What are the phases of menstruation, why should a woman keep monthly records? Is it possible to plan a pregnancy on your own if you clearly understand the essence of each phase of the menstrual cycle? Read more about the features of the female body in the article.
Female cycle norms
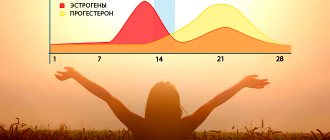
The female body has a certain exhaustible supply of eggs. Normally, in the first phase of the menstrual cycle, follicles begin to grow; by the middle of the menstrual cycle, one of them becomes leading or dominant (an egg is released from it during ovulation). At the site of the burst follicle, a corpus luteum is formed, which produces the hormone progesterone, which is necessary to maintain pregnancy if it occurs, and if this does not happen, menstruation begins.
The period from ovulation to menstruation is the second phase, and normally its duration is 14 days. The first phase can vary in duration.
To know how to count the menstrual cycle, use a simple rule - count the days from the beginning of one menstruation to the first day inclusive of the next. This period ranges from 21 to 33 days (plus or minus 3 days), but most often 28 days.
The average duration of menstruation ranges from 3 to 8 days (average value 5 days).
Normal blood loss during menstruation ranges from 40 to 80 ml.
Anything that goes beyond these parameters is a menstrual disorder .
It is necessary to understand that painful and heavy menstruation is a reason to consult a doctor. Since pain of varying intensity and weakness due to excessive blood loss with a subsequent drop in hemoglobin and iron levels ( posthemorrhagic anemia ) can significantly reduce a woman’s quality of life.
1 Colposcopy
2 Treatment of menstrual disorders
3 Treatment of menstrual disorders
Attention! Don't put off going to the doctor! Menstrual irregularities indicate the presence of pathological processes in the female body and can lead to infertility.
What do certain hormones affect?
An increase or decrease in the amount of female hormones in a certain phase is a sign of the presence of a disease that negatively affects the functioning of the reproductive system.
With the rapid growth of follicle-stimulating hormone, deviations such as:
- malignant tumors in the pituitary gland;
- deterioration in the functioning of the appendages;
- quick reaction of the body to obesity and bad habits.
A decrease in the level of luteinizing hormone is considered a sign of problems with the pituitary gland and can be caused by the presence of extra pounds. And the doctor notes an increase in the amount of this substance when a malignant tumor is detected in the brain.
Prolactin affects the amount of progesterone. Helps suppress follicle-stimulating hormone during pregnancy. Ensures the availability of milk during lactation. With this hormonal imbalance, the following is noted:
- problems with follicle synthesis that affect ovulation and ovarian function;
- dysfunction of the pituitary gland and its appendages.
Estrogen affects the formation of the egg and its release after the follicle ruptures. An increased amount indicates the presence of a neoplasm in the ovarian or adrenal glands. The level may be increased if the woman is underweight.
Problems with estrogen synthesis provoke a number of disorders:
- the possibility of getting pregnant decreases;
- disruption of the cycle;
- development of infertility.
Testosterone is a male sex hormone, a small amount of which is also present in the body of women. It maintains muscle mass, regulates the sebaceous glands and affects the nervous system. The hormone also promotes the growth of mammary glands during pregnancy and increases sexuality.
Causes of excess level:
- polycystic disease;
- benign and malignant formations;
- heredity;
- problems with the functioning of the adrenal glands;
- disturbances in the functioning of the pituitary gland.
Androgens are a type of hormone that plays a fairly important role in the female reproductive system. With the help of fat cells and skin, these hormones are transformed into estrogen.
Androgens prevent bone loss and are responsible for sexual desire and satisfaction.
If a female representative has a disturbed menstrual cycle, then it should be understood that any deviations have a negative impact on the functioning of the reproductive system.
A trip to the gynecologist and taking tests to determine the level of hormones in the body should become mandatory events. You should also monitor the phases of the menstrual cycle by day, then it will be easier to identify irregularities; which day of the cycle and which phase can be found out using special electronic calendars, which describe the women’s cycle by day.
Features of the menstrual cycle
The menstrual cycle is a monthly period in a woman’s life, which begins from the first days of the appearance of menstruation and until the first day of the next (with the exception of pregnancy and breastfeeding).
For natives of central Russia, the cycle begins at 11-14 years. In the first year, cyclical changes just begin to establish themselves, and then they occur at least 8 times a year.
Already at the time of birth, the baby’s ovaries contain approximately 2 million follicles, of which by the time the first menstruation occurs, just over 400 thousand remain. During each cyclic change, 1 ripening follicle is used to release an egg. Thanks to the precise functioning of the endocrine glands, the female cycle normally consists of two phases.
Cycle phases
The first phase is follicular. It is characterized by the action of follicle-stimulating hormone (or FSH), which is produced by the pituitary gland and hypothalamus. Thanks to FSH, the follicle grows and matures in the ovaries. During ovulation (the middle of the menstrual cycle), an egg emerges from a mature follicle, ready for fertilization.
The second phase is luteal . At this time, thanks to the work of brain hormones (luteinizing hormone or LH), the maturation of the corpus luteum begins, i.e. follicle that released the egg. If pregnancy occurs during this ovulation, the corpus luteum of pregnancy is created from the follicle.
Phases of cyclic changes in the endometrium
The follicular phase begins on day 5 of the cycle and lasts for 12-14 days. The active hormone is estrogen. During this period, the surface layer of the endometrium with tubular glands begins to grow.
The luteal phase lasts about 14 days. At this time, the levels of estrogen and progesterone increase. During this period, the tubular glands produce a secretion, the highest level of which is achieved on the 21st day of the cycle. On the 22nd day of the cycle, blood flow to the endometrial arteries increases, and excellent conditions for implantation of the zygote appear.
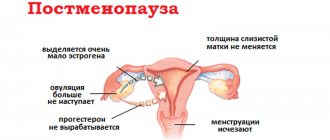
Menstruation occurs on days 24-27 of the cycle, only in cases where there has been no fertilization. It happens due to a small amount of hormones produced by the ovaries and a decrease in the blood supply to the endometrium. During this period, blood clots form in the endometrial vessels, then a sharp expansion and rejection of the endometrium occurs.
Thus, a constant cyclical process produced by the ovaries, endometrium and glands leads to the maturation and release of the egg from the ovary, its fertilization and attachment to the prepared endometrium, as well as the further development and maintenance of pregnancy. If fertilization does not occur, the functional layer of the endometrium is shed in the form of menstruation.
On what days of the cycle does the ovulatory phase occur?
The ovulatory phase of the cycle (menstrual) can be determined already 2 weeks (on the 14th or 15th day) after the onset of the follicular phase. During this time, various changes may occur in the patient’s body. On average, the duration of the ovulatory phase in patients with a 28-day menstrual cycle ranges from 36 to 48 hours. This period is the most favorable for conceiving a child, since the mature egg leaves the follicle (dominant) and penetrates the abdominal cavity. Its viability is quite short, only 24 hours, so if there is no fertilization during this time, pregnancy will never occur.
During the ovulatory period, patients experience increased sexual desire and overall well-being. They involuntarily begin to monitor their appearance, femininity and passion awaken in them.
Causes of menstrual irregularities
All causes of menstrual irregularities can be divided into 2 large groups - organic and functional.
Most often, organic causes are polyps or endometrial hyperplasia, adenomyosis or endometriosis of the uterus, uterine fibroids in the case of a submucosal location and malignancy.
Functional causes include ovarian dysfunction as a result of changes in climate and place of residence, overwork, stress, eating disorders, taking medications (anticoagulants, hormones, drugs from the field of psychiatry), and blood clotting disorders.
1 Uterine fibroids
2 Endometriosis
3 Ultrasound of the pelvic organs
general description
A blood test for hormones, the norm of which indicates a stable state in the body, is a full-fledged study of the concentration and presence in the composition of certain substances that are produced by the glands of the body.
Depending on the glands that secrete active substances into the blood, the test results indicate exactly those hormones that are necessary to diagnose a particular disease. For this reason, the norm of hormones in the human body is different for each indicator.
Types of menstrual irregularities
All types of menstrual irregularities depend on an increase or decrease in the volume of blood secreted, changes in the regularity of the cycle and the feeling of pain during menstruation.
Therefore, the following types of violations can be distinguished:
- hypomenstrual syndrome - a decrease in menstruation due to external reasons;
- oligomenorrhea - short time (2 days) of menstruation;
- amenorrhea - a period when there is no monthly cycle for six months;
- opsomenorea is a disorder in which the interval between cycles is more than 5-8 weeks;
- hypomenorrhea - low blood volume during menstruation;
- spaniomenorrhea - menstruation occurs only 2-4 times a year.
The next deviation is menorrhagia , which is manifested by copious discharge. There are different forms of it:
- hypermenorrhea - a large amount of blood loss within one menstruation;
- proyomenorrhea - “menstruation” occurs frequently, approximately every 2 weeks;
- polymenorrhea - prolonged and heavy discharge during menstruation.
Other types of deviations include:
- metrorrhagia - bleeding that occurs outside the cycle and without endometrial rejection;
- algodismenorrhea - menstruation accompanied by pain;
- intermenstrual bleeding - blood loss outside the cycle;
- bleeding during menopause - loss of blood in older women a year or more after menopause.
1 MRI of the brain
2 Laboratory diagnostics
3 Ultrasound of the pelvic organs
Hormone tests: normal indicators, interpretation
- A test for sex hormones is a test for the levels of substances such as testosterone, estradiol and progesterone in the blood. Testosterone is responsible for the growth of muscles, bones and the development of reproductive organs. Its blood level should be in the region of 4.95-32.02 nm/l in men and 0.39-1.98 nm/l in women. The normal value of the main estrogens depends on the phase of the female cycle. So, in the first phase, estradiol should be in the amount of 199-285 pM/l, and progesterone 1.1-2.3 nM/l.
- Tests for thyroid hormones depend on the selected active substance, the norm for each of which is different: thyroxine (0.6-1.49 ng/dl), T3 - (2.5 - 5.8 pm/l), AT-TG – (0-4.12 U/ml).
- During pregnancy, tests are prescribed for the hCG hormone, which is produced by the membrane of the embryo already on days 6-10 after fertilization, which makes it possible to quickly identify pathological development of the fetus, if any. The level of this hormone increases until the 7th month of pregnancy, and then sharply declines; for this reason, hormonal blood tests are performed very often.
- A blood test for adrenal hormones relies on three hormones: cortisol, DHEA-c and aldosterone. For the first, the norm is 3-22 mcg/dL for children and 3.8-19.5 mcg/dL for adults, for the second – 3592 – 11908 nm/l, for the third – 36 – 351 pg/ml.
An AMH test is included in the list of mandatory tests at the stage of diagnosing a woman and preparing for in vitro fertilization.
Interesting fact: AMH itself does not affect a woman’s fertility or ability to bear a child. However, it is the AMH level that allows you to assess the chances of natural conception or the likelihood of success with IVF. AMH analysis - the price is acceptable even in private clinics.
Diagnosis of menstrual cycle disorders
Before starting treatment for the menstrual cycle, it is necessary to undergo an examination.
During the consultation, the doctor can make a preliminary diagnosis based on a gynecological examination and the patient’s complaints, but will need to undergo a number of studies, including:
- laboratory blood test (hemoglobin level, serum iron, transferrin, sugar; hormone analysis);
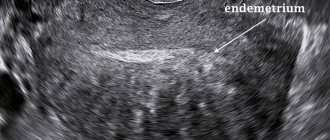
- Ultrasound examination of the pelvic organs (helps to exclude pathologies of the uterus, ovaries and endometrium);
- MRI of the brain for additional indications (performed to exclude tumors);
- examination of the inner layer of the uterus using hysteroscopy (carried out for dysfunctional uterine bleeding, if an endometrial polyp or hyperplasia, submucous uterine fibroid is suspected);
- colposcopy according to indications.
Videos on the topic
Reading time: min.
One of the most popular studies at the moment to detect the absence or presence of a certain disease is a blood test for hormones.
| Service name | Price |
| Initial consultation with a gynecologist | 2,300 rub. |
| Ultrasound gynecological expert | RUB 3,080 |
| Taking a smear (scraping) for cytological examination | 500 rub. |
| Complex “Reproductive Potential” Hormonal assessment of ovarian follicular reserve (AMH.FSH,LH,estradiol) | 1,900 rub. |
| Determination of testicular reserve, FSH stimulation test with cost of the drug | 5,000 rub. |
| FSH | 650 rub. |
| FSH (CITO) | 950 rub. |
| FSH (express) | 650 rub. |
Doctors use it especially often, since sometimes it is the fastest way to make an accurate diagnosis even in the early stages, which is especially important for effective treatment.
Treatment of menstrual disorders
Sometimes, in order to identify and treat menstrual irregularities, it is necessary to eliminate an external factor. It happens that this disorder is associated with a woman’s attempt to suddenly lose excess weight. In such cases, together with an endocrinologist, the correct diet and methods of weight correction are selected.
For mild to moderate bleeding, symptomatic treatment may be prescribed - the use of hemostatic drugs, replacement of iron loss, or antianemic therapy.
In extreme cases, treatment of menstrual irregularities may require surgical intervention, such as hysteroresectoscopy or endometrial ablation, uterine curettage, or hysterectomy.
Most often, menstrual irregularities are only a symptom of endocrine pathology or chronic inflammation. Only a highly qualified specialist can identify the causes of menstrual irregularities and prescribe appropriate treatment.
Our clinic has all the conditions for the treatment of menstrual disorders. If necessary, you can consult related specialists, such as an endocrinologist, neurologist, cardiologist, gastroenterologist, etc.
Adequate levels of estradiol and estrogen
Estrogen and its derivatives are the main female hormones; a woman’s general well-being, ability to conceive, and appearance depend on whether their level is normal. With a lack of estrogen, the following pathologies are detected:
- Menstrual irregularities.
- Psycho-emotional instability.
- Functional suppression of libido.
- Dermatological problems, drying and flaking of the skin.
However, excess estrogen production is no less dangerous and has a negative effect on the female body. This is fraught, for example, with the appearance of excess weight, dysfunction of the reproductive organs, and the development of cystic and other benign tumors. An elevated level tells the doctor about problems with the ovaries, causing instability of the menstrual cycle.
Standard values of progesterone
When undergoing a routine gynecological examination, patients are often prescribed a blood test for progesterone hormones. The level of this hormone in women is a diagnostically important criterion when planning conception, and is also important for the full bearing of a child. If progesterone levels remain unchanged throughout the entire menstrual cycle, the doctor will assume there is no ovulation. Low progesterone levels in pregnant women are a reason to take medications that facilitate and protect the pregnancy process.
Hormones:
norms of sex hormones in women , table of progesterone values
| Patients | Phases of the menstrual cycle | Progesterone level nmol/l |
| Girls from 0 to 9 years old | Less than 1.1 | |
| From 9 to 18 years old, in puberty. Tanner staging: | ||
| Stage I | Less than 1.1 | |
| Stage II | Less than 1.8 | |
| Stage III | 0,3-14,4 | |
| IV stage | 0,3-41,6 | |
| Stage V | 0,3-30,4 | |
| Women from 18 to 90 years old | ||
| After puberty and before postmenopause | ||
| In the follicular phase | 0,3-2,2 | |
| In the ovulatory phase | 0,5-9,4 | |
| Luteal phase | 7,0-56,6 | |
| Postmenopause | Less than 0.6 | |
| Pregnancy | ||
| I trimester | 8,9-468,4 | |
| II trimester | 71,5-303,1 | |
| III trimester | 88,7-771,5 |
Typical female hormones, norm table: luteinizing hormone (LH) and follicle-stimulating hormone (FSH)
FSH is responsible for follicular growth and maturation of eggs, and LH is necessary to stimulate ovulatory processes. I compare the level of these hormones with the normal table and, based on the identified deviations, make an assumption about the woman’s ability to conceive. High quantitative indicators of FSH and LH indicate acquired infertility.
Hormones: norm - table of indicators of LH, FSH, etc.
| Hormone | Normal indicator |
| Adrenocorticotropic (ACTH) | 0-50 ng/ml |
| Somatotropic (STG) | 0-10 ng/ml |
| Prolactin | 130-540 mcg/l in women of childbearing age. 107 |
| 107-290 mcg/l in women during menopause | |
| Thyroid stimulating (TSH) | 0.6-3.8 µIU/ml by RIA method |
| 0.24-2.9 µIU/ml using the IF method | |
| Follitropin (FSH) | 2.7-6.7 mIU/ml during ovulation |
| 2.1-4.1 mIU/ml in the luteal phase | |
| 29.6-54.9 mIU/ml in the menopausal phase | |
| Luteinizing (LH) | 18.2-52.9 mIU/ml during ovulation |
| 3.3-4.66 mIU/ml in the follicular phase | |
| 1.54-2.57 mIU/ml in the luteal phase | |
| 29.7-43.9 mIU/ml in the menopausal phase |
You need to understand that any deviation from the norms given in the tables can only be corrected under the supervision of a specialist, and therefore self-medication is strictly unacceptable.
Late secretion phase endometrium is cancer
On average, deciphering the results of an endometrial biopsy takes 1-2 weeks. This depends on the operating mode of the pathology laboratory and the complexity of the stains used.
The method of taking a biopsy of the uterine mucosa also plays a significant role - in some cases, the morphologist receives whole fragments of tissue with a preserved histological structure, while in others there is a high probability of receiving only blood clots.
Biopsy techniques
Most often, an endometrial biopsy is taken by traditional diagnostic curettage (CDC).
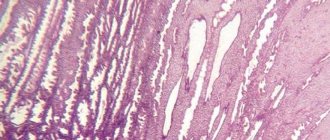
The resulting material consists of separate sections of the mucous membrane, in which the uterine glands, connective tissue stroma and their relationships with each other are clearly visible.
If the sample contains malignant elements, the pathologist can accurately determine the depth of their germination, and this directly affects the treatment tactics and prognosis of the disease.
Unlike RDV, during endometrial aspiration and pipel biopsy, the doctor does not receive complete layers of the mucosa, but its scattered elements with a large admixture of blood. Often the biomaterial is represented by nothing more than a meager accumulation of individual cells, from which it is impossible to reliably judge the nature of the pathological process.
From the point of view of the diagnostic value of the results of endometrial biopsy, preference should be given to separate diagnostic curettage.
However, in some cases, a comprehensive interpretation of biopsy specimens is not required. Thus, a pipel biopsy is usually performed to assess the condition of the endometrium before the IVF procedure.
In this situation, even scattered elements of the mucosa are enough to determine the type of pathology.
Interpretation of endometrial biopsy results
In his conclusion, the pathologist can give a different interpretation of the endometrial biopsy, with or without a detailed description of the morphology. Often the results are accompanied by a pathological diagnosis, which is a brief summary of the descriptive characteristics.
Below is an explanation of the various terms that can be found in the results of an endometrial biopsy.
Following actions
Further tactics depend on the method used to take the biopsy. If the results of an aspiration or pipel biopsy reveal hyperplasia and signs of atypia, then this in most cases serves as an indication for separate diagnostic curettage.
If, in addition to indicating the phase of the cycle and the presence of blood or detritus, nothing else is indicated in the conclusion, then in fact this indicates the absence of any pathology on the part of the endometrium.
Subsequent actions by the patient and the gynecologist should be aimed at excluding other causes of dysfunctional uterine bleeding.
The presence of tumor changes, including atypical hyperplasia, requires regular follow-up and consultation with a gynecological oncologist. The stage of the cancer process is determined and complex treatment is prescribed, including surgery, chemotherapy and radiation therapy.
Treatment in Israel
Israeli gynecologists have significant experience in treating various diseases of the uterus. Using modern technologies, doctors at the Top Ichilov Clinic accurately determine the likelihood of malignant degeneration of tumors and carry out their excision using minimally invasive methods.
To find out more detailed information regarding your case, fill out the form below.
For non-surgical treatment, Top Ichilov uses the latest drugs, the effectiveness of which exceeds 90%, and advanced techniques: brachytherapy, photodynamic therapy, radiotherapy using the latest generation TrueBeam units and many others.
If there is no choice left and it is necessary to surgically remove a tumor or even the uterus, Top Ichilov often uses the Da Vinci robotic surgical unit. This operation completely eliminates the possibility of medical error and prevents complications.
The endometrium is the mucous layer that lines the inside of the uterus. Its functions include ensuring implantation and development of the embryo. In addition, the menstrual cycle depends on the changes occurring in it.
One of the important processes occurring in a woman’s body is endometrial proliferation. Disturbances in this mechanism cause the development of pathology in the reproductive system. The proliferative endometrium marks the first phase of the cycle, that is, the stage that occurs after the end of menstruation. During this stage, endometrial cells begin to actively divide and grow.
Proliferation concept
Proliferation is the active process of cell division in a tissue or organ. As a result of menstruation, the mucous membranes of the uterus become very thin due to the fact that the cells that make up the functional layer are rejected. This is what determines the process of proliferation, since cell division renews the thinned functional layer.
However, proliferative endometrium does not always indicate the normal functioning of the woman’s reproductive system. Sometimes it can occur in the event of pathology development, when cells divide too actively, thickening the mucous layer of the uterus.
Causes
As mentioned above, the natural cause of proliferative endometrium is the end of the menstrual cycle. The rejected cells of the uterine mucosa are excreted from the body along with the blood, thereby thinning the mucous layer. Before the next cycle occurs, the endometrium needs to restore this functional area of the mucosa through the process of division.
Pathological proliferation occurs as a result of excessive stimulation of cells by estrogen. Consequently, when the mucous layer is restored, endometrial division does not stop and the walls of the uterus thicken, which can lead to the development of bleeding.
Process phases
There are three phases of proliferation (with its normal course):
- Early phase. It occurs during the first week of the menstrual cycle and at this time epithelial cells, as well as stromal cells, can be found on the mucous layer.
- Middle phase. This stage begins on the 8th day of the cycle and ends on the 10th. During this period, the glands enlarge, the stroma swells and loosens, and the cells of the epithelial tissue stretch.
- Late phase. The proliferation process stops on the 14th day from the beginning of the cycle. At this stage, the mucous membrane and all glands are completely restored.
Diseases
It is a consequence of hormonal disruption in the monthly cycle. Hyperplasia is a proliferation of endometrial and stromal glands and can be of two types: glandular and atypical.
Types of hyperplasia
The development of such an anomaly occurs mainly in women at menopausal age. The main reason is most often a large amount of estrogens, which affect endometrial cells, activating their excessive division.
With the development of this disease, some fragments of the proliferative endometrium acquire a very dense structure. In particularly affected areas, the compaction can reach 1.5 cm in thickness.
In addition, the formation of proliferative type polyps on the endometrium located in the organ cavity is possible.
This type of hyperplasia is considered a precancerous condition and is most often found in women during menopause or in old age. In young girls, this pathology is diagnosed very rarely.
Atypical hyperplasia is considered to be a pronounced proliferation of the endometrium, which has adenomatous sources located in the branching of the glands. Examining scrapings from the uterus, one can detect a large number of tubular epithelial cells.
These cells can have both large and small nuclei, and in some they can be stretched. In this case, the tubular epithelium can be either in groups or separately.
The analysis also shows the presence of lipids on the walls of the uterus; their presence is an important factor in making a diagnosis.
The transition from atypical glandular hyperplasia to cancer occurs in 3 out of 100 women.
This type of hyperplasia is similar to endometrial proliferation during a normal monthly cycle, however, during the development of the disease, there are no decidual tissue cells on the uterine mucosa.
Sometimes the process of atypical hyperplasia can be reversed, however, this is only possible under the influence of hormones.
Symptoms
With the development of proliferative endometrial hyperplasia, the following symptoms are observed:
- The menstrual functions of the uterus are disrupted, manifested by bleeding.
- There is a deviation in the menstrual cycle, in the form of intense cyclic and prolonged bleeding.
- Metrorrhagia develops - unsystematic and non-cyclical bleeding of varying intensity and duration.
- Bleeding occurs between periods or after their delays.
- Breakthrough bleeding with the release of clots is observed.
- The constant occurrence of bleeding provokes the development of anemia, malaise, weakness and frequent dizziness.
- An anovulatory cycle occurs, which can cause infertility.
Source: https://ginekologiya-urologiya.ru/potenciya/endometrij-pozdnej-stadii-fazy-sekretsii-eto-rak