenly located. The villi undergo fluctuations, the speed of which is maximum during the period of ovulation and some time after it, which depends on the hormonal level.
- Muscular, which in turn consists of three layers - two longitudinal and one transverse, which ensures peristalsis (wave-like movement) of the pipe walls. This resembles peristaltic contractions of the intestine, promoting the movement of food masses through its lumen.
In addition to the broad ligament, the cardinal and round ligaments are attached to the uterus. All of them provide fixation and a certain position of the uterus with appendages in the pelvis.
A general understanding of the structure of the organ allows us to better understand the causal mechanisms and how to treat obstruction of the fallopian tubes, as well as the importance of preventing inflammatory diseases of the uterus and its appendages for the implementation of the mechanism of fertilization.
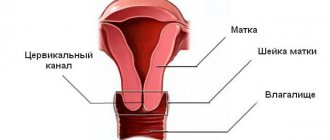
The sperm penetrates through the cervical canal and the uterine cavity into the fallopian tube, where it connects with the egg.
Vibrations of the villi, tubal peristalsis, relaxation of the uterine muscle in the area of its connection with the tube, as well as the directed flow of fluid in the tube ensure the movement of the egg, and after its fertilization, the fertilized egg, through the tube into the uterine cavity.
Here it attaches (implants) to the endometrium (the lining of the uterus). The mechanism of the transport function is realized under the influence of hormones, mainly progesterone and estrogens, secreted by the corpus luteum of the ovary.
Why do ultrasounds be done?
Ultrasound is a simple, painless technique that is performed according to indications: for complaints of pain in the lower abdomen, menstrual irregularities, heavy periods, intermenstrual bleeding, to control ovulation, as well as timely detection of tumors. The procedure is also prescribed to patients with a history of sexually transmitted diseases in preparation for in vitro fertilization. During pregnancy, the procedure is performed every trimester to monitor the growth and development of the fetus. Conventional ultrasound does not visualize the fallopian tubes and other diagnostic techniques are used to determine the patency of organs.
How is it carried out?
When planning a transabdominal ultrasound, it is recommended to avoid eating foods that cause increased gas formation 24-48 hours in advance. On the day of the procedure, you must drink at least 1 liter of fluid to fill your bladder. In order to conduct an ultrasound examination of the uterine appendages, hydrosonography is recommended. Progress of the procedure:
- a woman is asked to take a comfortable position on a gynecological chair
- a thin catheter will be inserted through the cervix, which will deliver a portion of saline solution
- The procedure is monitored by a diagnostician, while the saline solution gradually fills the uterus and fallopian tubes
- After the procedure is completed, the sensor will be removed from the vagina, and the catheter will be removed from the uterus
About 70% of women with infertility suffer from complete or partial obstruction of the fallopian tubes.
How to do the procedure
During ultrasound diagnostics of the pelvic organs, diagnosing the patency of the tubes is impossible: their lumen is not visible on the screen of the ultrasound machine. Therefore, echoGSS or USGSS is used - a procedure in which a special pigment is used to illuminate areas where ultrasonic waves only partially penetrate.
In ultrasonography, a sonologist uses a catheter in an outpatient setting. The doctor evaluates how a special pigmented solution flows through the fallopian tubes using an ultrasound sensor. HSG ultrasound is performed through the abdominal cavity or transvaginally.
Echosalpingography is a test that is prescribed for women with suspected infertility. In this case, the pathology affects not only the fallopian tubes, but also other adjacent organs.
Young girls who are unable to get pregnant are prescribed echohydrotubation. The procedure is completely safe, as only ultrasound waves are used without x-rays.
Hysterosonography is performed as follows:
- The doctor places the woman on the gynecological chair. The back of the chair lowers.
- A special speculum is inserted into the vagina. Then the cervix and vaginal cavity are processed.
- A disposable thin catheter with a contrast agent is inserted through the cervical canal. An inflating balloon is provided at the tip of the catheter to fix the position.
- Using an ultrasonic vaginal sensor, the correct positioning of the catheter during the study is assessed.
- A sterile saline solution is passed through the catheter. It moves along the fallopian tubes.
- The area where the saline solution is flowing is highlighted on the ultrasound machine screen. Where the solution stops, the adhesive process is recorded.
To get the most reliable clinical picture, you need to choose the right days. This is very important when an ultrasound is performed. Gynecology (which days are considered the most suitable, we will discuss below) is a special branch of medicine that requires responsibility on the part of the doctor, because the health of not only the woman, but also her future offspring depends on his actions.
Doctors recommend conducting the study taking into account the following timing:
- The period from the 6th day of the cycle to the 21st.
- Some gynecologists advise performing an ultrasound before ovulation, from the 7th to the 12th day of the cycle.
Why are these particular dates considered the most optimal? Doctors say that during these periods the cervix is maximally dilated. The endometrium after menstruation is minimally thick. These features allow the study to be carried out as accurately as possible.
When there is cause for concern
Due to the progression of the inflammatory process, activation of adhesive processes in the area of the fallopian tubes may be observed. This is accompanied by nagging pain, menstrual irregularities, and difficulties in conceiving a child. For any of the described or any other symptoms, it is recommended to refrain from self-medication and seek advice from an experienced gynecologist. The sooner specialists identify the cause of the disorder and direct efforts to eliminate it, the more favorable the prognosis for the woman.
Causes of disorders in the reproductive system
The main reasons that can provoke genital dysfunction include:
- termination of ectopic pregnancy
- development of inflammatory processes in the appendages: salpingoophoritis, adnexitis, oophoritis
- progression of endometritis - an inflammatory process that affects the inner lining of the uterus and occurs as a complication of abortion, curettage
- formation of adhesions caused by surgical interventions, peritonitis
- abnormal development of internal genital organs (bicornuate uterus)
To confirm the diagnosis, a comprehensive examination by a gynecologist and a number of diagnostic procedures are required: both instrumental (ultrasound) and laboratory. In order to fully examine the uterus and its appendages, the administration of contract drugs is required. The procedure is carried out only in case of objective indications; this is not a routine study recommended for all categories of women.
Bicornuate, vestigial uterus
A bicornuate uterus is a pathology of organ development, which is accompanied by the formation of two separate parts with cavities. In the lower part of the uterus, such “horns” unite, and a common canal opens into the vaginal area. Such a disorder occurs as a result of hereditary predisposition and exposure to external provoking factors. These can be toxic substances, viral infections, heavy metals, pathogenic microorganisms of bacterial origin.
There are no specific symptoms for this disorder. In some cases, menstrual irregularities, uterine bleeding, miscarriage, and difficulty conceiving may occur. In most cases, a bicornuate uterus is discovered by chance, during a routine examination by a gynecologist. In most cases, specific therapy is not required. Surgical correction is performed only if there are difficulties with conception.
Oophoritis
Oophoritis is an inflammatory process that affects the ovaries. Develops under the influence of infectious and inflammatory processes: endometritis, vulvovaginitis, adnexitis, sexually transmitted infections. Among the predisposing factors that can provoke pathology are impaired functioning of the immune system, regular hypothermia, a history of multiple abortions, surgical interventions, the use of an intrauterine device, and disruption of the natural microflora.
The disease is accompanied by intense pain in the lower abdomen, radiating to the sacrum or lower back, and intense purulent or mucous discharge. The pain intensifies when urinating. There are also complaints about deterioration in general health, the presence of intermenstrual bleeding. Therapy begins with treatment of the cause that provoked the oophoritis. They use medications with anti-inflammatory, antibacterial effects, as well as general tonic and immunomodulatory agents. During treatment it is recommended to abstain from sexual intercourse.
Salpingo-oophoritis
Salpingo-oophoritis is a pathological process in which the fallopian tubes and ovaries become inflamed. One of the main reasons that leads to infertility. Develops under the influence of infectious pathogens: chlamydia, gonococci, mycoplasma, staphylococcus, Escherichia coli, streptococci. It is observed in women who are subject to regular hypothermia, overwork, stress, abortion, and multiple births.
The disease is accompanied by pain in the lower abdomen, which persists both during physical activity and at rest. Vaginal discharge with an unpleasant odor and green color is observed, and body temperature rises. A woman complains of nausea, general weakness, libido and menstrual cycle disorders. During therapy, antibiotics, anti-inflammatory drugs, and physiotherapy are used.
Adnexit
Adnexitis is an inflammatory process that affects the uterine appendages. Leads to simultaneous inflammation of the fallopian tubes and ovaries, provokes adhesions. The causative agent of the disease is pathogenic microorganisms (chlamydia, gonococcus, streptococcus, staphylococcus). The disease is accompanied by pain, discomfort during menstruation, increased body temperature, weakness, and increased fatigue. For purulent forms of the disease, surgical intervention is indicated. In other cases, therapy is carried out in a hospital setting with antibiotics and painkillers.
Why and how to do an ultrasound of the fallopian tubes: preparation and interpretation
Examination of the condition of the uterus and fallopian tubes is extremely important not only because it is a matter of the woman’s health, but also a matter of the health of the possible child.
Hysterosalpingoscopy (this is the name of this procedure; otherwise - USGSS ) is one of the medical diagnostic procedures. Ultrasound of the fallopian tubes is a modern way of studying these organs for patency.
The examination is carried out using ultrasound and contrast fluid.
When is it prescribed?
It is recommended to undergo an ultrasound to determine the patency of the tubes if:
- a woman has been diagnosed with infertility (both primary and secondary);
- the menstrual cycle is irregular;
- inflammation of the uterus is chronic;
- no periods, but pregnancy is excluded;
- the patient has pain in the lower abdomen;
- the woman has been treated for any of the sexually transmitted infections (especially if the treatment was not completed).
What will it show?
With traditional ultrasound, it is impossible to assess the condition of the tubes in detail (they are not visualized), because their lumen is simply not visible. However, checking the condition of these organs is very important, which is why a special technique has been developed that allows a qualitative examination of the fallopian tubes and shows existing pathologies.
Are fallopian tubes visible on ultrasound?
Usually, the tubular organs of the uterus cannot be seen on ultrasound.
However, if liquid has accumulated in them, then the likelihood of seeing them increases.
But neither adhesions nor internal inflammation can be diagnosed.
These phenomena are not determined due to the lack of ultrasound signs and can only be detected using contrast fluid.
Therefore, to study the patency of the tubes, a special procedure is required, which is accompanied by the introduction of fluid into the uterine cavity .
Preparation
Before determining how passable the tubes are, the patient will need to prepare for an ultrasound examination. To do this, you need to pass several tests:
- flora smear - taken by a gynecologist during an examination;
- general clinical blood and urine tests;
- PAP test (Papanicolaou smear for oncocytology);
- for infections using PCR (for mycoplasma, ureaplasma and chlamydia)
Preparation for such procedures certainly includes a hygienic part - immediately before visiting the doctor, you need to thoroughly clean your genitals (wash yourself or take a shower).
Reference! If the doctor deems it necessary, then 40 minutes before the GSS, antispasmodics can be prescribed.
You also need to clarify which sensor will be used for the study - if transabdominal, then you will need to fill the bladder.
When is the best time to do it?
The optimal period for diagnosing the fallopian tubes is considered to be from days 5 to 20 of the cycle, or more precisely the time before ovulation (on days 8-11). The fact is that during this period the cervix is most dilated, which means the chances of a spasm occurring are reduced. In addition, after menstruation, the endometrium becomes thinner and does not interfere with the procedure.
How do they do it?
Hysterosalpingoscopy is performed in one of two ways: externally (through the abdominal wall) or transvaginally (by inserting a sensor into the vagina).
Progress of the procedure:
- The back of the gynecological chair is lowered, and the woman takes a lying position on it.
- Then a thorough treatment of the cervix and vagina is performed.
- A disposable small-diameter catheter with a balloon at the end is inserted through the neck, which is necessary for fixation.
- Using an ultrasound, the doctor makes sure that the catheter is positioned correctly (a vaginal sensor is used for the procedure).
- A saline solution or a special gel is injected into a woman’s body, which, as it moves through the fallopian tubes, makes it possible to examine their structure (its amount varies from 20-40 ml to 100-110 ml). The procedure allows not only to determine the presence of adhesions, but also to identify inflammation.
The study is carried out on an outpatient basis, and the patient does not need to stay in the hospital after its completion.
1. Ultrasound of the fallopian tubes.
In terms of time, the GSS takes from 10 minutes to half an hour.
Norm and decoding
If the woman is healthy and there are no pathologies in the pelvic area, then the injected contrast liquid should completely remain in the recess of the abdominal cavity (more precisely, between the rectum and the uterus). If there is no fluid there, but it is found in the fallopian tubes and the uterus itself, it means that the patency of the tubular organs is seriously impaired.
Increased diameter
One of the possible pathologies detected during ultrasound of the fallopian tubes is their expansion (scientifically called hydrosalpinx).
Important! Often the disease is a consequence of fluid accumulation, the development of inflammation or impaired blood circulation.
What causes the fallopian tubes to become dilated? The reason may be:
- Hydrosalpinx, both simple and follicular. The first leads to an enlargement of the pipe in only one cavity and occurs in a mild form, but is dangerous with a high probability of complications. Therefore, it is so important to identify the disease in time and completely treat it.
- Salpingitis is an inflammation that occurs in the tubular organs of the uterus.
- Enlargement of the isthmus of the tube.
Advantages and disadvantages of UZGSS
Like any diagnostic procedure, examination of the fallopian tubes has positive and negative aspects, related both to the patient’s comfort during the ultrasound and to its information content.
Minuses
The UZGSS procedure has a number of disadvantages:
- due to spasmodic compression of the uterus and tubes or a large volume of injected fluid, the patient may feel discomfort;
- The cause of obstruction of the gel or saline solution can be not only adhesions, but also severe spasms.
pros
This diagnostic study has clear advantages over other methods for determining tubal obstruction:
- When planning a pregnancy, conception is possible in the same cycle, because unlike X-ray examination, GSS does not lead to irradiation of the genital organs. Therefore, the question “which is better - X-ray or ultrasound examination” does not arise here.
- In some cases, the procedure is a stimulus for the onset of gestation , since the contrast liquid leads to the washing away of the derivative that clogs the tubes. It also separates thin adhesions and activates the work of the fimbria, which captures and promotes the egg.
- The patient does not require hospitalization or a long wait for diagnosis.
- The procedure will not take much time .
- At the same time, it allows us to identify pathologies of the uterus.
- It is performed non-invasively, that is, without punctures of the abdominal skin.
- Painlessness allows you not to resort to anesthesia for ultrasound examination.
Contraindications
Tubal patency testing is contraindicated in:
- bleeding from the uterus;
- inflammation in the pelvis (especially during exacerbations);
- the onset of pregnancy;
- dysplasia and precancerous changes in the cellular structure of the uterus or its cervix.
Where to do it and how much does it cost?
The price of an ultrasound examination of the degree of tubal patency is made up of the costs of three components of the procedure: an intrauterine catheter, contrast fluid and consumables. The total cost of this type of ultrasound ranges from 1,500 to 4,500 rubles.
Reviews
On the Internet you can find different reviews from patients about this procedure. Most women agree that assessing tubal patency was not painful .
Some say that during the examination they experienced practically nothing.
But there are also patients for whom the procedure left the most unpleasant memories - they were in so much pain that they had to resort to the help of antispasmodics or painkillers.
Such a variety of reviews indicates how individual everything is in the context of this examination, because each woman has a different pain threshold.
Conclusion
Hysterosalpingoscopy has been and remains the most effective and popular diagnostic method in determining pathologies of the fallopian tubes. A timely diagnosis procedure under ultrasound control will help avoid bad consequences and quickly restore women’s health.
Source: https://MediGid.com/uzi/organy/malyj-taz/zhenshhiny/matka/matochnye-truby.html
Anatomical and physiological features of the organ
The uterine, or fallopian, tubes are considered a hollow and somewhat elongated paired organ, which is an important part of the female reproductive system. They are located almost horizontally and start from the fundus of the uterus on both sides.
The main functions of the fallopian tubes:
- transportation of eggs and sperm;
- creating favorable conditions for fertilization, development of the zygote and its movement into the uterine cavity.
Normally, each tube begins with the uterine (or interstitial) section, which is enclosed in the thickness of the myometrium and has a length of about 15-30 mm. Outside the uterus, the organ passes into the isthmus (isthmic section) - a thin horizontal canal in the leaves of the broad ligament, having a length of 27-40 mm. The isthmus is followed by the ampulla. It occupies about 50% of the entire length of the pipe and ends in a kind of funnel, on which there are narrow and long villi - fimbriae. The latter capture the egg released into the pelvic cavity as a result of ovulation and transfer it to the tube.
In women of reproductive age, the average length of the fallopian tube ranges from 100-120 mm, and its thickness is 5 mm. At the same time, according to statistics, the left tube is slightly shorter than the right one.
Types of fallopian tube obstruction
Many women have a huge number of questions after undergoing a fallopian tube diagnosis. The results of the study often contain terms that are incomprehensible to the average person: the fallopian tubes are not located (not visualized), the fallopian tube is dilated, long fallopian tubes, the mouths of the fallopian tubes are closed.
What does all this mean? Each of these pathologies has its own root cause and the treatment is different in each case.
In order to prescribe the correct treatment, experts classify fallopian tube infertility according to several criteria: by the side affected, the level of blockage of the lumen, the cause of blockage and the degree of blockage of the lumen of the fallopian tube.
The affected side. The fallopian tubes are a paired organ, so it is necessary to take into account which of the tubes is obstructed.
There are also two main variations in the classification of tubal obstruction: unilateral and bilateral.
With unilateral obstruction, only one tube is affected, therefore the possibility of conception remains, although it is reduced by half. With bilateral obstruction, conception is impossible.
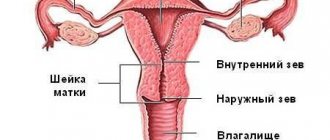
Level of lumen blockage. The fallopian tube is conventionally divided into four sections: intramural, isthmus, ampullary and infundibulum.
For convenience, experts also classify obstruction depending on the level at which the lumen of the fallopian tube is closed.
If, for example, the fallopian tubes are not visualized during diagnosis, then the blockage most likely occurred at the intramural level (often this means that the mouth of the fallopian tube is closed, or a sphincter spasm has occurred).
Cause of blockage. To treat obstruction, it is important to know the cause of its occurrence, so the causes are divided into two groups: functional and anatomical.
For an anatomical reason, for example, a tumor in the fallopian tube or pathology of the mucous membrane, etc. can be diagnosed.
For a functional reason, there may be, for example, excessively long fallopian tubes with sluggish peristalsis, or tubes with a partial absence of mucosa that have lost the function of transporting the egg.
The degree of closure of the lumen of the fallopian tube. There are two degrees of obstruction: partial and complete. If the lumen is completely closed, conception is excluded. With a partial degree, narrowing occurs rather than obstruction, but the fertilized egg cannot overcome this narrowing, but the sperm may well.
Therefore, this pathology is often associated with an increased risk of ectopic (tubal) pregnancy, which can lead to rupture of the fallopian tube (if not consulted in a timely manner), or, depending on the stage of pregnancy, removal of the fallopian tube or dissection of the fallopian tube to extract the fetus.
Any of these situations carries negative consequences.
Why fallopian tubes are not visualized on ultrasound
Normally, these structures are so thin and small that the resolution of most devices simply does not allow them to be examined using ultrasound. In addition, the pipes constantly make floating movements.
With the transvaginal technique , provided that a sufficient amount of fluid accumulates in the pelvis, it is sometimes possible to “catch” this organ. Normal pipes have a uniform structure; the muscle layer and lumen are not determined. In some cases, the doctor may see the ampullary segment with fimbriae.
That is why, to assess the condition of the “appendages” of the uterus, hydrotubation, or hysterosalpingoscopy, is performed.
Causes of disorders in the reproductive system
In a significant number of cases, pregnancy may not occur due to lack of patency of the fallopian tubes. Causes of pathology:
- anomalies in the development of internal organs of the reproductive system ( bicornuate, rudimentary uterus , etc.);
- inflammatory processes on the part of the uterine appendages ( oophoritis, salpingo-oophoritis, adnexitis );
- adhesive disease in the pelvic area as a result of peritonitis after surgery;
- widespread endometritis (inflammation of the inner lining of the uterus) as a complication of abortion;
- interrupted or surgically terminated ectopic pregnancy.
Are fallopian tubes visible on a pelvic ultrasound: normal – no; their full examination is possible provided that a contrast agent is injected into the uterus. This study is called hysterosalpingoscopy, it is carried out according to strict indications and in the absence of pregnancy, acute inflammation or tumors of the genital organs, or uterine bleeding. The procedure is performed by gynecologists using an ultrasound machine, a special catheter and a contrast agent.
Source
Methodology
The ultrasound examination technique is quite simple and absolutely painless. In addition, ultrasound, contrary to popular myth, is a safe technique, which is why it is used for diagnosis during pregnancy.
During pregnancy, ultrasound is performed at the very beginning, when there is a delay in menstruation. Also, the study is carried out as planned at the beginning and each trimester, and in the presence of pathologies it can be carried out several times more often.
With a conventional ultrasound, if there is no development of pathological processes or accumulation of fluid in the pelvic cavity, then the fallopian tubes are not located, that is, they are not visible. There are special techniques for determining the patency of the fallopian tubes. How to check the fallopian tubes for patency and why is this necessary?
Sometimes, under the influence of many reasons, among which the factor of inflammatory processes prevails, the adhesive process is activated in the fallopian tubes. Adhesions connect the walls of the fallopian tubes to each other, blocking, significantly or completely, the lumen in the tubes.
As a result, the patency of the fallopian tubes is disrupted. This situation manifests itself as nagging pain in the lower abdomen from the affected tube, menstrual irregularities, and infertility develops.
If the lumen of the fallopian tube is not completely closed, there is a risk of ectopic pregnancy. The fertilized egg cannot penetrate the uterine cavity, where it should attach to the endometrium and develop further, but remains in the fallopian tube and begins to grow
When the egg reaches a certain size, signs will appear:
- pain from the affected organ,
- delayed menstruation (or scanty spotting),
- nausea,
- headache.
In the future, the fallopian tube may rupture and peritonitis will develop. This is a life-threatening situation.
Therefore, representatives of the fair sex who are planning a pregnancy or have problems with the reproductive system are recommended to undergo a procedure for checking the patency of the fallopian tubes. There are two ways to do this.
Hydrosonography
The procedure is carried out under ultrasound control. The patient is placed on a gynecological chair, legs bent at the knees. A speculum is inserted into the vagina. Then the cervix and vagina are treated with antiseptics. A catheter is inserted through the cervical canal of the cervix into the uterine cavity.
The next step will be the introduction of saline solution into the uterine cavity. The fluid will first enter the uterus and then pass through the fallopian tubes. It is the process of fluid passing through the pipes that is monitored using ultrasound. The procedure itself lasts approximately 25-30 minutes, ultrasound control can be carried out transabdominally and transvaginally.
We invite you to familiarize yourself with Fetal Doppler - everything about ultrasound of pregnant women with Doppler
The examination is prescribed from 7 to 21 days of the menstrual cycle; the most effective period is considered to be the period from 8 to 12 days of the cycle (before ovulation). At this moment, the lumen of the cervical canal opens, which facilitates the insertion of the catheter. However, the individual characteristics of each woman’s cycle should be taken into account.
Directly on the day of the study, it is recommended to take an antispasmodic agent (Spazmalgon, No-shpa). You need to have a sanitary pad with you, as spotting may occur. The consequences of the procedure may be accompanied by minor nagging pain in the lower abdomen and the presence of discharge.
Together with determining the patency of the fallopian tubes, the condition of the uterus (fibroids, polyps, endometritis, etc.) can be determined. The procedure does not require a long hospital stay or anesthesia.
There is a range of contraindications:
- The procedure cannot be performed if the patient has uterine bleeding.
- Inflammatory processes in acute or other forms are a direct contraindication.
- Pathological conditions of the cervix, vagina.
- Pregnancy.
X-ray
Preparation, testing and carrying out the procedure are completely identical to hydrosonography. Only instead of saline solution, a special contrast agent (urografin, verografin) is administered, and instead of ultrasound control, an x-ray is taken.
The procedure can be carried out throughout the menstrual cycle; to determine the patency of the fallopian tubes, it is better to choose the second phase of the cycle.
After the procedure, moderate pain in the lower abdomen and spotting will appear. This is normal (the contrast agent comes out). However, if the pain does not stop after three days, the discharge intensifies, and an increase in temperature appears, you should consult a gynecologist.
The dose of X-ray radiation with this examination method is insignificant, but it is worth protecting against the occurrence of conception during one menstrual cycle (precautionary measure).
Before the procedure, it is necessary to do a pregnancy test and ultrasound control (for the same reason). There are also contraindications.
The procedure cannot be performed if:
- There is an allergic reaction to the contrast agent.
- Inflammatory processes of the reproductive organs.
- Pregnancy.
- Uterine bleeding.
- Tumors, cysts.
- Thyroid diseases.
The choice of examination method remains with the specialist. If you experience pain in the lower abdomen, irregular cycles, heavy discharge or other disturbing symptoms, contact your gynecologist. Timely examination and treatment are the key to your health.
Diagnosis of the condition of the female reproductive system includes a medical examination, a hormonal panel and an ultrasound examination. Many women are interested in if the fallopian tube is not visualized on an ultrasound, what does this mean, how important is this study.