The endometrium is heterogeneous on ultrasound: reasons, changes in its thickness in different phases of the cycle are normal
The female genital area is an area under constant control of the body's hormonal system. Almost any hormonal imbalance affects the condition of the ovaries, uterus, as well as its epithelium, and a heterogeneous endometrium is often detected.
Read further about ultrasound methods for diagnosing pathologies of the uterine epithelium and the causes of their occurrence.
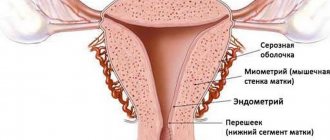
Anatomical features of the endometrium
The endometrium is the lining of the uterus. Its main functions are to create conditions for the attachment of a fertilized egg (blastocyst), as well as to prevent the adhesion of the walls of the uterus and the formation of intrauterine adhesions.
The structure of the endometrium is normally homogeneous and consists of several layers:
- Basal layer . Located directly on the muscular wall of the uterus. The thickness is approximately 1 cm. Its structures change little in different phases of the monthly cycle. A structural feature is a very well developed vascular network. The function of the basal endometrium is to restore the surface uterine epithelium after menstruation.
- Functional layer . Represented by columnar ciliated epithelium. The proliferation of its cells is hormone-dependent and varies depending on the phase of the cycle. During menstruation, the functional layer is completely rejected and then restored due to cell division in the basal lamina.
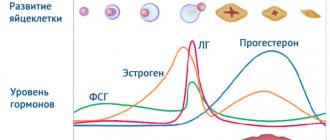
Changes in the endometrium during different phases of the menstrual cycle are normal
The average length of the monthly cycle varies from person to person and ranges from 23 to 31 days, with an average of 28 days. Depending on the state of the epithelial layer of the uterus, 3 main phases are distinguished:
- Desquamation . During this phase, menstruation occurs - the rejection of the functional layer of the epithelium. The destruction of the upper layer of the epithelium is initiated by a decrease in the production of progesterone by the corpus luteum of the ovary. This leads to spasm of the supply vessels, which causes ischemia and necrosis of epithelial cells. The subsequent relaxation of blood vessels promotes the detachment of superficial areas down to the basal epithelium and their removal during menstruation.
- Regeneration . Under the influence of estrogens secreted by the maturing ovarian follicle, active cell division and complete restoration of the surface area of the epithelium occur. The duration of the proliferative phase is approximately 14 days, before the onset of ovulation.
- Secretions . After ovulation, a corpus luteum is formed, which actively synthesizes progesterone. Under the influence of this hormone, the endometrium reaches its maximum thickness, and the number of glands producing mucous secretion increases. If fertilization does not occur, then the concentration of progesterone gradually decreases and menstruation begins.
Thus, the condition of the epithelial layer of the uterus is under the control of estrogen and progesterone produced by the ovaries. The work of the appendages, in turn, is regulated by follicle-stimulating (FSH) and luteinizing (LH) hormones of the hypothalamic-pituitary system.
Ultrasound of the endometrium: normal indicators
The structure and structural features of the uterus, including its epithelial layer, are determined during an ultrasound examination of the pelvic organs.
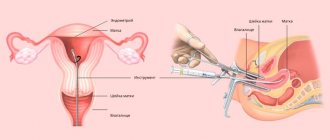
To determine the condition of the endometrium, it is preferable to perform intravaginal ultrasound using a special sensor.
This will allow the doctor to accurately determine the thickness, echogenicity and presence of pathological formations in the epithelial layer of the organ.
The optimal time for an ultrasound examination is days 5–7 of the cycle, that is, almost immediately after the cessation of menstruation. During this period, there is no functional epithelium, and the doctor can easily identify pathological formations in the uterine cavity.
During an ultrasound, the so-called M-echo, or median echo of the uterus, is determined. This parameter allows you to evaluate the following characteristics of the uterine endometrium:
- thickness of the epithelial layer;
- structure;
- correspondence of the structure of the epithelium to the phase of the menstrual cycle;
- the presence of pathological inclusions and inflammatory changes;
- readiness of the endometrium for attachment of the fertilized egg.
Normal endometrial indicators depending on the day of the cycle
The table below shows the thickness of the endometrium and its echogenicity depending on the phase of the cycle for women of reproductive age.
| Cycle day | Endometrial thickness, mm | Echostructure |
| 1–3 | 3–9 | Endometrium of heterogeneous structure |
| 4–6 | 3–4 | Not visible on echogram |
| 7–9 | 8–10 | There is a decrease in echogenicity |
| 11–15 | 10–13 | A clear hyperechoic rim appears |
| 16–19 | 13–16 | Likewise |
| 20–23 | 10–22 | The growth of the functional layer of the uterine epithelium stops. The echogenicity of the epithelium is increased. |
| 24–28 | 10–18 | Likewise |
What the thickness of the endometrium depends on and what its normal value is, the specialist explains in this video.
Endometrial parameters during menopause
The thickness of the endometrium during menopause decreases compared to the reproductive period. Accordingly, it does not change due to the absence of cyclic changes in the concentrations of female sex hormones.
When menopause lasts less than 5 years, the thickness of the epithelial layer is considered to be no more than 5 mm. Subsequently, the uterine epithelium continues to thin 10 years after menopause, reaching 3 mm. Exceeding normal M-echo levels during menopause is a reason for an in-depth examination, as this gives reason to suspect an oncological process in the uterus.
Homogeneous endometrium - what does it mean?
A completely homogeneous epithelial layer is characteristic of menopausal women. This is due to a decrease in the concentrations of female sex hormones in the female body.
During childbearing age, the uterine epithelium cannot be constantly homogeneous, since it is constantly subject to hormonally dependent changes.
It is important to understand that during the reproductive period it is not so much the homogeneity of the epithelium that is important, but its compliance with the phases of the menstrual cycle.
Heterogeneous structure of the endometrium - what is it?
To confirm the presence of heterogeneous endometrium, it is recommended to perform an ultrasound scan in the first phase of the cycle, since after rejection of the basal layer, all deviations from the norm are easily visualized.
With a heterogeneous structure of the uterine epithelium, the following is observed:
- hyperplasia – its growth over 16–17 mm;
- epithelial hypoplasia - a decrease in the thickness of the layer below 8 mm during childbearing age;
- pathological formations - cysts, polyps, tumors ;
- inflammatory processes - acute and chronic endometritis .
Causes of heterogeneity of the uterine epithelium
Source: https://uzi.guru/mal-taz/womns/metr/f/endm/endometrij-neodnorodnyj.html
Disruption of the development of the inner layer of the uterus
Diagnosis of the thickness of the layer lining the inner surface of the uterus is usually prescribed for infertility. It is determined by the presence of unprotected sexual intercourse throughout the year in the absence of pregnancy in the woman. Insufficiency of the layer (hypoplasia) prevents the implantation of a fertilized egg, and it is rejected by the body.
In addition to the inability to become pregnant, the patient’s risk of developing a bacterial infection of the main reproductive organ increases. After all, thinning the layer reduces the resistance of the uterus to aggressive environmental factors and pathogenic bacteria. After establishing the pathology and identifying its cause, the doctor prescribes drugs that affect the growth of the internal lining of the organ.
When planning pregnancy, it is important to monitor the correspondence of endometrial development to the days of the cycle. Deviation from the norms threatens the usefulness of the reproductive system. If a disorder in the direction of hyperplasia or a decrease in thickness is detected, hormonal therapy is prescribed, but this happens after the main factor that caused the failure has been eliminated.
Causes of endometrial heterogeneous structure
Heterogeneous endometrium is an alarming signal about the presence of various abnormalities in a woman’s body.
So what does this mean? The endometrium is the tissue that covers the inner layer of the uterus, and its heterogeneity confirms the presence of an inflammatory process or hormonal disorder.
For doctors, such heterogeneity of the uterus signals a deviation not only in the female genital organs, but also in the body as a whole.
Features of the endometrium
The endometrium is the lining of the uterus, which is enriched with blood vessels. The size of the inner layer of the uterus helps in determining the disease, which can even threaten a woman’s life. The thickness of the endometrium varies depending on various factors, but in some cases this may be the norm.
Normal indicators
For women of childbearing age, the normal endometrium at different phases of the cycle has its own characteristics:
- Phase 1 – Beginning of the cycle. The thickness of the endometrium varies from 5 to 9 mm. The sound comes through perfectly, and there are no separations into layers.
- Phase 2 – Middle of the cycle. The endometrium thickens. Echogenicity decreases, but sound transmission remains quite high.
- Phase 3 – End of the cycle. The endometrium is divided into layers with hyperechoic inclusions that reach 9-10 mm. It is also worth noting that this is the most favorable phase for conception.
And for women in the postmenopausal stage, the thickness of the inner lining of the uterus is considered to be at least 6 mm with an even structure.
In general, the endometrium normally has a somewhat homogeneous structure, that is, it is equally compacted and also approximately thickened depending on the phase of the cycle. However, it is worth noting that in rare cases, a heterogeneous inner layer of the uterus may be a physiological norm, but generally this indicates dangerous disorders in the body.
Reasons for deviations
Basically, when the endometrium has a heterogeneous structure, this is considered a physiological norm. It depends on what phase of the menstrual cycle the woman is in now.
And the following deviations indicate problems with uneven endometrial thickness:
- When the heterogeneous inner layer of the uterus, regardless of the period of the menstrual cycle, is manifested by a change in the hormonal background of the female body.
- When a woman is pre- or postmenopausal, this condition may indicate the presence of cancer or other serious pathological processes.
A significant factor in the heterogeneity of the endometrium is a violation of the blood supply to the internal mucous membrane of the uterus.
The main task before the gynecologist is to determine the exact cause of the deviation. To do this, the patient will have to undergo an extensive examination, and sometimes even consult with specialists of a different profile.
Using an ultrasound, a specialist sees the structure and size of the endometrium and gives an opinion whether pathological changes are present or not.
Types
At this time, it is customary to divide this condition into two types, namely:
- Normal heterogeneous endometrium is when development occurs during the menstrual cycle or during pregnancy. This condition is normal, that is, natural, it does not cause discomfort and does not require medication.
- Pathological is when development occurs outside of bearing a child and outside the corresponding day of menstruation. This pathology must be treated with medication, but first you need to determine the cause of its occurrence. There can be many factors: hormone imbalance, trauma to the uterine mucosa, impaired blood supply, as well as microcirculation of the internal layer and the pelvic organs as a whole.
It is worth noting that there are cases of congenital heterogeneity of the endometrium due to underdevelopment or developmental features of the reproductive system.
Symptoms
The symptomatic manifestations of this disease are not well defined, but both the doctor and the patient herself should be alert, firstly, to irregularities in the menstrual cycle and the presence of pain during menstruation. These signs show heterogeneous endometrium in the initial stages.
The heterogeneous structure of the endometrium is diagnosed by a gynecologist based on the results of an ultrasound examination, and after additional examination it is possible to determine a number of other diseases. With timely consultation with a doctor, a woman can prevent the development of infertility, cancer, heavy bleeding, accumulation of blood in the uterine cavity, and endometrial rupture.
If a heterogeneous endometrium has already been diagnosed, this means that an inflammatory process has started in the body. It cannot be ignored, and even more so, self-medication, this will only worsen the situation.
Perhaps the gynecologist will prescribe curettage - this is a fairly simple procedure. It involves removing the top layer of the uterus, which then tends to recover. As a rule, this procedure is carried out some time before the onset of menstruation.
Treatment after surgery is prescribed with antibiotics. Spotting or slight bleeding may occur for a short period of time.
A heterogeneous structure of the inner layer of the uterus occurs after a medical abortion. In this case, due to the thin layer of the endometrium, curettage is not prescribed.
The recovery process lasts for a month, but doctors are trying to speed up the process.
https://www.youtube.com/watch?v=fI0oEDQ1fEw
All women are recommended to follow preventive measures that help prevent the formation of gynecological diseases.
Treatment
Depending on the type of pathological process and the condition of the mucous membrane, certain drug therapy is prescribed. In cases of inflammation, treatment is carried out with antibiotics that have a wide spectrum of action, namely:
- Ceftriaxone;
- Amoxicillin.
Drugs are also prescribed to boost the immune system. In some cases, non-steroidal anti-inflammatory drugs are prescribed in addition:
In cases of hormonal imbalance, treatment is carried out using hormones:
- Quite often with the use of combined oral contraceptives, such as Regulon, Yarina;
- Estrogen, for example, Estrogel;
- Progesterone, for example, Utrozhestan, Nokolut.
Prevention
In order to prevent this disease, the following recommendations should be taken into account.
Firstly, you should start by undergoing an ultrasound and a preventive examination with a gynecologist at intervals of once every six months. You should also undergo the necessary tests and smears, especially for women of reproductive age, as you need to regularly monitor your hormone levels.
During sexual intercourse, you should pay attention to the use of barrier methods of contraception, which can prevent the onset of unwanted conception. This is also one of the methods of preventing infection with sexually transmitted diseases.
A mandatory requirement is to undergo a preventive examination and ultrasound once a year for women who are in a state of menopause, since these women are at risk.
If you experience the first alarming symptoms or pain in the pelvic organs, you should urgently contact your treating gynecologist.
This condition may indicate the presence of infection or the development of pathological abnormalities.
If you are attentive to your health and take care of it, you can prevent the occurrence of various kinds of diseases or quickly cure them at an early stage.
Source: https://MatkaMed.ru/endometrij/neodnorodnyj-endometrij
What does heterogeneous endometrium mean - Gynecology
A woman's reproductive health depends on many factors. Of great importance in the ability to conceive and bear a child is the endometrium, which has the property of changing during a woman’s menstrual cycle.
But there are situations in which, under the influence of various factors, pathological conditions arise in the endometrium, for example, its heterogeneity.
What this means and what treatment is used for this disease will be discussed in the article.
Definition of endometrium
The endometrium is the mucous membrane of the uterus that lines its inner surface. It is rich in multiple blood vessels. The thickness of the endometrium changes throughout the cycle under the influence of hormonal levels.
Normally, it has a relatively uniform structure, the same density and approximately the same thickness. Immediately after menstruation, the endometrium thickens in preparation for the attachment of a fertilized egg.
If this does not happen, the functional layer is rejected and leaves the body along with the blood, after which the basal layer is restored.
But sometimes there are situations in which, during ultrasound diagnostics, the doctor determines untimely heterogeneity of the endometrium. What does it mean? This condition indicates hormonal imbalances or serious inflammatory processes.
Norms
Let's look at the normal indicators of the endometrium depending on the phase of the menstrual cycle (see table).
| Cycle days | Endometrial thickness, mm | Echogenicity |
| 1–2 | 5–9, heterogeneous | Reduced |
| 3–4 | Around 5 | good |
| 5–7 | Until 6 | Slightly reduced |
| 8–10 | To 10 | Promoted |
| 11–18 | 8–15 | Average |
| 19–23 | 12–16 | Promoted |
| 24–26 | 9–12 | Promoted |
| Menopause | About 6 | Promoted |
Causes
Heterogeneity of the endometrium can be a consequence of both physiological processes occurring in the body and pathological ones, which require immediate treatment. Let's consider the most common factors in the development of endometrium of heterogeneous thickness.
Physiological reasons include:
- A certain phase of the menstrual cycle.
- Pregnancy. In this case, careful medical supervision is necessary, since this condition may indicate a pathological process that threatens the normal course of pregnancy.
- Menopause. A doctor's supervision is required.
There are many more pathological reasons for the heterogeneous thickness of the endometrium of the uterus. These include:
- Hormonal disorders. During menstruation, progesterone plays an important role, under the influence of which the endometrium increases. Then, to maintain the thickness of the uterine mucosa within normal limits, estrogen begins to act, which prevents excessive growth of the endometrium. If hormonal levels are disrupted, there is a high probability of developing dangerous diseases.
- Inflammatory processes in the appendages.
- Poor blood circulation in the uterus and other organs of the woman’s reproductive system.
- Underdevelopment of the reproductive organs.
- Adenomyosis, characterized by the appearance of cystic neoplasms of various sizes in the uterine cavity.
- Submucosal fibroid. At the same time, the tissue around itself grows, the uterus enlarges. Heterogeneity of the endometrium is detected locally.
- Polyps in which there is uneven growth of the mucous layer of the uterus.
- Poor quality curettage of the uterine cavity.
- Endometrial diseases (for example, endometriosis, hypoplasia or endometritis).
- Traumatic effects on the uterus.
- Abortion.
- Taking hormonal drugs.
- Benign neoplasms on the uterus.
- Malignant formations, which, however, develop significantly rarely.
Symptoms
The initial stage of the condition, in which heterogeneity of the endometrium develops, does not manifest itself with characteristic signs. The clinical picture can be quite blurred. As the underlying cause of the condition progresses, symptoms become more severe. Let's look at the most common signs:
- Menstrual irregularities, which may result in long delays, painful menstruation and heavy menstruation.
- Infertility.
- Separation of mucus from the genitals.
- Miscarriages.
In the future, the manifestations of the pathological condition will depend on the cause that caused it. If the above symptoms appear, it is recommended to consult a doctor and undergo the necessary tests.
Diagnostics
Heterogeneity of the endometrium cannot be determined during a routine medical examination.
The most informative diagnostic method in this case is ultrasound diagnostics, during which a specialist is able not only to assess the condition of the endometrium, but also to identify neoplasms and other factors that have led to changes in the mucous layer of the uterus. Using ultrasound, heterogeneous endometrium can be diagnosed as accurately as possible.
In addition to ultrasound examination, it is possible to prescribe curettage, which is both a diagnostic tool and a treatment method.
Laboratory tests are very important, which include:
- Analysis of urine.
- General blood analysis.
- A blood test for hormones, which is performed on certain days of the cycle.
- Swabs for infections.
Preventive measures
To prevent the development of endometrial heterogeneity, it is necessary to adhere to certain rules. Let's look at them in more detail:
- First of all, you need to carefully monitor your health and not neglect scheduled visits to the gynecologist, especially during pregnancy.
- If even minor signs appear, you should go to the hospital as soon as possible and undergo an ultrasound examination.
- Monitor the level of hormones in the body by periodically taking tests, especially for women in menopause and during pregnancy, as hormonal changes occur in the body.
- Maintain intimate hygiene.
- Use contraception.
- Follow all recommendations of your attending physician.
Possible complications
In the absence of adequate and timely treatment, pathological conditions that lead to heterogeneity of the endometrium can lead to the development of dangerous complications. These include:
- Infertility.
- Miscarriages.
- Degeneration of pathological areas into a malignant form.
- Bleeding.
- Endometrial ruptures.
If the structure of the endometrium of the uterus is heterogeneous, the possible consequences depend on the reason that led to the change in the mucosa.
Forecast and conclusion
With a systematic visit to the doctor, it is possible to detect changes in the endometrium at an early stage. This will allow you to promptly detect the cause that provoked the appearance of heterogeneity of the mucous membrane and begin treatment. In this case, the prognosis in most cases will be positive. Otherwise, serious complications may develop.
If the endometrium is heterogeneous, self-medication is prohibited. Therapy is prescribed only by the attending physician after establishing the cause of this condition and strictly on an individual basis.
Source:
If the endometrium is heterogeneous, what does this mean?
Heterogeneous endometrium is the first signal that there are any abnormalities. The endometrium is the tissue that lines the inside of a woman's uterus. It is well equipped with blood vessels and occupies a major place in the menstrual cycle.
During menstruation, the endometrium peels off and comes out along with the blood.
Heterogeneity of the tissue may indicate that there are inflammatory processes in the woman’s body or hormonal changes have occurred, and the cause of heterogeneity is long-term use of antibiotics.
There are two types of layers in this fabric:
- basal;
- functional.
During the onset of menstruation, the second layer (functional) is rejected, but the first layer (basal) is then restored in the next cycle.
You need to know that the endometrium has a strong sensitivity to hormones; accordingly, in the second period of the menstrual cycle, this tissue thickens.
This leads to preparation for the acceptance of the embryo; in cases where fertilization does not occur, the functional layer is rejected and then menstruation simply occurs.
In order for fertilization to occur, it is very important to know the thickness of the endometrium; it can only be determined by performing an ultrasound examination. The thickness varies depending on what phase of the cycle.
The structure and thickness of the endometrium in women who are likely to give birth is very different from that of those who are postmenopausal.
In postmenopausal women, as a rule, this tissue consists of one layer (basal). That is why the endometrium has a small thickness (less than 6 mm) and a homogeneous structure.
In women who are of reproductive age, rejection occurs approximately 3 to 5 days after the start of menstruation.
In postmenopausal women, the endometrium can be considered normal if its size is at least 6 mm and its structure is homogeneous. The thickness becomes smaller due to increasing age category. In certain cases, the echogenicity of the uterine cavity itself in women is characterized by a direct accumulation of mucus or secretion in the lumen itself.
Normal endometrium
In the first days of the menstrual cycle, the endometrium has the appearance of a heterogeneous structure, it transmits sound without obstacles, the total thickness is 5-9 mm. During this period there is no division into layers.
On the third day of the cycle, the endometrium begins to resemble a formation with good echogenicity, the size of which is approximately 3-5 mm.
On the fifth day, you can notice a large increase in the structure itself, it becomes dense, and the size becomes about 7-9 mm, the previously mentioned echogenicity begins to decrease, and sound conductivity, accordingly, increases.
On the eighth day, changes are observed: the endometrium becomes a hyperechoic structure, the size reaches 9-10 mm. Approximately this size is fixed until the end of the menstrual cycle. The endometrium, which is normal in accordance with the phase of the cycle, forms a good environment for the attachment of the fertilized egg.
There are a number of reasons why there may be a discrepancy with the day of the cycle:
- The resulting hormonal imbalance.
- Consequences of improper scraping, which led to injuries.
- The uterus is not developed enough.
- Poor blood circulation in the uterus and pelvic organs.
Source: https://cmsch71.ru/ginekologiya/chto-oznachaet-neodnorodnyj-endometrij.html
The structure of the endometrium is homogeneous
The female genital area is an area under constant control of the body's hormonal system. Almost any hormonal imbalance affects the condition of the ovaries, uterus, as well as its epithelium, and a heterogeneous endometrium is often detected.
Read further about ultrasound methods for diagnosing pathologies of the uterine epithelium and the causes of their occurrence.
Ultrasound of the endometrium: normal indicators
The structure and structural features of the uterus, including its epithelial layer, are determined during an ultrasound examination of the pelvic organs.
To determine the condition of the endometrium, it is preferable to perform intravaginal ultrasound using a special sensor.
This will allow the doctor to accurately determine the thickness, echogenicity and presence of pathological formations in the epithelial layer of the organ.
The optimal time for an ultrasound examination is days 5–7 of the cycle, that is, almost immediately after the cessation of menstruation. During this period, there is no functional epithelium, and the doctor can easily identify pathological formations in the uterine cavity.
During an ultrasound, the so-called M-echo, or median echo of the uterus, is determined. This parameter allows you to evaluate the following characteristics of the uterine endometrium:
- thickness of the epithelial layer;
- structure;
- correspondence of the structure of the epithelium to the phase of the menstrual cycle;
- the presence of pathological inclusions and inflammatory changes;
- readiness of the endometrium for attachment of the fertilized egg.
Values for menopause
The onset of menopause is marked by a decrease in the production of female sex hormones, therefore, at approximately the age of 45-55 years, a woman’s regularity of menstruation is disrupted until it completely disappears.
The endometrium no longer undergoes cyclical transformations and does not increase its thickness. It remains within 5 mm, which is considered normal, and if it is exceeded, the development of a pathological process is suspected, including the growth of neoplasms (polyps, cysts, tumors).
Heterogeneous structure of the endometrium: normal or pathological
Women's reproductive health depends on the condition of the endometrium. This term usually refers to the tissue covering the inner layer of the uterus.
Throughout the entire menstrual cycle, changes in the mucous membrane are observed, and in many cases this is considered a physiological norm.
But pathological structural disorders are also possible, when heterogeneous endometrium is a sign of abnormalities in the body. Most often this occurs under the influence of hormonal disorders and inflammatory processes.
Characteristic
In the female reproductive system, the endometrium plays a special role. For successful embryo implantation and normal development of the embryo, the inner layer of the reproductive organ must have sufficient maturity and an appropriate structure.
Thanks to uterine changes, the female body prepares for possible fertilization. The heterogeneous structure of the endometrium and the different thickness of the inner layer in certain phases of the cycle create comfortable conditions for conception.
The mucous membrane is very sensitive to hormonal levels. It is this feature that is reflected in the size of the endometrium. Immediately after menstruation, the tissue thickens, which facilitates the successful attachment of the egg to the villi of the inner layer of the uterus.
The embryo receives the amount of oxygen molecules and nutrients necessary for growth. If pregnancy does not occur, the functional layer of tissue is torn away and comes out with blood.
The woman begins her period, and the remaining basal layer is restored by the onset of the next menstrual cycle.
A physiologically normal process is characterized by a change in the thickness of the inner layer of the uterus only during certain phases of the cycle. If a failure occurs and the doctor diagnoses untimely structural disorders, diffuse changes in the mucosa are possible.
The pathological proliferation of epithelial cells and glands over the entire uterine surface leads to the ingrowth of the endometrium into the adjacent muscle layer (myometrium). Such conditions must be corrected at the initial stage, otherwise the woman may have problems conceiving.
Diffuse changes in the myometrium are one of the most common gynecological problems, but this is far from the only cause of disruption of the endometrial structure. Before we deal with abnormal conditions, we will outline situations when you don’t have to fear for your health.
Standard indicators
An atypical structure of the uterine mucosa may be congenital, but such cases are rarely detected. Normal heterogeneity of the endometrial structure is diagnosed:
- Endometrium during pregnancy. When carrying a child, progesterone dominates in a woman’s body, causing endometrial growth. The hormone level increases gradually and reaches a maximum at the time of birth.
- During menopause. With age and the approach of menopause, the structure of the endometrium changes. The functional layer gradually becomes thinner, and with the onset of menopause, only the basal layer remains. The tissue has a homogeneous structure and is normally 5–6 mm.
- Specific phases of the menstrual cycle. In a healthy woman, in the first days of menstruation, the thickness of the mucous membrane is 5–8 mm. Around the 3rd day, the endometrium transforms and acquires good echogenicity. During this period, the size of the surface tissue varies from 3 to 5 mm. By the end of menstruation, the inner layer of the uterus increases, thickens and reaches a thickness of 7–9 mm. On the 8th day, the size of the mucosa is 8–10 mm.
The development of the endometrium throughout the cycle allows us to identify the presence of severe disturbances in the functioning of the body. The thickness should vary from 5 to 17 mm. If changes are not detected by ultrasound, treatment is prescribed. Women whose condition of the uterine mucosa does not correspond to the norms of a particular phase also need therapy.
Transformations associated with loss of endometrial homogeneity during menopause and pregnancy do not cause discomfort and are not treated. These are normal conditions, but medical supervision and preventive measures should not be excluded. The situation can change at any moment, and it is only possible to identify blood supply disturbances and other abnormalities with regular ultrasound scans.
Pathological conditions
Violation of the structure and thickness of the uterine mucosa can be caused by diseases such as:
- submucous fibroid (benign neoplasm);
- adenomyosis (cellular growth in the muscle layer of the uterus);
- polyps and cystic formations;
- endometriosis and endometritis;
- hyperplasia (structural deformation and pathological growth of the glands of the functional layer);
- malignant tumors.
Inflamed, uneven endometrium negatively affects the well-being and health of women. Many of the identified pathologies interfere with normal conception and pregnancy. Cancers can be life-threatening and require immediate treatment.
Research and diagnostics
During a routine examination, the condition of the endometrium is difficult to determine. Pathological changes are detected by ultrasound examination, which is done after menstruation.
A detailed analysis allows us to determine the density, thickness and structure of the endometrium.
During the examination, the doctor examines the echogenicity of the structure of the uterine mucosa and can identify neoplasms and other problems that affect reproductive functions.
In addition to local ultrasound, the doctor may prescribe curettage. If thickening and structural heterogeneity are detected, this type of surgical intervention is used for treatment and diagnosis.
In addition, for a more complete and detailed analysis, specialists from various fields can be involved in the diagnostic examination. This is due to the fact that the cause of many gynecological diseases are disorders of other systems and organs.
Complications and consequences of non-compliance
The main consequence of the discrepancy between the thickness of the endometrium and the standard indicators is the inability to become pregnant and carry a baby to term. Complications that occur more often against the background of hyperplasia include:
- submucous uterine fibroids;
- polyps;
- adenomyosis;
- endometriosis;
- malignant neoplasms;
- Irregular cycle and heavy periods.
Adenomyosis