A little physiology
Normally, the endometrium consists of two layers - basal and functional. The main feature of the endometrium is its very high sensitivity to monthly changes in hormonal levels. A new menstrual cycle begins with the rejection of the functional layer of the mucous membrane. Outwardly this is manifested by menstruation. The concentration of hormones is at a functional minimum. After the end of menstruation, the concentration of estrogen, which is responsible for the growth of the endometrium, begins to gradually increase. The functional layer is gradually restored - this is the regenerative phase of the menstrual cycle. At the same time, a follicle matures in one of the ovaries.
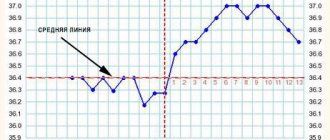
Approximately in the middle of the cycle, when the amount of estrogen is at its peak, ovulation occurs - a mature egg is released into the abdominal cavity, then into the ampullary part of the fallopian tube, where conception occurs.
In place of the burst follicle, a corpus luteum appears, producing progesterone. Under its influence, glands begin to mature in the endometrium - the mucous membrane prepares for implantation of a fertilized egg. If conception does not occur, the levels of progesterone and estrogen begin to gradually decrease. As soon as it reaches a minimum, the functional layer will begin to be rejected again. A new menstrual cycle will begin.
Norms of endometrial thickness in accordance with the day of the menstrual cycle
The main reproductive organ, the uterus, is lined with a functional layer. It is intended for conception, the embryo is attached to it, and through it the embryo is fed with the necessary substances.
The thickness of the endometrium varies by day of the cycle: it gradually increases, is saturated with blood through the vessels and glands, preparing to receive the embryo.
Based on the size of the layer, conclusions can be drawn about the correct functioning of the reproductive system and whether a woman can become pregnant.
Structure and tasks of the endometrioid layer
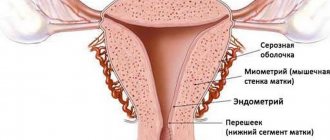
The inner surface of the uterus is lined with tissue consisting of two layers, each of which has its own functionality:
- Basal - penetrated by capillaries, has a static thickness, is responsible for the supply of blood and restoration of the layer following it.
- Functional – controls the process of the menstrual cycle. In the absence of pregnancy, it is this layer that is rejected. It grows again in 28–35 days. The functional layer will suffer significant damage during abortion, curettage and childbirth.
The established norm of endometrium changes by day of the cycle, taking into account the woman’s age, infectious diseases she has suffered, abortions, childbirth and other factors.
Normal embryo implantation and cycle stability depend on changes in the endometrium.
Endometrioid tissue performs the following functions in the uterus:
- prevention of fusion of the uterine walls;
- promoting the attachment of the fertilized egg to the wall of the uterus;
- nutrition supply to the embryo;
- participation in filling the placenta with blood.
Under the influence of hormonal substances, endometrial growth occurs on the days of the cycle in 4 periods:
- Bleeding (desquamation). Parts of the rejected mucosa come out during active contractions of the uterus. The regression of the corpus luteum is recorded and the concentration of hormones quickly drops. The capillaries of the functional layer undergo spasm, and as a result of ischemia of the surface of the layer, it is rejected. The period lasts 1 or 2 days.
- Regeneration. The process takes 3 or 4 days, during which the basal cells restore the destroyed endometrium.
- Proliferation or restoration. When, after the cessation of menstruation, the mucous tissue grows again, the main follicle of the epididymis is formed. The period takes from 5 to 14 days.
- Secretion. The phase got its name due to the filling of the mucous membrane with liquid secretion, which accumulates due to the development of capillaries and glands inside the tissue. It lasts 15–28 days, during which the egg matures and is released from the ovary. Progesterone production begins after the destruction of the follicle and the formation of the corpus luteum.
Table of endometrial norms in millimeters
Taking into account the data on the average diameter of the uterine mucosa, the doctor draws conclusions about the woman’s health status; the normal size of the endometrium by day of the cycle is reflected in the table.
| Stage of tissue development | Exact days of the monthly cycle | Diameter of the functional layer in mm | |
| Bleeding | Desquamation | 1–2 | 4–9 |
| Regeneration | 3–4 | 2–5 | |
| Proliferation | Start 5–7 | 3–7 | |
| Mid 8–10 | 7–10 | ||
| Completion 11–14 | 10–14 | ||
| Secretion | Start 15–18 | 12–16 | |
| Mid 19–23 | 12–18 | ||
| Completion 24–27 | 12–15 |
Decoding table data
The first days are menstruation, the process of bleeding, which normally takes 3–7 days. The rejection phase lasts two days. During menstruation, the normal layer is 5–9 mm. The violation can be noticed by an ultrasound interpretation specialist.
Next, regeneration starts. The diameter of the mucous tissue is now minimal - the endometrium during menstruation is only three millimeters.
The proliferative phase begins by the fifth day and lasts 13–16 days. The volume of mucous membrane increases (in days):
- initial stage – from the sixth to the seventh (5–7 mm);
- middle stage – from the eighth to the tenth (8–12 mm);
- late stage - from tenth to fourteenth (10–14 mm).
In the secretory phase, the functional tissue becomes thicker, increasing in diameter from the initial to the final stage from 12 to 20 mm; by the beginning of menstruation, the mucous membrane thins from 20 to 15 mm.
The endometrium becomes thickest by the first day of the menstrual cycle. Blood vessels swell, the epithelium, in the absence of conception, prepares for rejection.
Menstruation begins when the endometrium is 20 or 21 mm thick, provided that the level of hormones in the woman’s body is stable.
While waiting for her period, a woman may experience stress, physical overload, a cold, or be on a strict diet - all this affects the maturation of the uterine lining. If the listed factors lead to hormonal imbalance, the layer does not grow in accordance with the day of the cycle and the thickness of the endometrium before menstruation will be only 12 mm - 16 mm.
What does an ultrasound show and when to do it?
When a doctor prescribes an ultrasound examination, the day of the monthly cycle, the presence of systemic and gynecological diseases that may affect the result are taken into account.
The patient must undergo an ultrasound no later than 5–7 days of the cycle to find out whether the tissue lining the uterus is performing its functions normally.
It should be taken into account that the norms for endometrial thickness by day of the cycle may differ among different women, so it can be difficult to determine the deviation.
During menstruation, the uterine cavity, according to ultrasound data, expands to 5 mm. The thickness of the endometrium during menstruation ranges from 5 to 9 mm, before it – from 15 to 18 mm. It is impossible to determine exactly because the tissue is rejected.
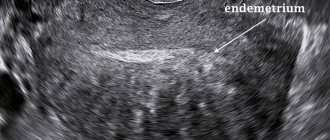
On days 3–7, functional tissue on the walls of the uterus looks like a strip 3–8 mm thick. Further, a thickening of approximately 0.1 mm occurs daily, until ovulation occurs. The average is 7 mm, the maximum is 12 mm. In the period before ovulation, ultrasound determines the following:
- homogeneity of structure;
- the endometrium is hypoechoic;
- The uterine walls are connected in an area with hyperechoic indicators.
After the onset of the ovulatory stage, the thickness of the endometrium reaches from 9 to 13 mm, the structure of the uterus is five-layered, with slightly increased echogenicity.
Using ultrasound, it is possible to determine the thickness of the endometrium by days of the monthly cycle for conception. In the mucous layer, vacuoles and gland ducts are visible in the form of small anechogenic spots. The average size of the functional layer of the uterus, favorable for the reception of a fertilized egg, is from 15 to 16 mm.
This is what the endometrium should look like according to the days of the cycle in healthy women of reproductive age:
- 1–7 – from 3 to 8 mm;
- the endometrium on the 7th–10th day of the cycle is normally 5–12 mm;
- postovulatory period (15–21) – from 6 mm to 13 mm;
- the final period of the cycle (from 22 to 28) – up to 15 mm.
The duration of the cycle is individual for each woman. If it is increased, the rate at which tissue grows will be slower. With a shortened cycle, on the contrary, the mucous layer will become thicker every day.
What is the thickness of the endometrium in women during menopause?
Upon reaching the age of 35, the ovarian reserve of the appendages in women begins to decline, but the first symptoms of decline in reproductive function are noted only at the age of 45. Due to a decrease in estrogen production, the endometrial layer grows more slowly during the days of the cycle.
During menopause, indicators by day of the uterine mucosa are usually at the lower threshold of normal or much lower, and depend on how long ago menopause began:
- less than 5 years – the endometrium grows up to 5 mm;
- more than 5 years – maximum 4 mm;
- more than 10–15 years - the layer is so thin that ultrasound cannot determine its thickness.
Many women, for medical reasons, during menopause undergo a course of hormone replacement therapy, which stabilizes estrogen production. Their number of mm of mucous layer by day may be normal or close to it.
Causes of thin endometrium
To date, doctors have identified several fundamental factors that affect the thickness of the endometrium. The main ones include:
- hormonal imbalance;
- impaired blood circulation in the uterus;
- uterine injuries, including surgical interventions;
- developmental anomalies;
- chronic inflammatory processes in the uterus;
- prolonged and uncontrolled use of contraceptives;
- burdened heredity.
Generally speaking, the hormone estradiol is responsible for the thickness of the endometrium. If the concentration of this hormone is too low, the lining of the uterus will become thinner. As a rule, gynecologists recommend checking the entire hormonal profile. This gives a more complete picture of the patient's health status. If there are deviations, the doctor will advise ovulation stimulation or hormonal correction.
Another reason for hormonal imbalance that prevents the endometrium from enlarging is the absence or insufficient number of estradiol receptors.
The cause of poor circulation may be low blood flow, as well as pathological changes in the pelvic veins. To confirm the diagnosis, you need to consult a phlebologist. He also prescribes treatment.
Of the surgical interventions, the most significant cause of thin endometrium is frequent curettage and abortion. Damage to the basal layer makes regenerative processes impossible. As a result, the mucous membrane becomes thinner. Anomalies of the uterus include a bicornuate uterus, saddle-shaped, and with septa. In addition, thinning of the endometrium can be observed with fibroids, polyps, and adhesions. Confirm the diagnosis using ultrasound. In controversial and difficult situations, computed tomography or magnetic resonance imaging is recommended. Treatment is surgical or conservative, depending on the situation.
Chronic inflammatory processes in the uterine mucosa can lead to its thinning. As a rule, an accurate diagnosis is made after hysteroscopy with biopsy and pathomorphological examination of the biopsy. Long-term use of oral contraceptives or other sex hormones without a doctor’s recommendation and proper monitoring leads to an imbalance in the hormonal balance in the body and, as a result, thinning of the endometrium. The role of heredity in thin endometrium has not been sufficiently studied. However, some authors argue that it plays an important role.
Phases of endometrial proliferation
It is usually difficult for women to understand what the phases of endometrial proliferation are and how a violation of the sequence of stages is associated with health. Knowledge about the structure of the endometrium helps to understand the issue.
The mucosa consists of a ground substance, a glandular layer, connective tissue (stroma) and numerous blood vessels. From about the 5th day of the cycle, when proliferation begins, the structure of each of the components changes. The entire period lasts about 2 weeks and is divided into 3 phases: early, middle, late. Each stage of proliferation manifests itself differently and takes a certain time. The correct sequence is considered the norm. If at least one of the phases is absent or there is a malfunction in its course, the likelihood of pathologies developing in the lining inside the uterus is very high.
Early
The early stage of proliferation is days 1-7 of the cycle. The mucous membrane of the uterus during this period begins to gradually change and is characterized by the following structural transformations of tissue:
- the endometrium is lined with a cylindrical epithelial layer;
- blood vessels are straight;
- the glands are dense, thin, straight;
- cell nuclei have a rich red color and oval shape;
- the stroma is oblong, spindle-shaped.
- The thickness of the endometrium in the early proliferative phase is 2–3 mm.
Average
The middle stage of the proliferative endometrium is the shortest, usually on the 8th–10th day of the menstrual cycle. The shape of the uterus changes, noticeable changes occur in the shape and structure of other elements of the mucosa:
- the epithelial layer is lined with cylindrical cells;
- the kernels are pale;
- the glands are elongated and curved;
- connective tissue of loose structure;
- the thickness of the endometrium continues to grow and reaches 6–7 mm.
Late
On days 11–14 of the cycle (late stage), the cells inside the vagina increase in volume and swell. Significant changes occur in the uterine lining:
- the epithelial layer is high and multilayered;
- some of the glands elongate and have a wavy shape;
- the vascular network is tortuous;
- cell nuclei increase in size and have a rounded shape;
- the thickness of the endometrium in the late proliferative phase reaches 9–13 mm.
All of these stages are closely related to the secretion phase and must correspond to normal values.
Diagnostics
Diagnosis of thin endometrium is based on three principles:
- interviewing the patient;
- gynecological examination;
- additional examination.
During the interview, the doctor details all complaints, clarifies their nature, time and possible cause of occurrence, and dynamics. This will be followed by a gynecological examination, during which the doctor may identify some causes of thin endometrium, such as underdeveloped uterus or congenital anomalies.
Additional research methods are used:
- flora smears;
- laboratory methods to identify the causative agent of infectious diseases;
- tests to determine the level of hormones in the blood;
- ultrasound examination;
- CT;
- MRI;
- hysteroscopy;
- diagnostic laparoscopy.
Based on the results of additional research methods, the doctor will make a final diagnosis and prescribe treatment.
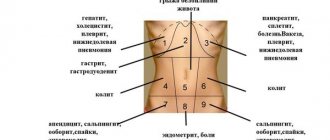
Disorders of the mucosal layer
So what do you need to know about this? The main reasons why the endometrium does not grow were discussed above. However, despite the fact that the most common case is a lack of estrogen, it is not the only reason. Very often the problem is caused by the following factors:
The most severe case is when the endometrium does not grow after curettage. When performing abortions or various operations, doctors have to act blindly, so the likelihood of soft tissue damage is very high. And if surgical procedures are performed repeatedly, then a high risk of developing infertility is created, since the basal layer simply has nothing to form from.
Physiotherapeutic treatments
If the doctor was able to determine why the endometrium is not growing and select the most optimal treatment program, but the expected result was not achieved, then drug therapy is combined with physiotherapeutic procedures to increase effectiveness. They significantly speed up the rehabilitation process after infectious diseases of the genitourinary system, and contribute to the normalization of hormonal levels. The following procedures have proven themselves to be excellent:
The doctor determines which procedure to prescribe based on the diagnosis and clinical picture of the patient. It is not recommended to sign up for them on your own, as they have many contraindications.
Insufficient thickness
It has already been said above whether the endometrium grows after ovulation. As soon as the menstrual cycle ends, the old layer is rejected and the formation of a new one begins. This is the basis of the theory that you need to have an idea about. But it happens that the mucosal layer does not develop. As a rule, this is caused by a violation of the normal blood circulation of the internal organs of the pelvic area, as a result of which they cease to receive enough nutrients necessary for normal functioning. The following pathologies may be to blame for this:
How quickly does the endometrium grow in any of the above cases? It is very difficult to answer this question, since each specific case is unique. Development can be either slow or completely absent. Regardless of the dynamics, the woman requires long-term complex therapy based on taking medications and physiotherapeutic procedures.
Artificial insemination
As noted above, if the mucosal layer is not thick enough, the fertilized egg will not be able to attach to the wall of the uterus. In most cases, timely treatment allows achieving positive results - the woman manages to become pregnant. However, in rare cases, therapy may lead to nothing, so some representatives of the fair sex go for artificial insemination. But with it everything is not so simple, since for some it turns out to be a lifeline, and for others - another disappointment.
In vitro fertilization very often ends unsuccessfully, since irreversible changes occur in the inner mucous membrane of the uterus, as a result of which the following can occur:
Considering all of the above, it is worth noting that you should agree to artificial insemination only as a last resort. You must first consult with a specialized specialist, as well as undergo a full examination and preparation. Only with a serious approach can you at least slightly increase the chances of successful conception and the birth of a healthy baby.
Alternative medicine
If you know until what day of the cycle the endometrium grows and can independently identify the problem at an early stage, then you can try to cope with it using traditional methods. Our ancestors created a huge number of different decoctions and infusions that allowed us to restore the normal growth of the mucosal layer. However, it is best to first consult with a specialist, since, firstly, self-medication can be dangerous, and secondly, the use of folk remedies will be much more effective if combined with modern methods of treatment.
Decoctions of plants such as:
Also, many healers advise drinking freshly squeezed pumpkin juice and tea brewed from young raspberry leaves. These plants are a good source of phytosterol, which in its composition and effect on the body is very similar to female sex hormones. In addition to decoctions, bdellotherapy, therapeutic massage and acupuncture help well with this problem. If your endometrium is not growing well, then these methods will not only activate soft tissue cells, but also generally improve and strengthen the body, as well as normalize the functioning of internal organs.