Reproductive organs in women
The female reproductive system is represented by the mammary glands, located on the front surface of the chest, and the pelvic organs.
These are interconnected structures necessary for conception, bearing a child and the development of the body as a whole. Hormones secreted by the endocrine glands control the functions of the reproductive system and maintain the constancy of the internal environment of the body. Many structural diseases of the female reproductive system are caused by a disorder of endocrine regulation. The main organs of the female reproductive system are the ovaries. These are paired sex glands located in the pelvic cavity. The ovaries are connected to the uterine cavity using the fallopian tubes. The organs are formed by connective tissue, cortex and follicles. The key period of ovarian development is puberty, during which sex hormones cause the maturation of organs.
Functions of the ovaries:
- Formation of female germ cells. During ovulation, a mature egg is released from the follicle of the organ and enters the fallopian tube, where the fusion of male and female germ cells occurs to form the rudiment of a new organism. The embryo migrates into the uterine cavity and attaches to the endometrium. If fertilization does not occur, the egg is destroyed, and the functional layer of the uterus is renewed. All these processes occur during the menstrual cycle.
- Release of sex hormones. The follicle from which the egg is released turns into the corpus luteum. This structure begins to produce hormones that prepare the reproductive system for bearing a child. Estrogens, androgens and progestins secreted by the ovaries are necessary to regulate the functions of the genital organs and other anatomical structures.
The ovaries gradually change with age. There is a decrease in the number of active follicles and a change in the volume of hormone production. After the onset of the last menstrual cycle (menopause), the reproductive functions of the organ are reduced.
Is it always necessary to treat?
Observation is indicated only for functional formations - follicular and luteal cysts. It does not matter significantly what size the lesion is if the pathology was detected for the first time. The waiting period is 3 months. During this time, the functional cyst should resolve. If this does not happen, the formation must be removed.
In some cases, the doctor may recommend taking hormonal medications to speed up the regression of the lesion.
Organic cysts - dermoid, serous, paraovarian - can only be treated surgically. Observation is not indicated even with minimal lesion sizes. Such an education is not capable of regressing on its own.
Organic ovarian cysts can only be eliminated by surgical removal.
An exception is made only for asymptomatic cysts up to 3-4 cm in diameter when a woman is planning a pregnancy and does not want to undergo surgery. In most cases, such formations do not interfere with the conception and bearing of a child, and surgical treatment is carried out after childbirth.
Classification
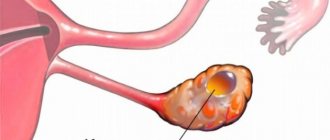
Gynecologists know several types of ovarian cysts, differing in size and content. The size of the smallest formations does not exceed a few millimeters, while large cystic structures can reach 15-20 centimeters. Classification of the disease is necessary to assess possible complications and select treatment methods.
Main types:
- A follicular cyst is a small structure with liquid contents, the walls of which are formed by a reduced follicle. This pathology is formed due to hormonal imbalance. The abnormal follicle may continue to fill with fluid and enlarge.
- Corpus luteum cyst is a pathological structure that forms in the later stages of the menstrual cycle. Normally, the corpus luteum is reduced after performing its own functions, but an endocrine disorder can provoke the growth of a cyst, filling the structure with gland secretions.
- A dermoid cyst is a structure that may contain hair, skin, teeth, and other tissue. The reason for the formation of such a disease is a violation of the regulation of embryonic cells. In rare cases, the contents of such a cyst turn into a malignant tumor. Large dermoid cysts often cause peritonitis.
- Endometrioid cysts. This type of disease is formed during the migration of cells in the inner lining of the uterus. The contents of such a cyst are usually represented by clotted blood.
- Cystadenomas are a benign tumor-like structure consisting of epithelial tissue. The contents of a cystadenoma can be represented by watery fluid.
The doctor may need biopsy results to determine the type of pathology.
Acceptable sizes
The danger of an ovarian cyst lies in the property of the formation itself to grow from a few millimeters to 10-12 centimeters. In some cases, hollow tumors can grow up to 20 cm in diameter. An ovarian cyst with such parameters can be detected already during palpation performed by a gynecologist.
For medical reasons, conditionally safe . However, drug treatment and periodic examination by a gynecologist remain a mandatory requirement.
This size of the cyst is considered critical, since even if cystic formations with a diameter of about 6 cm are detected, there is a risk of further complications and only a doctor can decide how dangerous this is and what to do next in each individual case.
As a rule, an examination by a gynecologist is carried out every 3-4 weeks to monitor the behavior of the pathology itself.
Causes
Benign ovarian structures can be independent diseases or complications of other pathological processes. The exact mechanisms of cyst formation are unknown, but scientists associate this pathology with the functioning of the endocrine system, the regulation of embryonic cells and the functions of the ovaries.
Possible reasons:
- A hormonal disorder that occurs due to the early onset of menstruation, ovulation disorders and functional ovarian failure. At the same time, the level of hormones that control the reduction of the follicle and corpus luteum may decrease,
- Surgical interventions in the pelvic area, such as artificial termination of pregnancy.
- Pathologies of the endocrine organs: underactive thyroid gland, adrenal gland disorder.
- Inflammatory and infectious diseases of the ovaries.
- Congenital disorders of ovarian development associated with the influence of genetic mutations.
Clarifying the cause of the pathology allows you to select the most effective treatment.
Kidney cyst 4 cm - is it big?
This size for a kidney cyst is considered quite large, since a neoplasm with a diameter of 40 mm disrupts the functioning of the organ. In a certain area of the kidney, the formation and outflow of urine changes. Blockage of the tubules, stagnation of urine, and accelerated development of kidney infection may occur.
Such a cystic structure is dangerous and requires systemic treatment if it manifests itself with pathological symptoms:
- pain in the lumbar region due to a cyst on the kidney measuring 4 cm;
- disturbances in the outflow of urine, painful urination;
- fever, even if it is subfebrile 37-38℃, and even more so if the temperature rises higher;
- hypertensive crises.
If a kidney cyst of 4-5 cm is silent and does not reveal itself except on ultrasound, then it needs to be observed and a puncture done if it grows further. We wrote in detail about lifestyle with a kidney cyst in one of our previous articles.
Risk factors
Doctors also take into account the influence of various pathological factors on functional tissue (of the ovary). Various forms of predisposition to the disease may be associated with the patient’s lifestyle, individual history and heredity.
Possible risk factors:
- diseases of the reproductive organs, such as endometrial growth;
- infections and injuries of the pelvic cavity organs;
- late onset of menopause;
- detection of a cystic ovarian lesion in a close relative of the patient.
Taking into account risk factors is necessary for prevention.
Pathogenesis
On average, the menstrual cycle lasts 28 days. In the first phase of the cycle, a large amount of follicle-stimulating hormone is released, which is necessary to prepare the ovary for ovulation. As a result, one dominant follicle in the ovary matures, accompanied by the production of estrogen and luteinizing hormone. Ultimately, this leads to the release of the female reproductive cell into the fallopian tube. With excess production of follicle-stimulating hormone and deficiency of luteinizing hormone, a follicular cyst forms in the ovary. Continuous endocrine stimulation provokes subsequent growth of this formation. Preservation of the cells lining the follicle in the cyst can lead to excessive production of estradiol and disruption of the menstrual cycle.
Normally, the absence of fertilization within 14 days after ovulation provokes a reduction of the corpus luteum. If pregnancy occurs, the corpus luteum continues to secrete progesterone for 5-9 weeks, until its final destruction at 14 weeks. If the reduction of this structure is disrupted, a cyst is formed in place of the corpus luteum. Rupture of this formation is accompanied by bleeding and acute pain.
Clinical picture of the disease
The size of the cyst affects the symptoms of the pathology. Small formations up to 30 mm in size (the size of a quail egg) usually do not manifest themselves. A woman may not know there is a problem until she has an ultrasound. Often we are talking about functional cysts that resolve safely without the use of medications.
A gynecological ultrasound is performed on the 5-7th day of the cycle (unless the doctor recommends otherwise). During examination, lesions ranging in size from 2-3 cm are clearly visible. Small formations are not always visible during ultrasound and are often indistinguishable from normal follicles.
Medium lesions measuring 3-6 cm (the size of a chicken egg) can manifest themselves with the following symptoms:
- Menstrual irregularities. With functional formations, there is a delay in menstruation, after which prolonged and heavy bleeding occurs. Endometrioma produces spotting before and after menstruation. Other cysts do not affect the menstrual cycle;
- Uterine bleeding is observed mainly against the background of endometrioma. This pathology is often combined with a hyperplastic process of the endometrium;
- Nagging pain in the lower abdomen is characteristic of any type of formation.
A sign of the presence of a cyst may be nagging pain in the ovarian area.
Large cysts are characterized by the following symptoms:
- Pressure on the pelvic organs leads to constipation, bloating and urination problems;
- Increase in size of the abdomen due to growth of formation.
The largest ovarian cyst was removed in 1991 in California from a 36-year-old woman. The formation weighed 137 kg. It reached this level in 2 years. Dr Catherine O'Hanlan, head of the surgical team, said the patient was afraid of the operation and did not see doctors for a long time. Removing the giant cyst took 6 hours.
In 2021, a complex operation was performed in Mexico to remove a cyst weighing 33 kg. The diameter of the formation was about 150 cm. Dr. Eric Hanson Viana, who performed the operation, points out that this is the only case in the history of medicine when a cyst of this size could be removed without pumping out fluid from it or damaging the capsule.
Symptoms
In most cases, the disease does not manifest itself symptomatically. However, some cystic structures can interfere with ovarian function and cause discomfort.
Possible symptoms and signs:
- pain in the lower abdomen on the side of the affected ovary (right or left abdominal region);
- feeling of heaviness in the abdomen;
- bloating;
- nausea;
- irregular and heavy uterine bleeding;
- lack of ovulation;
- male pattern body hair growth;
- asymmetry of the abdomen.
Asymptomatic cysts are detected during a gynecological examination. If you experience severe abdominal pain, dizziness, vomiting and pale skin, you should seek medical help, since such symptoms may indicate rupture of the cyst membrane and bleeding.
4 cm breast cyst – how dangerous is it?
The size of a breast cyst is difficult to accurately compare with its age. A 40 mm bubble can develop in a few months or in 2-3 years. The lifespan of a cystic structure in the breast is determined by the density of the capsule. Solid neoplasms with a diameter of 4 cm, which are easily palpable, formed quite a long time ago. But recent ones will have soft walls and are more difficult to detect.
Breast cysts appear due to hormonal disorders, obesity, injuries, and also after the introduction of silicone implants.
Breast cyst 4 cm - is it big or not? The average size of such formations is 6 cm, so a bubble with a diameter of 40 mm can be considered not the largest. But it will already be clearly visible with breast sizes 0-4. It can rupture when dropped or hit and become infected. Therefore, fluid from the cyst cavity must be removed by puncture.
What are the prognoses for such a neoplasm?
- A 4 cm breast cyst is not life-threatening; such structures rarely degenerate into malignant ones. But there is a risk, so observation by a mammologist is necessary.
- And at the stage of 40 mm, and especially with further growth, the bubble will compress the surrounding areas and cause pain.
- Pain in the breast with a cyst will intensify before the onset of menstruation.
- If left untreated, inflammatory complications may occur, which will require surgery to remove the cyst.
Diagnostics
If symptoms of the disease appear, you must make an appointment with a gynecologist. The doctor will ask the woman about her complaints and examine her medical history to identify risk factors for the disease. The next stage of diagnosis is a general examination of the pelvic organs, including palpation of anatomical structures. If signs of cystic ovarian lesions are detected, the gynecologist prescribes instrumental and laboratory tests.
Additional diagnostics:
- Ultrasound examination. The doctor inserts a special probe into the vagina to obtain images of the ovaries. Reflections of ultrasonic waves create images of organs on the monitor. Ultrasound of the ovaries is the most reliable method for diagnosing cysts. This painless and safe procedure is used for the initial detection of the disease and monitoring the results of treatment. If necessary, the sensor is inserted through the anterior abdominal wall (transabdominal access).
- Puncture of the posterior vaginal vault (culdocentesis). This safe diagnostic procedure is necessary to detect complications of the disease. The doctor treats the skin of the vaginal vault with an antiseptic, numbs the tissues and pierces the skin with a long needle. Aspiration of the free contents of the small pelvis is carried out. The abdominal cavity may contain blood or exudate. The resulting material is examined in the laboratory to exclude the presence of abnormal cells.
- Blood analysis. In the treatment room, a nurse collects venous blood and sends the material to the laboratory. Specialists evaluate the quantity and ratio of formed elements, and also determine the concentration of sex hormones. This analysis is necessary to determine the cause of the disease. Also, specialists can detect an oncological marker in the patient’s blood, indicating the growth of a malignant neoplasm in the ovary.
- Diagnostic laparoscopy is a minimally invasive surgical procedure. The doctor treats the skin of the surgical field with an antiseptic, performs anesthesia and makes a small incision in the area of the anterior abdominal wall. Instruments are inserted into the resulting hole to examine the ovary and abdominal cavity. If necessary, the surgeon removes the ovary. Histological examination of the removed organ allows for an accurate diagnosis.
- Computed tomography or magnetic resonance imaging are the most accurate methods of visual diagnosis. The patient is asked to remove metal objects, lie down on the tomograph table and remain still. The results of CT and MRI are layer-by-layer images of anatomical structures, making it possible to assess the location and size of the pathological area.
Diagnostic methods depend on primary clinical data. The gynecologist must rule out diseases with similar symptoms, such as ectopic pregnancy.
Pathological and normal cyst sizes
The conventional norm is considered to be a capsule volume of up to 2 cm. Exceeding this figure can be considered as a potentially dangerous formation for women’s health, since the development of such conditions as:
- shell rupture;
- leg torsion;
- suppuration;
- development of hemorrhage and others.
The size of an ovarian cyst is considered large if it exceeds 6 cm in diameter. Many experts recognize such formations as dangerous, but it all depends on its type.
It is important to remember that a large ovarian cyst, if ruptured, can cause massive internal bleeding.
An ovarian cyst of 2 cm in volume does not pose a particular danger to women’s health. For example, if it is a follicular variety, then it will resolve on its own within one to three menstrual cycles.
Most often, cystic formations of this size are treated with medication. The woman is prescribed hormonal medications.
Treatment of ovarian tumors with a volume of 3 cm is carried out with the help of medications. Hormone therapy was recommended for the patient. Surgery is practiced when necessary.
An adnexal cyst on the left or right ovary of 4 cm is most often a parovarian neoplasm. It tends to increase and can reach significant volumes.
Dangerous for a woman, as it can be complicated by torsion of the leg. Symptoms of the condition include:
- cramping pain localized in the lower abdomen;
- attacks of nausea and vomiting;
- increased body temperature;
- tachycardia;
- tension of the anterior abdominal wall.
If such symptoms develop, the woman is recommended to undergo urgent surgical intervention.
When diagnosing an ovarian cyst measuring 5 cm, you must regularly visit the gynecologist’s office. This should be done once every six months. The patient is recommended to periodically determine hormonal levels, which makes it possible to monitor changes that have occurred.
An ovarian cyst of 6 cm is considered large. Quite often, gynecologists take a wait-and-see approach, monitoring changes in the patient’s general health.
To determine how dangerous this neoplasm is for her, a woman is prescribed additional examinations:
- blood and urine tests;
- CT and/or MRI;
- blood test for tumor markers;
- puncture;
- diagnostic laparoscopy.
Based on the results obtained, the doctor decides whether to perform removal surgery or not.
Treatment
The choice of treatment regimen depends on the woman’s age and individual medical history. It is necessary to prevent the development of complications and preserve reproductive functions. For small functional cysts, the gynecologist prescribes drug therapy and constant monitoring.
Medication prescriptions:
- Oral contraceptives are medicinal substances that affect the level of female sex hormones. The gynecologist prescribes a course of such medications for approximately 2-3 months. The condition of the cyst is regularly monitored using ultrasound of the pelvic organs.
- Additional medications: vitamin complexes and painkillers.
In parallel with drug treatment, the gynecologist may prescribe physical therapy. These procedures prevent the development of the inflammatory process and eliminate pain. If conservative treatment does not produce results, surgery is prescribed. Laparoscopic operations allow the removal of pathological structures with minimal risks.
Surgical treatment options:
- Removal of the cyst while preserving healthy ovarian tissue. The surgeon carefully removes the pathological formation and eliminates the resulting hemorrhage. This operation allows you to preserve the reproductive functions of the organ.
- Radical removal of the ovary. This treatment is prescribed for very large cysts, complications of the disease, and if a malignant neoplasm is suspected.
- Removal of the ovaries, uterus and cervix of the organ to prevent malignant tissue degeneration. This treatment is usually prescribed to women over the age of 50, when there is no need to preserve reproductive function.
After treatment, rehabilitation is carried out. The gynecologist regularly prescribes examinations to exclude postoperative complications.
Ovarian cyst
Signs
In some women, an ovarian cyst does not manifest itself at all.
It is discovered accidentally during an ultrasound. For others, it causes sharp pain in the lower abdomen during sexual intercourse or physical activity, frequent urination, nausea, vomiting, tachycardia, high temperature (38-39°C) and weight gain. The cyst does not always affect the menstrual cycle. It is found in 30% of women with regular periods and in 50% of women with cycle disorders. After menopause, the likelihood of developing an ovarian cyst decreases.
Description
The ovaries are a paired organ measuring from 1.5 to 5 cm. They are located on the sides of the uterus and perform endocrine (produce female sex hormones - estrogens and progesterone and a small amount of androgens) and generative (form female reproductive cells - eggs). The ovary is divided into a cortex and medulla. The cortex contains large spherical sacs approximately the size of a pea. These are follicles in which eggs mature. The ovarian medulla is connective tissue with blood vessels and nerves. Disruption of the ovaries can lead to the formation of an ovarian cyst.
An ovarian cyst is a benign hollow formation in the ovarian tissue filled with fluid. They develop, as a rule, from a maturing follicle due to the accumulation of secretions in the ovarian tissue. This secretion is produced by cells that form the walls of the cyst. The cyst can reach 10-12 cm in diameter.
Cysts are divided into:
- Follicular, which are formed if ovulation (the release of a mature egg from the ovary into the abdominal cavity) does not occur for some reason. This type of cyst occurs most often in girls during puberty. On average, such a cyst reaches 5-7 cm in diameter. If it reaches more than 8 cm, there is a danger of torsion of its legs, rupture of the cyst and necrosis of the ovary. Small cysts (up to 4 cm) are not treated. But the patient should periodically do an ultrasound to monitor the behavior of the cyst. As a rule, such cysts disappear after 1.5-2 months. Sometimes taking oral contraceptives can speed up this process.
- Corpus luteum cysts. A mature egg ruptures the follicle and exits, as we have already written, into the abdominal cavity, from which it is sucked into the fallopian tube. And in place of the follicle, a corpus luteum is formed, which produces estrogen and progesterone. If pregnancy does not occur, it normally resolves. But it may happen that it does not resolve, but fills with fluid or blood. It is from this formation that a corpus luteum cyst arises. Its diameter does not exceed 6-8 cm. And after 2-3 months this cyst usually resolves. However, if the cyst stalk is twisted, it may rupture. In this case, urgent surgical intervention is required. Surgery is also performed if the cyst has reached a large size. In other cases, medication and physiotherapy are sufficient.
- Paraovarian, located in the mesentery of the fallopian tube. They develop from the epididymis. Most often, women over 30 years old face this problem. Despite the fact that such a cyst grows slowly, it can reach 20 cm in diameter. Clinically, this neoplasm may not manifest itself in any way: the cyst is inactive and causes almost no anxiety to the woman. But due to its size, it puts pressure on neighboring organs - the bladder and rectum. Treatment is only surgical.
- Dermoid, containing hair, hair follicles, sebaceous glands. All this floats in a mucus-like liquid and is enclosed in a thick-walled capsule, the inner surface of which is lined with stratified squamous epithelium. It can reach 15 cm in diameter. A dermoid cyst is a congenital formation that occurs at the site of fusion and fusion of embryonic furrows and cavities due to impaired development of the embryo. Despite the fact that this cyst exists from birth, it can manifest itself at any age. Ovarian dermoid cyst occurs most often in girls during puberty. In 5-8%, a dermoid cyst can develop into a malignant tumor. The treatment of such a cyst at any period of its development is only surgical.
- Endometriotic, formed when the endometrium penetrates the ovaries. These cysts are bilateral. Often, along with the ovaries, neighboring organs are also affected - the bladder, ureter, and intestines. These cysts can be from 4-5 to 15-20 cm in diameter. At first they do not manifest themselves in any way, but then small holes appear in them, through which the contents flow into the abdominal cavity. This may cause adhesions. Treatment is only surgical.
Many factors can trigger the development of an ovarian cyst. This includes the rhythm of life of a modern woman, diet, and working conditions. Anything that affects the functioning of the endocrine system can also lead to the development of ovarian cysts. Only a timely visit to a gynecologist can help get rid of a cyst without unpleasant consequences.
Unfortunately, complications of the disease are also possible. These include:
- Torsion of the cyst stalk. This complication occurs with sudden movements or rapid changes in body position. When the leg is twisted, the nutrition of the cyst is disrupted and necrosis begins. The patient's condition is rapidly deteriorating, the skin and mucous membranes turn pale, sharp abdominal pain appears, blood pressure decreases and the temperature rises.
- Cyst rupture. May occur due to rough examination or mechanical trauma. At the same time, due to internal bleeding, blood pressure drops, spots flash before the eyes, dizziness and nausea. There are sharp pains in the abdomen, radiating to the rectum.
- Suppuration. When the cyst suppurates, the temperature rises and pain in the lower abdomen appears, similar to pain in acute adnexitis. The abscess can adhere to neighboring organs or break into the bladder or rectum, forming fistulas.
- Malignancy is the most dangerous complication of an ovarian cyst. Moreover, among all gynecological diseases, the ovarian cyst ranks first in predisposition to cancer, ahead of even uterine fibroids. Therefore, women with this diagnosis must be carefully monitored to prevent malignancy.
Many women are against surgical intervention, but if an ovarian cyst is diagnosed and there is a possibility of complications, it is better to “surrender” to the surgeon, because it is unknown when and under what conditions a complication will occur and whether they will be able to help you in time.
Diagnostics
The first stage of diagnosis is a gynecological examination. If the doctor, based on complaints and examination, suspects the patient has an ovarian cyst, he sends her for an ultrasound, gives a referral for a general analysis of urine and blood, laparoscopy of the cyst, morphological examination of a specimen of ovarian tissue, colposcopy, computed tomography (CT) and does a pregnancy test.
The most informative diagnostic method is ultrasound of the pelvic organs. It is especially effective when using a transvaginal sensor.
General and biochemical blood tests and a general urine test are done to identify inflammation, if any.
Laparoscopy of an ovarian cyst is prescribed if there is a suspicion of rupture of the cyst or torsion of its legs. This manipulation allows not only to diagnose the condition, but also, if necessary, to immediately remove the cyst. It is performed under general anesthesia.
A CT scan is done to distinguish an ovarian cyst from other neoplasms.
A pregnancy test is performed to rule out ectopic pregnancy.
Treatment
Depending on the complexity, size and type of cyst, treatment can be medicinal (conservative) or surgical.
If the situation allows the cyst to be treated with medication, monophasic or biphasic oral contraceptives, vitamins A, E, C, B1, B6, K are prescribed. If the patient is obese, she is recommended diet therapy, balneotherapy and physical therapy. If such treatment does not help, surgical intervention is necessary.
In this case, you first need to find out the nature of the cyst and make sure that the tumor is benign. Most cysts are removed laparoscopically. The operation is performed under anesthesia through small, up to 1.5 cm, incisions in the skin. The abdominal cavity fills with gas. Instruments and a camera are introduced through the holes. It is removed carefully so that the contents are not exposed during the operation. After the operation, a histological examination of the cyst is performed. Usually the patient is discharged from the hospital 2-3 days after surgery.
Prevention
There is no specific prevention for ovarian cysts. To identify changes in the ovaries at an early stage it is necessary:
- monitor hormonal levels, eliminate disruptions to the endocrine system in a timely manner;
- carefully select contraceptives to avoid abortions;
- visit a gynecologist regularly;
- Avoid promiscuity and protect yourself from sexually transmitted infections.
The most effective method of preventing complications of an ovarian cyst is its timely treatment or removal, because any planned operation goes better than an emergency one. In postmenopausal women, in order to prevent the cyst from degenerating into a malignant tumor, the ovaries are removed.
© Dr. Peter
Complications
Without treatment, cystic structures may gradually increase in size. In some cases, a rupture of the cyst shell occurs, releasing the contents of the structure into the abdominal cavity. Extensive inflammation of the peritoneum (peritonitis) is a life-threatening condition, so if you experience severe abdominal pain, vomiting, dizziness and weakness, you should seek medical help. Peritonitis is treated with surgery and drug therapy.
Other complications:
- Infection of a paraovarian cyst. Most often, infection occurs when the cyst stalk is twisted, the blood supply is disrupted, and tissue necrosis occurs. The entry of exudate along with pathogenic microorganisms into the abdominal cavity causes severe peritonitis.
- Reproductive dysfunction: reversible infertility or complication during pregnancy.
- Formation of adhesions in the pelvic area.
Timely diagnosis makes it possible to detect even minor changes in the structure of the ovary in time and carry out treatment.
Types of cysts and their sizes
A cystic tumor is classified into several types and its permissible size is one of the main determination criteria. An ovarian cyst can be:
- Luteal (corpus luteum). Its formation occurs in the post-ovulation period. The internal contents may contain blood particles. The disease itself often occurs without identifying any symptoms. In this case, parameters in the range of 6-8 cm are considered normal.
- Follicular, which is formed in the ovary in the period between the beginning of menstruation and the ovulatory process. Its manifestation is usually accompanied by sharp pain in the lower abdomen, which radiates to the lower back. An acceptable variant of the norm may be a formation of no more than 3 cm, but without appropriate treatment its parameters can increase to 10 cm.
- Endometrioid, which is more often bilateral than others, is distinguished by its location on the mucous membrane of the uterus and the presence of blood particles in the internal contents. Treatment is considered necessary if it is possible to detect an ovarian cyst measuring from 6 to 20 cm. Its minimum diameter is about 4 cm.
- Paraovarian, which is formed from cells of the appendages. In such cases, the size is considered large if the cyst has reached a diameter of 7 cm. Its maximum parameter is limited to 12-14 centimeters.
- Dermoid, which requires mandatory surgical intervention. Only a doctor can tell you how dangerous it is in each individual case. The formation itself has internal fluid, which includes almost all types of body tissue.
According to the nature of the contents, hollow cystic formations can be organic or functional. Only the latter have the property of self-dissolving. In addition, they are more easily affected by medications and can completely disappear after 2-3 cycles of treatment with specially selected hormonal drugs. If there are functional formations no more than 60 mm in diameter, a woman still has the opportunity to become pregnant. The organic type of tumors requires surgical intervention and does not allow for spontaneous resorption.
Prevention and prognosis
In most cases, the prognosis is favorable. Doctors are able to carry out treatment at any stage while maintaining reproductive function. Only in rare cases is it necessary to remove the organ. Many women experience a recurrence of the cyst, but constant use of hormonal therapy helps reduce the risk of such a complication.
Preventive recommendations:
- taking hormonal contraceptives under the supervision of a doctor;
- you should visit a gynecologist regularly;
- Timely treatment of inflammatory and infectious diseases of the pelvis is necessary.
Diagnosis of ovarian diseases is mandatory during pregnancy and preparation for conception. A consultation with a gynecologist will allow a woman to learn more about the prevention and treatment of this disease.