The structure and purpose of the endometrium
The endometrium is basal and functional in structure. The first layer remains practically unchanged, and the second regenerates the functional layer during menstruation. If there are no pathological processes in a woman’s body, then its thickness is 1-1.5 centimeters. The functional layer of the endometrium changes regularly. Such processes are associated with the fact that during menstruation in the uterine cavity, individual sections of the walls peel off.
Damage appears during labor, during mechanical abortion or diagnostic sampling of material for histology.
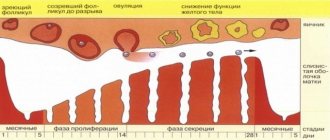
Women's menstrual cycle
Changes occur in the female body every month that help create optimal conditions for conceiving and bearing a child. The period between them is called the menstrual cycle. On average, its duration is 20-30 days. The beginning of the cycle is the first day of menstruation. At the same time, the endometrium is renewed and cleansed.
If women experience abnormalities during the menstrual cycle, this indicates serious disorders in the body. The cycle is divided into several phases:
Proliferation refers to the processes of reproduction and cell division that contribute to the growth of internal tissues of the body. During the proliferation of the endometrium, normal cells begin to divide in the mucous membrane of the uterine cavity. Such changes may occur during menstruation or have a pathological origin.
The duration of proliferation is on average up to two weeks. In a woman’s body, estrogen begins to increase rapidly, which is produced by an already mature follicle. This phase can be divided into early, middle and late stages. At an early stage (5-7 days) in the uterine cavity, the surface of the endometrium is covered with epithelial cells, which have a cylindrical shape. In this case, the blood arteries remain unchanged.
The middle stage (8-10 days) is characterized by the covering of the plane of the mucous membrane with epithelial cells, which have a prismatic appearance. The glands are distinguished by a slightly convoluted shape, and the nucleus has a less intense shade and increases in size. A huge number of cells appear in the uterine cavity, which arose as a result of division. The stroma becomes swollen and quite loose.
The late stage (11-15 days) is characterized by a single-layer epithelium, which has many rows. The gland becomes tortuous, and the nuclei are located at different levels. Some cells contain small vacuoles that contain glycogen. The vessels have a tortuous shape, the cell nuclei gradually acquire a rounded shape and greatly increase in size. The stroma becomes engorged.
The endometrium of the secretory type uterus can be divided into several stages:
- early (15-18 days of the menstrual cycle);
- medium (20-23 days, pronounced secretion is observed in the body);
- late (24-27 days, secretion gradually fades away in the uterine cavity).
The menstrual phase can be divided into several periods:
- Desquamation. This phase occurs from day 28 to day 2 of the menstrual cycle and occurs when fertilization has not occurred in the uterine cavity.
- Regeneration. This phase lasts from the third to fourth day. It begins before the complete separation of the functional layer of the endometrium along with the beginning of the growth of epithelial cells.
Definition
The diagnosis of reverse development of the endometrium is made, most often, based on the results of endometrial scraping. What it is? Reverse development of the endometrium is a condition of the uterine mucosa in which its condition does not correspond to the current phase of the cycle. This condition develops under the influence of hormonal imbalance. And the imbalance itself is already developing for various reasons, and depending on this, such a condition may or may not be pathological.
It is considered normal for a woman after childbirth. By the beginning of the first menstruation after the birth of a child, the endometrium may be in this state, and no treatment is necessary at this stage. The same applies to women during menopause and before the last menopause. In this case, reverse development can be observed and is not cured, as it is considered normal. The formation of the process is associated with the gradual fading of the functioning of the ovary due to natural reasons.
This condition usually does not manifest itself in any way in the patient, except for menstrual irregularities in some cases. There is usually no pain, deterioration of well-being and acyclic bleeding. Often this condition is diagnosed by chance, as it does not have a specific clinical picture.
Depending on what causes the pathology, it can occur as two completely different processes (which, in fact, are the two types of reverse development of the endometrium). Depending on what kind of impact or failure caused the pathology, fundamentally different treatments are prescribed. It is quite effective in both cases, and if eliminated in a timely manner, it does not in any way interfere with the occurrence of future pregnancies.
Pathology of the corpus luteum
A fairly common type of pathology. With reverse development in pathology of the corpus luteum, it occurs as a result of hormonal imbalance. This phenomenon is said to occur when persistence of the corpus luteum is observed. In this case, progesterone, which is produced by the corpus luteum, is formed in smaller quantities than it should. The pathological condition develops with sufficiently long-term exposure to such low concentrations.
How can a patient notice such a condition? A certain clinical picture is formed. The time of menstrual bleeding is prolonged, which is due to the fact that the secretory (renewing) endometrium is rejected and renewed more slowly. At the same time, most of it is subject to reverse development.
The reasons for this phenomenon almost always lie in the gradual decline of the function of one or both ovaries. Therefore, this condition is most typical for women of premenopausal age, as well as in menopause. However, sometimes it develops in women of reproductive age, which may be associated with endocrine diseases, cancer and inflammatory processes in the ovaries, as well as for other reasons.
Disturbed pregnancy
This condition has other causes and manifestations if it develops during a disturbed pregnancy. Moreover, this does not happen immediately; often a disrupted pregnancy is present in an undiagnosed patient for quite a long time (several weeks) before it begins to cause reverse development of the endometrium. Often it is diagnosed just when visiting a doctor due to symptoms of reverse development. In what cases can we talk about such a pregnancy?
- Incomplete spontaneous abortion;
- Incomplete removal of the fertilized egg during mechanical or medical abortion;
- Death of the embryo in a very early stage of pregnancy.
Normal structure
If the study is carried out at different phases of the menstrual cycle, the test result will be different. For example, towards the end of the proliferation period, the basal layer begins to increase, and therefore does not respond to any hormonal influences. At the very beginning of the cycle, the internal mucous cavity of the uterus has a pinkish tint, a smooth surface and small areas of the functional layer that has not completely separated.
At the next stage, a proliferative type of endometrium begins to grow in a woman’s body, which is associated with cell division. Blood vessels are located in folds and arise as a result of uneven thickening of the endometrial layer. If there are no pathological changes in the woman’s body, then the functional layer should be completely rejected.
Forms of deviation
Any deviations in endometrial thickness arise as a result of functional causes or pathological changes. Functional disorders appear in the early stages of pregnancy or a week after fertilization of the egg. In the uterine cavity, the baby's place gradually thickens.
Pathological processes arise as a result of chaotic division of healthy cells, which form excess soft tissue. In this case, neoplasms and malignant tumors form in the body of the uterus. These changes most often occur as a result of hormonal imbalance due to endometrial hyperplasia. Hyperplasia comes in several forms.
- Glandular. In this case, there is no clear separation between the basal and functional layers. The number of glands increases.
- Glandular-cystic form. A certain part of the glands forms a cyst.
- Focal. In the uterine cavity, epithelial tissue begins to grow and numerous polyps form.
- Atypical. In a woman’s body, the structure of the endometrium changes and the number of connective cells decreases.
Phases of endometrial proliferation: normal and abnormalities, diagnosis and treatment of concomitant diseases
The endometrium of the proliferative type is an intensive growth of the mucous uterine layer, occurring against the background of hyperplastic processes caused by excessive division of the cellular structures of the endometrium.
With this pathology, gynecological diseases develop and reproductive function is disrupted. When faced with the concept of proliferative endometrium, it is necessary to understand what this means.
Features of development
Endometrium - what is it? This term refers to the mucous layer lining the inner uterine surface. This layer has a complex structural structure, which includes the following fragments:
- glandular epithelial layer;
- main substance;
- stroma;
- blood vessels.
The endometrium performs important functions in the female body. It is the mucous uterine layer that is responsible for the attachment of the fertilized egg and the onset of a successful pregnancy. After conception, the endometrial blood vessels provide the fetus with oxygen and essential nutrients.
Proliferation of the endometrium promotes the growth of the vascular bed for normal blood supply to the embryo and the formation of the placenta. During the menstrual cycle, a number of cyclic changes occur in the uterus, divided into the following successive stages:
- The endometrium in the proliferation phase is characterized by intensive growth due to the proliferation of cellular structures through their active division. In the proliferation phase, the endometrium grows, which can be either a completely normal physiological phenomenon, part of the menstrual cycle, or a sign of dangerous pathological processes.
- Secretion phase - At this stage, the endometrial layer is prepared for the menstrual phase.
- Menstrual phase, endometrial desquamation - desquamation, rejection of the overgrown endometrial layer and its removal from the body with menstrual blood.
To adequately assess the cyclic changes of the endometrium and the extent to which its condition corresponds to the norm, it is necessary to take into account factors such as the duration of the menstrual cycle, the stages of proliferation and the secretive period, the presence or absence of dysfunctional uterine bleeding.
Phases of endometrial proliferation
The process of endometrial proliferation includes several successive stages, which corresponds to the concept of normality.
The absence of one of the phases or failures in its course may mean the development of a pathological process. The entire period takes two weeks.
During this cycle, follicles mature, stimulating the secretion of the hormone estrogen, under the influence of which the endometrial uterine layer grows.
The following stages of the proliferation phase are distinguished:
- Early - lasts from 1 to 7 days of the menstrual cycle. At the early stage of the phase, the uterine mucosa changes. Epithelial cells are present on the endometrium. Blood arteries practically do not twist, and stromal cells have a specific shape that resembles a spindle.
- The middle phase is a short phase that occurs between the 8th and 10th days of the menstrual cycle. The endometrial layer is characterized by the formation of certain cellular structures formed during indirect division.
- The late stage lasts from 11 to 14 days of the cycle. The endometrium is covered with convoluted glands, the epithelium is multilayered, the cell nuclei are round in shape and large in size.
The stages listed above must meet the established norm criteria, and they are also inextricably linked with the secretory phase.
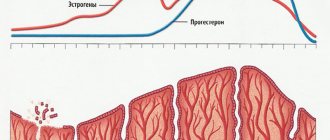
Phases of endometrial secretion
The secretory endometrium is dense and smooth. Secretory transformation of the endometrium begins immediately after completion of the proliferation stage.
Experts distinguish the following stages of secretion of the endometrial layer:
- Early stage - observed from 15 to 18 days of the menstrual cycle. At this stage, secretion is very weakly expressed, the process is just beginning to develop.
- The middle stage of the secretion phase occurs from days 21 to 23 of the cycle. This phase is characterized by increased secretion. A slight suppression of the process is noted only at the end of the stage.
- Late - for the late stage of the secretion phase, suppression of secretory function is typical, which reaches its peak at the onset of menstruation itself, after which the process of reverse development of the endometrial uterine layer begins. The late phase is observed in the period from 24-28 days of the menstrual cycle.
Proliferative diseases
Proliferative endometrial diseases - what does this mean? Typically, the secretory type endometrium poses virtually no threats to a woman’s health. But the mucous uterine layer during the proliferative phase grows intensively under the influence of certain hormones.
This condition carries a potential danger in terms of the development of diseases caused by pathological, increased division of cellular structures. The risks of developing tumors, both benign and malignant, increase.
Among the main pathologies of the proliferative type, doctors identify the following:
Hyperplasia is a pathological growth of the uterine endometrial layer.
This disease is manifested by such clinical signs as:
- menstrual irregularities,
- uterine bleeding,
- pain syndrome.
With hyperplasia, the reverse development of the endometrium is disrupted, the risks of infertility increase, reproductive dysfunction and anemia develop (against the background of heavy blood loss). The likelihood of malignant degeneration of endometrial tissue and the development of cancer also increases significantly.
Endometritis is an inflammatory process localized in the mucous membrane of the uterine endometrial layer.
This pathology manifests itself:
- uterine bleeding,
- heavy, painful menstruation,
- vaginal discharge of a purulent-bloody nature,
- aching pain localized in the lower abdomen,
- painful intimate contacts.
Endometritis also negatively affects the reproductive functions of the female body, provoking the development of complications such as problems with conception, placental insufficiency, the threat of miscarriages and spontaneous termination of pregnancy in the early stages.
Uterine cancer is one of the most dangerous pathologies developing in the proliferative period of the cycle.
Patients over 50 years of age are most susceptible to this malignant disease. The disease manifests itself as active exophytic growth simultaneously with concomitant infiltrating germination into muscle tissue. The danger of this type of oncology lies in its practically asymptomatic course, especially in the early stages of the pathological process.
The first clinical sign is leucorrhoea - vaginal discharge of a mucous nature, but, unfortunately, most women do not pay special attention to this.
Clinical symptoms such as:
- uterine bleeding,
- pain localized in the lower abdomen,
- increased urge to urinate,
- bloody vaginal discharge,
- general weakness and increased fatigue.
Doctors note that most proliferative diseases develop against the background of hormonal and gynecological disorders. The main provoking factors include endocrine disorders, diabetes mellitus, uterine fibroids, endometriosis, hypertension, and excess body weight.
- In the high-risk group, gynecologists include women who have undergone abortions, miscarriages, curettage, surgical interventions on the organs of the reproductive system, and who abuse hormonal contraceptives.
- To prevent and timely detect such diseases, it is necessary to monitor your health, and be examined by a gynecologist at least 2 times a year for the purpose of prevention.
The danger of suppressing proliferation
Inhibition of proliferative processes in the endometrial layer is a fairly common phenomenon, characteristic of the menopause and the decline of ovarian functions.
In patients of reproductive age, this pathology is fraught with the development of hypoplasia and dysmenorrhea.
During processes of a hypoplastic nature, thinning of the mucous uterine layer occurs, as a result of which the fertilized egg cannot attach normally to the wall of the uterus, and pregnancy does not occur.
The disease develops against the background of hormonal disorders and requires adequate, timely medical care.
Proliferative endometrium - a growing mucous uterine layer, can be a manifestation of the norm or a sign of dangerous pathologies. Proliferation is characteristic of the female body. During menstruation, the endometrial layer is shed, after which it is gradually restored through active cell division.
For patients with reproductive disorders, it is important to take into account the stage of endometrial development when conducting diagnostic examinations, since in different periods the indicators may have significant differences.
Source:
What is proliferative endometrium?
To find out what proliferative endometrium is, it is necessary to understand how the female body functions. The inside of the uterus, lined with the endometrium, experiences cyclic changes throughout the menstrual period.
The endometrium is a mucous layer covering the inner plane of the uterus, abundantly supplied with blood vessels and serving to supply the organ with blood.
Purpose and structure of the endometrium
According to its structure, the endometrium can be divided into two layers: basal and functional.
The peculiarity of the first layer is that it hardly changes and is the basis for the regeneration of the functional layer in the next menstrual period.
It consists of a layer of cells tightly adjacent to one another, connecting tissues (stroma), equipped with glands and a large number of branched blood vessels. In normal condition, its thickness varies from one to one and a half centimeters.
Unlike the basal layer, the functional layer constantly experiences changes. This is due to damage to its integrity as a result of peeling due to blood leakage during menstruation, the birth of a child, artificial termination of pregnancy, and curettage during diagnostics.
The endometrium is designed to perform several functions, the main one of which is to provide the necessary conditions for the onset and successful course of pregnancy, when the number of glands and blood vessels included in the structure of the placenta increases. One of the purposes of a child's place is to supply the embryo with nutrients and oxygen. Another function is to prevent the opposing walls of the uterus from sticking together.
Changes occur monthly in the female body, during which favorable conditions are created for conception and gestation. The period between them is called the menstrual cycle and lasts from 20 to 30 days. The beginning of the cycle is the first day of menstruation.
Any deviations that arise during this period indicate the presence of any disturbances in the woman’s body. The cycle is divided into three phases:
- proliferation;
- secretion;
- menstruation.
Proliferation is the process of cell reproduction by division, leading to the growth of body tissues. Endometrial proliferation is an increase in the tissue of the mucous membrane inside the uterus as a result of the division of normal cells. The phenomenon can occur as part of the menstrual cycle or have a pathological origin.
The duration of the proliferation phase is about 2 weeks. The changes that occur in the endometrium during this period arise due to an increase in the amount of the hormone estrogen, which is produced by the maturing follicle. This phase includes three stages: early, middle and late.
The early stage, which lasts from 5 days to 1 week, is characterized by the following: the surface of the endometrium is covered with cylindrical epithelial cells, the glands of the mucous layer resemble straight tubes, in a cross section the outlines of the glands are oval or round; the epithelium of the glands is low, the cell nuclei are located at their base, are oval in shape and intensely colored. Cells connecting tissues (stroma) are spindle-shaped with large nuclei. The blood arteries are almost not tortuous.
The middle stage, which occurs on the eighth to tenth day, is characterized by the fact that the plane of the mucous membrane is covered with tall epithelial cells of a prismatic appearance.
Source: https://rdbkomi.ru/zabolevaniya/fazy-poliferatsii-endometriya-norma-i-otkloneniya.html
Secretory type
During the menstrual cycle, most of the endometrium dies, but when menstruation occurs, it is restored through cell division. After five days, the structure of the endometrium becomes renewed and is quite thin. The endometrium of the secretory type uterus has an early and late phase. It has the ability to grow and with the onset of menstruation it increases several times. In the first stage, the inner lining of the uterus is covered with cylindrical low epithelium, which has tubular glands. In the second cycle, the endometrium of the secretory type uterus is covered with a thick layer of epithelium. The glands in it begin to lengthen and take on a wavy shape.
In the secretory stage, the endometrium changes its original shape and increases significantly in size. The structure of the mucous membrane becomes saccular, glandular cells appear through which mucus is secreted. The secretory endometrium is characterized by a dense and smooth surface with a basal layer. However, he does not show activity. The secretory type of endometrium coincides with the period of formation and further development of follicles.
Glycogen gradually accumulates in the stromal cells, and a certain part of them is transformed into decidual cells. At the end of the period, the corpus luteum begins to involute, and progesterone stops working. In the secretory phase of the endometrium, glandular and glandular-cystic hyperplasia can develop.
Interpretation of endometrial biopsy results
On average, deciphering the results of an endometrial biopsy takes 1-2 weeks.
This depends on the operating mode of the pathology laboratory and the complexity of the stains used. The method of taking a biopsy of the uterine mucosa also plays a significant role - in some cases, the morphologist receives whole fragments of tissue with a preserved histological structure, while in others there is a high probability of receiving only blood clots.
Biopsy techniques
Most often, an endometrial biopsy is taken by traditional diagnostic curettage (CDC).
The resulting material consists of separate sections of the mucous membrane, in which the uterine glands, connective tissue stroma and their relationships with each other are clearly visible.
If the sample contains malignant elements, the pathologist can accurately determine the depth of their germination, and this directly affects the treatment tactics and prognosis of the disease.
Unlike RDV, during
endometrial aspiration and pipel biopsy, the doctor does not receive complete layers of the mucosa, but its scattered elements with a large admixture of blood.
Often the biomaterial is represented by nothing more than a meager accumulation of individual cells, from which it is impossible to reliably judge the nature of the pathological process. From the point of view of the diagnostic value of the results of endometrial biopsy, preference should be given to separate diagnostic curettage.
However, in some cases, a comprehensive interpretation of biopsy specimens is not required. Thus, a pipel biopsy is usually performed to assess the condition of the endometrium before the IVF procedure.
In this situation, even scattered elements of the mucosa are enough to determine the type of pathology.
In his conclusion, the pathologist can give a different interpretation of the endometrial biopsy, with or without a detailed description of the morphology. Often the results are accompanied by a pathological diagnosis, which is a brief summary of the descriptive characteristics.
Below is an explanation of the various terms that can be found in the results of an endometrial biopsy.
- Adenocarcinoma is a synonym for uterine cancer.
- Adenomyosis is the growth of the uterine glands in the myometrium (the muscular lining of the uterus). A rare find, mainly in RDV.
- Atrophic mucosa - thinned endometrium with single glands. Quite normal during menopause; at a younger age indicates serious hormonal imbalances.
- Chorionic villi are auxiliary components of the fertilized egg, thanks to which it attaches to the uterine mucosa. Subsequently, they transform into the placenta. The presence of chorionic villi in endometrial scraping is an unambiguous sign of pregnancy.
- Hyalinosis is a thickening and narrowing of the lumen of small uterine arteries.
- Atypical hyperplasia is the proliferation of endometrial glands with signs of malignant transformation. Potentially precancerous condition.
- Simple hyperplasia is the same thing, but without signs of a tumor. Occurs with hormonal disorders due to ovarian cysts and other conditions.
- Hypoplastic mucosa is a thinned endometrium, occupying an intermediate state between mature and atrophic.
- Gravidar mucosa is the endometrium of the pregnant uterus with fields of decidual tissue.
- Detritus is a designation for amorphous masses represented by the remains of dead cells.
- Decidual tissue is a collection of large cells containing an abundance of nutrients. Sign of pregnancy.
- Dysplasia is a change in the structure and cellular composition of the uterine glands, reminiscent of tumor transformation.
- A cyst is an enlarged gland filled with fluid.
- Leiomyoma is a benign tumor of smooth muscle located in the middle lining of the uterus.
- Lymphoid follicles are accumulations of lymphocytes that reflect a long-term inflammatory process (for example, chronic endometritis).
- Menstrual mucosa - endometrium at the height of menstruation.
- Metaplasia is a condition in which the normal epithelium of the uterine mucosa is replaced by epithelium characteristic of another organ.
- Placental polyp - remnants of the placenta after a miscarriage, abortion or natural birth (less often after a cesarean section).
- A polyp is any formation of the mucous membrane protruding into the lumen of the uterus.
- Hydatidiform mole is a pathology of pregnancy, a variant of trophoblastic disease. Characterized by the growth of chorionic villi alone; the fetus is not formed.
- The Arias-Stella reaction is a variant of changes in the endometrium, reminiscent of the transformation of the glands of the cervical canal during pregnancy. Indicates a hyperplastic process.
- Regenerating mucosa - endometrium in the first 1-3 days after menstruation.
- Spiral arteries are small blood vessels that penetrate the lining of the uterus. The main source of its blood supply.
- Stroma is the tissue in which the endometrial glands are embedded.
- Trophoblast is the cellular material from which chorionic villi and other auxiliary structures of the embryo are formed.
- The proliferation phase corresponds to days 5-14 of the menstrual cycle (after menstruation).
- The secretion phase corresponds to days 15-26 of the menstrual cycle (before menstruation).
- Fibrosis is the proliferation of dense connective tissue in the stroma. A sign of chronic inflammation, and also a normal phenomenon in postmenopause.
- Choriocarcinoma is a malignant tumor of atypical chorionic villi, a variant of trophoblastic disease. To put it roughly, choriocarcinoma is a “cancerous hydatidiform mole.”
- Endometritis is an inflammation of the uterine mucosa.
Following actions
Further tactics depend on the method used to take the biopsy. If the results of an aspiration or pipel biopsy reveal hyperplasia and signs of atypia, then this in most cases serves as an indication for separate diagnostic curettage.
If, in addition to indicating the phase of the cycle and the presence of blood or detritus, nothing else is indicated in the conclusion, then in fact this indicates the absence of any pathology on the part of the endometrium.
Subsequent actions by the patient and the gynecologist should be aimed at excluding other causes of dysfunctional uterine bleeding.
The presence of tumor changes, including atypical hyperplasia, requires regular follow-up and consultation with a gynecological oncologist. The stage of the cancer process is determined and complex treatment is prescribed, including surgery, chemotherapy and radiation therapy.
Treatment in Israel
Israeli gynecologists have significant experience in treating various diseases of the uterus. Using modern technologies, doctors at the Top Ichilov Clinic accurately determine the likelihood of malignant degeneration of tumors and carry out their excision using minimally invasive methods.
To find out more detailed information regarding your case, fill out the form below.
For non-surgical treatment, Top Ichilov uses the latest drugs, the effectiveness of which exceeds 90%, and advanced techniques: brachytherapy, photodynamic therapy, radiotherapy using the TrueBeam and many others.
If there is no choice left and it is necessary to
surgically remove a tumor or even the uterus, Top Ichilov often uses a Da Vinci .
This operation completely eliminates the possibility of medical error and prevents complications. Source: https://ProBiopsii.ru/rasshifrovka-rezultatov-biopsii-jendometrija/
Causes of glandular cystic hyperplasia
Glandular cystic hyperplasia occurs in women of all ages. In most cases, formations occur in the secretory type of endometrium during the period of hormonal changes.
Congenital causes of glandular cystic hyperplasia include:
- hereditary genetic abnormalities;
- hormonal imbalance during puberty in adolescents.
Acquired pathologies include:
- problems of hormonal dependence - endometriosis and mastopathy;
- inflammatory processes in the genital organs;
- infectious pathologies in the pelvic organs;
- gynecological manipulations;
- curettage or abortion;
- disturbances in the proper functioning of the endocrine system;
- excess body weight;
- polycystic ovary syndrome;
- arterial hypertension;
- depressed function of the liver, mammary gland and adrenal glands.
Clinical manifestations
Glandular cystic hyperplasia, which forms in the secretory endometrium, is manifested by the following symptoms.
- Menstrual irregularities. Spotting between periods.
- The discharge is not profuse, but with bloody, dense clots. With prolonged blood loss, patients may experience anemia.
- Pain and discomfort in the lower abdomen.
- Lack of ovulation.
Pathological changes can be determined at the next preventive examination by a gynecologist. Glandular cystic hyperplasia of the secretory endometrium does not resolve on its own, so it is important to seek help from a qualified doctor in a timely manner. Only after a comprehensive diagnosis will a specialist be able to prescribe therapeutic treatment.
Diagnostic methods
Glandular cystic hyperplasia of the secretory endometrium can be diagnosed using the following diagnostic methods.
- Diagnostic examination by a gynecologist.
- Analysis of the patient’s medical history, as well as determination of hereditary factors.
- Ultrasound examination of the uterine cavity and pelvic organs. A special sensor is inserted into the uterus, thanks to which the doctor examines and measures the endometrium of the secretory type of uterus. He also checks for polyps, cystic formations or nodules. But ultrasound does not give the most accurate result, so patients are prescribed other examination methods.
- Hysteroscopy. This examination is carried out with a special medical optical apparatus. During diagnosis, differential curettage of the secretory endometrium of the uterus is performed. The resulting sample is sent for histological examination, which will determine the presence of pathological processes and the type of hyperplasia. This technique should be carried out before the onset of menstruation. The results obtained are the most informative, so gynecologists will be able to make a correct and accurate diagnosis. With the help of hysteroscopy, it is possible not only to determine the pathology, but also to perform surgical treatment of the patient.
- Aspiration biopsy. During a gynecological examination, the doctor scrapes the secretory endometrium. The resulting material is sent for histology.
- Histological examination. This diagnostic method determines the morphology of the diagnosis, as well as the type of hyperplasia.
- Laboratory tests to determine the level of hormones in the body. If necessary, hormonal disorders are checked in the thyroid gland and adrenal glands.
Only after a thorough and comprehensive examination will the doctor be able to make the correct diagnosis and prescribe effective treatment. The gynecologist will individually select medications and their exact dosages.
I did a pipette biopsy of the endometrium at 21 dc, the histology result: “endometrium in the middle stage of the secretion phase” and that’s it! does this mean everything is normal? Continue reading →
Hello everyone, I received the histology result: the endometrium corresponds to the secretion phase, see the doctor on Monday, is everything normal with me?