In progress uterine cycle
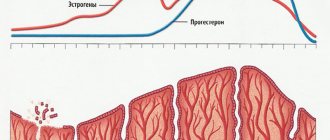
ovarian hormones produced in the follicle and corpus luteum influence cyclic changes in the tone, excitability and blood supply of the uterus. More significant cyclic changes occur in the endometrium. Their essence lies in the correctly repeating process of proliferation, in the qualitative change, rejection and restoration of the layer of the mucous membrane, which faces the lumen of the uterus. This layer, which undergoes cyclical changes, is called the functional layer of the endometrium. The layer of the mucous membrane adjacent to the muscular layer of the uterus does not undergo cyclic changes and is called the basal layer.
The uterine cycle, like the ovarian cycle, lasts 28 days (less often 21 or 30-35 days). It consists of: desquamation phase, regeneration phase, proliferation phase and secretion phase.
Desquamation phase
manifested by bleeding that lasts 3-5 days (menstruation). The functional layer of the mucous membrane, under the influence of enzymes, disintegrates, is rejected and is released out along with the contents of the uterine glands and blood from ruptured vessels. The phase of endometrial desquamation coincides with the beginning of the death of the corpus luteum in the ovary.
Regeneration phase
mucous membrane begins during the period of desquamation and ends 5-6 days from the beginning of menstruation. Restoration of the functional layer of the mucous membrane occurs due to the proliferation of the epithelium of the remnants of the glands located in the basal layer, and through the proliferation of other elements of this layer (stroma, vessels, nerves). Regeneration is due to the influence formed in the follicle, the development of which begins after the death of the corpus luteum.
Proliferation phase
endometrium coincides with the maturation of the follicle in the ovary and continues until the 14th day of the cycle (with a 21-day cycle up to 10-11 days). Under the influence of the estrogen hormone, which affects the nervous elements and metabolic processes in the uterus, proliferation or growth of the stroma and growth of the mucous membrane occur. The glands stretch out in length, then twist like a corkscrew, but do not contain a secretion. The mucous membrane of the uterus thickens 4-5 times during this period.
Secretion phase
coincides with the development of the corpus luteum in the ovary and lasts from the 14th-15th to the 28th day, i.e. until the end of the cycle.
Under the influence of the corpus luteum hormone, important qualitative transformations occur in the uterine mucosa. The glands produce secretions, their cavity expands, and bay-shaped protrusions form in the walls. The stromal cells become enlarged and slightly rounded, resembling the decidual cells produced during pregnancy. Glycogen, phosphorus, calcium and other substances are deposited in the mucous membrane.
As a result of these changes in the mucous membrane, conditions are created that are favorable for the development of the embryo if fertilization occurs. At the end of the secretion phase, serous permeation of the stroma is noted, and diffuse leukocyte infiltration of the functional layer appears. The vessels of this layer lengthen, acquire a spiral shape, dilations form in them, and the number of anastomoses increases.
Endometrial hyperplasia is a pathology of the uterine body, which is characterized by a strong proliferation of the inner layer of the uterus. The disorder can occur in women of all ages. Most often it is provoked by hormonal imbalances. Also, the reason may lie in inflammation, curettage and abortion, and serious somatic pathologies. What is hyperplasia and how often does it occur?
This pathology is diagnosed frequently. It occurs in approximately 5% of patients suffering from gynecological disorders. As a rule, this process appears in women during menopause. It also often occurs during adolescence. Thus, common causes of occurrence are due to hormonal changes.
Hyperplasia of the endometrium of the uterus and the menstrual cycle have a certain connection. Normally, it includes several components:
- proliferation - at this stage the functional layer of the endometrium grows;
- secretion – maturation of the endometrium occurs;
- desquamation - the main layer is rejected, which causes bleeding.
The initial stage takes place on the first day of menstruation. In the middle of the cycle, ovulation occurs, which is characterized by the release of an egg from the ovary. This process may be accompanied by mucous transparent discharge.
In the absence of fertilization, the egg leaves the body with a functional layer of the endometrium, and menstruation begins. At this stage, the woman begins to experience bloody discharge. This process is carried out under the influence of sex hormones. Thus, estrogen is responsible for the proliferation stage, and progesterone is responsible for the secretion stage.
Also during proliferation, cell death occurs - atoposis. Thanks to this, the endometrium cannot grow excessively. Atoposis occurs exclusively in the presence of ovulation. If a woman experiences an anovulatory cycle, the endometrium thickens, which provokes the appearance of hyperplasia.
In menopause
During the menopausal period, the mucous membrane should not grow. The norm of the endometrium is 4-5 mm. Gradually the functional layer atrophies, menstruation is absent. If an ultrasound revealed a size of up to 6 mm, the woman is offered observation.
Upon reaching the age of 35, the ovarian reserve of the appendages in women begins to decline, but the first symptoms of decline in reproductive function are noted only at the age of 45. Due to a decrease in estrogen production, the endometrial layer grows more slowly during the days of the cycle.
During menopause, indicators by day of the uterine mucosa are usually at the lower threshold of normal or much lower, and depend on how long ago menopause began:
- less than 5 years – the endometrium grows up to 5 mm;
- more than 5 years – maximum 4 mm;
- more than 10–15 years - the layer is so thin that ultrasound cannot determine its thickness.
Bleeding phase
In the phase of menstruation or bleeding, the desquamation stage (twenty-eighth - second day) is characterized by an increase in changes that are noted for the late secretory stage. The process of endometrial rejection begins from the surface layer and is focal in nature. Desquamation ends completely by the third day of menstruation. A morphological sign of the monthly phase is the detection of collapsed star-shaped glands in necrotic tissue. The regeneration process (the third or fourth day) is carried out from the tissues of the basal layer. By the fourth day, the mucous membrane is normally epithelialized. Impaired endometrial rejection and regeneration can be caused by slow processes or incomplete endometrial rejection.
The abnormal state of the endometrium is characterized by so-called hyperplastic proliferative changes (glandular-cystic hyperplasia, glandular hyperplasia, adenomatosis, mixed form of hyperplasia), as well as hypoplastic conditions (non-functioning, resting endometrium, transitional endometrium, hypoplastic, dysplastic, mixed endometrium).
The most important and interesting news about infertility treatment and IVF is now in our Telegram channel @probirka_forum Join us!
Causes
When endometrial hyperplasia occurs, the reasons may be different. The provoking factor is an absolute or relative increase in estrogen levels in the blood. Various factors can lead to this condition:
- age-related disorders of the regulation of sex hormones - the amount of estrogen often changes before menopause;
- polycystic ovary syndrome;
- hormonal abnormalities - increased estrogen levels due to a lack of progesterone;
- hormone-producing tumor lesions of the ovaries;
- improper use of hormonal drugs;
- frequent abortions;
- disruption of the adrenal cortex;
- performing curettage for diagnostic purposes;
- hereditary tendency;
- inflammatory lesions of the female genital organs;
- the appearance of other pathologies - hypertension, diabetes, disorders of the mammary glands or thyroid gland.
After childbirth, this process is not observed too often. However, in some cases, the pathology recurs after the birth of the child. Most often this occurs with an atypical and focal form of the disease.
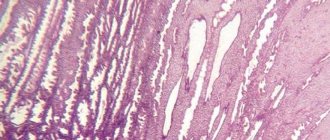
One of the most common functional diagnostic tests is histological examination of endometrial scrapings. For the purposes of functional diagnostics, the so-called “line scraping” is usually used, in which a small strip of the endometrium is taken with a small curette. Clinical, morphological and differential diagnosis of the phases of the 28-day menstrual cycle based on endometrial structures is clearly given in the work of O. I. Topchieva (1967) and can be recommended for practical use. The whole is divided into 3 phases: proliferation, secretion, bleeding, and the phases of proliferation and secretion are divided into early, middle and late stages, and the bleeding phase into desquamation and regeneration.
When assessing changes occurring in the endometrium, it is necessary to take into account the duration of the cycle, its clinical manifestations (presence or absence of premenstrual and postmenstrual bleeding, duration of menstrual bleeding, amount of blood loss, etc.).
Early stage of the proliferation phase
(5-7th day) is characterized by the fact that the surface of the mucosa is lined with cubic epithelium, the endometrial glands look like straight tubes with a narrow lumen, on a cross section the contours of the glands are round or oval; the epithelium of the glands is prismatic, low, the nuclei are oval, located at the base of the cells, intensely colored. The stroma consists of spindle-shaped cells with large nuclei. The spiral arteries are slightly tortuous.
In the middle stage (8-10th day), the surface of the mucosa is lined with high prismatic epithelium. The glands are slightly convoluted. Numerous mitoses are detected in the nuclei. A mucus border may be found at the apical edge of some cells. The stroma is swollen and loosened.
In the late stage (days 11-14), the glands acquire a tortuous outline. Their lumen is expanded, the nuclei are located at different levels. In the basal sections of some cells, small vacuoles containing glycogen begin to be detected. The stroma is juicy, the nuclei are enlarged, rounded and stained less intensely. The vessels take on a convoluted shape.
The described changes, characteristic of a normal cycle, can occur in pathology: a) during the second half of the menstrual cycle during anovulatory cycles; b) with dysfunctional uterine bleeding due to anovulatory processes; c) with glandular hyperplasia - in various parts of the endometrium.
If tangles of spiral vessels are found in the functional layer of the endometrium of the proliferation phase, this indicates that the previous cycle was two-phase, and during the next menstruation the entire functional layer was not rejected and it only underwent reverse development.
In the early stage of the secretion phase
(15-18th day) subnuclear vacuolization is detected in the epithelium of the glands; vacuoles push the nuclei into the central parts of the cell; the nuclei are located at the same level; vacuoles contain glycogen particles. The lumens of the glands are enlarged, and traces of secretion may already be detected in them. The endometrial stroma is juicy and loose. The vessels become even more convoluted. A similar structure of the endometrium can occur with the following hormonal disorders: a) with an inferior corpus luteum at the end of the menstrual cycle; b) with a delayed onset of ovulation; c) with cyclic bleeding that occurs as a result of the death of the corpus luteum, which has not reached the flowering stage; d) with acyclic bleeding caused by the early death of an inferior corpus luteum.
In the middle stage of the secretion phase (days 19-23), the lumens of the glands are expanded, their walls become folded. Epithelial cells are low, filled with secretions that are released into the lumen of the gland. In the stroma, by the 21st-22nd day, a decidua-like reaction begins to occur. The spiral arteries are sharply tortuous and form tangles, which is one of the most reliable signs of a full luteal phase. A similar structure of the endometrium can be observed with prolonged and increased function of the corpus luteum or with taking large doses of progesterone, with an early uterine pregnancy (outside the implantation zone), with progressive ectopic pregnancy.
In the late stage of the secretion phase (days 24-27), due to regression of the corpus luteum, the juiciness of the tissue decreases; the functional layer decreases in height. The folding of the glands increases, acquiring a sawtooth shape in longitudinal sections and a stellate shape in transverse sections. There is a secret in the lumen of the glands. The perivascular decidua-like reaction of the stroma is intense. Spiral vessels form coils closely adjacent to each other. By the 26-27th day, the venous vessels are filled with blood with the formation of blood clots. Infiltration with leukocytes occurs in the stroma of the compact layer; focal hemorrhages and areas of edema appear and increase. This condition must be differentiated from endometritis, in which the cellular infiltrate is localized mainly around the vessels and glands.
In the phase of bleeding (menstruation) for the desquamation stage (28-2nd day), an increase in the changes noted for the late secretory stage is characteristic. Rejection of the endometrium begins from the superficial layers and is focal in nature. Complete desquamation is completed by the third day of menstruation. A morphological sign of the menstrual phase is the discovery of collapsed glands with stellate outlines in necrotic tissue. Regeneration (3-4th day) occurs from the tissues of the basal layer. By the fourth day, the mucous membrane is normally epithelialized. Impaired rejection and regeneration of the endometrium may be due to a slowdown in the process or incomplete rejection with reverse development of the endometrium.
The pathological state of the endometrium is characterized by so-called hyperplastic proliferative changes (glandular hyperplasia, glandular-cystic hyperplasia, mixed form of hyperplasia, adenomatosis) and hypoplastic conditions (resting, non-functioning endometrium, transitional endometrium, dysplastic, hypoplastic, mixed endometrium).
The menstrual cycle plays a big role in a woman's life. By its course, duration and delay of menstruation, one can determine disorders in reproductive health, pregnancy and the beginning of the decline of reproductive function. Therefore, every woman is recommended to keep her own menstrual cycle calendar in order to calculate the most favorable days for conception or, conversely, “safe” days.
Menstrual cycle
The menstrual cycle (from the Latin word menstruus) literally means “lunar” cycle. The menstrual cycle is a periodic change in the female body aimed at the possibility of conception. Its duration is individual for each woman and depends on the physiological processes in the woman’s body, and does not depend in any way on the phases of the moon. On average, its duration is 28 days, but can range from 21 days to 35. The beginning of the menstrual cycle is considered the first day of menstruation.
Menarche
Menarche is the first menstrual cycle, which is the main event of puberty, indicating the possibility of conception. On average, menarche occurs at age twelve, but the onset of the first menstruation can range from 8 to 16 years. It depends on heredity, social factors, past diseases, climatic conditions and nationality. Only 30% of girls develop a regular menstrual cycle very quickly. For others it takes at least a year.
Stopping the menstrual cycle
The cessation of the menstrual cycle or menopause occurs, on average, at the age of 40-58 years. During this period, reproductive function declines, and it also depends on hereditary factors, chronic diseases or surgical interventions. But today the concepts of “menopause” and “menopause” are becoming less and less common. The following terminology is considered more accepted:
- premenopausal period – from 45 years to the onset of menopause;
- perimenopausal period – premenopausal period and two years after menopause;
- menopause is the last menstruation, which occurs on average at age 50;
- postmenopausal period - starting after menopause and lasting until the death of the woman.
Phases of the menstrual cycle
There are four phases of the menstrual cycle:
- follicular phase;
- ovulatory phase;
- secretory phase;
- desquamation phase.
Follicular phase
The follicular phase begins on the first day of the menstrual cycle. At this time, the dominant follicle matures, from which a mature egg will subsequently be released. Its duration is different for each woman, from 7 to 22 days, and on average it is 14 days. At this time, the endometrium begins to grow and thicken in the uterus, which is preparing to receive a fertilized egg.
Ovulatory phase
By the seventh day, a dominant follicle is determined, which continues to grow and secretes estradiol, while other follicles undergo reverse development during this period. This phase lasts three days, during which the luteinizing hormone (LH) is released, under the influence of which the dominant follicle bursts and a mature egg is released. That is, ovulation occurs in the next 24 hours. In order to get pregnant, it is necessary to calculate the day of ovulation in advance, since the egg does not exist for a long time, and sperm remain viable for up to three days. Therefore, sexual intercourse must occur in advance, before ovulation, so that sperm have time to penetrate the fallopian tube and meet a mature egg.
Every month, a woman’s body undergoes changes associated with hormonal cyclic fluctuations. One of the manifestations of such changes is menstrual bleeding. But this is only the visible part of a complex mechanism aimed at maintaining a woman’s reproductive function. It is very important that the mucous layer of the uterus - the endometrium - has a normal thickness throughout the entire cycle. What thickness of the endometrium before, during and after menstruation is considered normal?
Women's menstrual cycle
Changes occur in the female body every month that help create optimal conditions for conceiving and bearing a child. The period between them is called the menstrual cycle. On average, its duration is 20-30 days. The beginning of the cycle is the first day of menstruation. At the same time, the endometrium is renewed and cleansed.
If women experience abnormalities during the menstrual cycle, this indicates serious disorders in the body. The cycle is divided into several phases:
Proliferation refers to the processes of reproduction and cell division that contribute to the growth of internal tissues of the body. During the proliferation of the endometrium, normal cells begin to divide in the mucous membrane of the uterine cavity. Such changes may occur during menstruation or have a pathological origin.
The duration of proliferation is on average up to two weeks. In a woman’s body, estrogen begins to increase rapidly, which is produced by an already mature follicle. This phase can be divided into early, middle and late stages. At an early stage (5-7 days) in the uterine cavity, the surface of the endometrium is covered with epithelial cells, which have a cylindrical shape. In this case, the blood arteries remain unchanged.
The middle stage (8-10 days) is characterized by the covering of the plane of the mucous membrane with epithelial cells, which have a prismatic appearance. The glands are distinguished by a slightly convoluted shape, and the nucleus has a less intense shade and increases in size. A huge number of cells appear in the uterine cavity, which arose as a result of division. The stroma becomes swollen and quite loose.
The late stage (11-15 days) is characterized by a single-layer epithelium, which has many rows. The gland becomes tortuous, and the nuclei are located at different levels. Some cells contain small vacuoles that contain glycogen. The vessels have a tortuous shape, the cell nuclei gradually acquire a rounded shape and greatly increase in size. The stroma becomes engorged.
The endometrium of the secretory type uterus can be divided into several stages:
- early (15-18 days of the menstrual cycle);
- medium (20-23 days, pronounced secretion is observed in the body);
- late (24-27 days, secretion gradually fades away in the uterine cavity).
The menstrual phase can be divided into several periods:
- Desquamation. This phase occurs from day 28 to day 2 of the menstrual cycle and occurs when fertilization has not occurred in the uterine cavity.
- Regeneration. This phase lasts from the third to fourth day. It begins before the complete separation of the functional layer of the endometrium along with the beginning of the growth of epithelial cells.
Phases of endometrial proliferation: norm and deviations
The inner layer of the uterus is called the endometrium. This fabric has a complex structural structure and a very important role. The reproductive functions of the body depend on the condition of the mucous membrane.
Every month throughout the cycle, the density, structure and size of the inner layer of the uterus changes. The proliferation phase is the very first stage of the natural transformations of the mucous membrane that begin. It is accompanied by active cell division and proliferation of the uterine layer.
The state of the proliferative endometrium directly depends on the intensity of division. Disturbances in this process lead to abnormal thickening of the resulting tissues.
Too many cells have a negative impact on health and contribute to the development of serious diseases. Most often, when examined in women, glandular endometrial hyperplasia is detected.
There are other, more dangerous diagnoses and conditions that require emergency medical attention.
Features of endometrial proliferation
For successful fertilization and a trouble-free pregnancy, cyclic changes in the uterus must correspond to normal values. In cases where an atypical structure of the endometrium is observed, pathological deviations are possible.
It is very difficult to find out about the unhealthy state of the uterine mucosa by symptoms and external manifestations. Doctors will help with this, but to make it easier to understand what endometrial proliferation is and how tissue proliferation affects health, it is necessary to understand the features of cyclical changes.
The endometrium consists of functional and basal layers. The latter consists of tightly adjacent cellular particles penetrated by numerous blood vessels. its function is to restore the functional layer, which, if fertilization fails, peels off and is excreted with the blood.
The uterus cleanses itself after menstruation, and the mucous membrane during this period has a smooth, thin, even structure.
The standard menstrual cycle is usually divided into 3 stages:
- Proliferation.
- Secretion.
- Bleeding (menstruation).
In this order of natural changes, proliferation comes first. The phase begins approximately on the 5th day of the cycle after the end of menstruation and lasts 14 days. During this period, cellular structures multiply through active division, which leads to tissue proliferation.
The inner layer of the uterus can increase up to 16 mm. This is the normal structure of the endometrial layer of the proliferative type.
This thickening helps to attach the embryo to the villi of the uterine layer, after which ovulation occurs, and the uterine mucosa enters the secretion phase in the endometrium.
If conception has occurred, the corpus luteum is implanted into the uterus. If a pregnancy fails, the embryo stops functioning, hormone levels decrease, and menstruation begins.
Normally, the stages of the cycle follow each other in exactly this sequence, but sometimes failures occur in this process.
For various reasons, proliferation may not stop, that is, after 2 weeks, cell division will continue uncontrollably and the endometrium will grow.
Too dense and thick inner layer of the uterus often leads to problems with conception and the development of serious diseases.
Proliferative diseases
Intensive growth of the uterine layer during the proliferative phase occurs under the influence of hormones. Any disruption in this system prolongs the period of cell division activity. An excess of new tissue causes uterine cancer and the development of benign tumors. Background pathologies can provoke the occurrence of diseases. Among them:
Hyperactive cell division is observed in women with identified endocrine disorders, diabetes mellitus and hypertension. The condition and structure of the uterine mucosa are negatively affected by abortion, curettage, excess weight, and abuse of hormonal contraceptives.
Hyperplasia is most often diagnosed against the background of hormonal problems. The disease is accompanied by abnormal growth of the endometrial layer and has no age restrictions. The most dangerous periods are puberty and hyperplasia during menopause. In women under 35 years of age, the disease is rarely detected, since hormonal levels at this age are stable.
Endometrial hyperplasia has clinical signs: the cycle is disrupted, uterine bleeding is observed, and constant pain appears in the abdominal area. The danger of the disease is that the reverse development of the mucous membrane is disrupted. The size of the enlarged endometrium does not decrease. This leads to infertility, anemia, and cancer.
Depending on how effectively the late and early stages of proliferation occur, endometrial hyperplasia can be atypical and glandular.
Glandular hyperplasia of the endometrium
High activity of proliferative processes and intensive cell division increases the volume and structure of the uterine mucosa. With pathological growth and thickening of glandular tissues, doctors diagnose glandular hyperplasia. The main reason for the development of the disease is hormonal disorders.
There are no typical symptoms for glandular hyperplasia. The symptoms that appear are characteristic of many gynecological diseases. Most women's complaints are related to conditions during menstruation and after menstruation.
The cycle changes and is different from previous ones. Heavy bleeding is painful and contains clots. Often discharge occurs outside the cycle, which leads to anemia.
Serious blood loss causes weakness, dizziness and weight loss.
The peculiarity of this form of endometrial hyperplasia is that the newly formed particles do not divide. The pathology rarely transforms into a malignant tumor. Nevertheless, this type of disease is characterized by indomitable growth and loss of function typical of tumor formations.
Atypical
Atypical hyperplasia refers to intrauterine diseases that are associated with hypoplastic processes of the endometrium. The disease is mainly detected in women after 45 years of age. In every third out of 100, the pathology develops into a malignant tumor.
In most cases, this type of hyperplasia develops due to hormonal disruptions that activate proliferation. Uncontrolled division of cells with a disrupted structure leads to the growth of the uterine layer. In atypical hyperplasia, there is no secretory phase, as the size and thickness of the endometrium continues to grow. This leads to long, painful and heavy periods.
Severe atypia is a dangerous condition of the endometrium. Not only does active cell proliferation occur, the structure and structure of the nuclear epithelium changes.
Atypical hyperplasia can develop in the basal, functional, and simultaneously in both layers of the mucosa. The last option is considered the most severe, since there is a high probability of developing cancer.
Phases of endometrial proliferation
It is usually difficult for women to understand what the phases of endometrial proliferation are and how a violation of the sequence of stages is associated with health. Knowledge about the structure of the endometrium helps to understand the issue.
The mucosa consists of a ground substance, a glandular layer, connective tissue (stroma) and numerous blood vessels. From about the 5th day of the cycle, when proliferation begins, the structure of each of the components changes.
The entire period lasts about 2 weeks and is divided into 3 phases: early, middle, late. Each stage of proliferation manifests itself differently and takes a certain time. The correct sequence is considered the norm.
If at least one of the phases is absent or there is a malfunction in its course, the likelihood of pathologies developing in the lining inside the uterus is very high.
Early
The early stage of proliferation is days 1-7 of the cycle. The mucous membrane of the uterus during this period begins to gradually change and is characterized by the following structural transformations of tissue:
- the endometrium is lined with a cylindrical epithelial layer;
- blood vessels are straight;
- the glands are dense, thin, straight;
- cell nuclei have a rich red color and oval shape;
- the stroma is oblong, spindle-shaped.
- The thickness of the endometrium in the early proliferative phase is 2–3 mm.
Average
The middle stage of the proliferative endometrium is the shortest, usually on the 8th–10th day of the menstrual cycle. The shape of the uterus changes, noticeable changes occur in the shape and structure of other elements of the mucosa:
- the epithelial layer is lined with cylindrical cells;
- the kernels are pale;
- the glands are elongated and curved;
- connective tissue of loose structure;
- the thickness of the endometrium continues to grow and reaches 6–7 mm.
Late
On days 11–14 of the cycle (late stage), the cells inside the vagina increase in volume and swell. Significant changes occur in the uterine lining:
- the epithelial layer is high and multilayered;
- some of the glands elongate and have a wavy shape;
- the vascular network is tortuous;
- cell nuclei increase in size and have a rounded shape;
- the thickness of the endometrium in the late proliferative phase reaches 9–13 mm.
All of these stages are closely related to the secretion phase and must correspond to normal values.
Causes of uterine cancer
Cancer of the uterus is one of the most dangerous pathologies of the proliferative period. In the early stages, this type of disease is asymptomatic. The first signs of the disease include copious mucous discharge. Over time, signs such as pain in the lower abdomen, uterine bleeding with endometrial fragments, frequent urge to urinate, and weakness appear.
The incidence of cancer increases with the onset of anovulatory cycles, characteristic of people over 45 years of age. During premenopause, the ovaries still produce follicles, but they rarely mature. Ovulation does not occur, and accordingly, the corpus luteum does not form. This leads to hormonal imbalance - the most common cause of cancer.
At risk are women who have not had pregnancy or childbirth, as well as those with identified obesity, diabetes mellitus, metabolic and endocrine disorders. Background diseases that provoke cancer of the reproductive organ are polyps in the uterus, endometrial hyperplasia, fibroids, and polycystic ovaries.
Diagnosis of oncology is complicated by the condition of the uterine wall in case of cancerous lesions. The endometrium becomes loose, the fibers are located in different directions, and the muscle tissue is weakened. The boundaries of the uterus are blurred, polyp-like growths are noticeable.
Regardless of the stage of the pathological process, endometrial cancer is detected by ultrasound. To determine the presence of metastases and the location of the tumor, hysteroscopy is used. In addition, the woman is recommended to undergo a biopsy, x-ray and a series of tests (urine, blood, hemostasis study).
Timely diagnosis makes it possible to confirm or exclude the growth of a tumor, its nature, size, type and degree of spread to neighboring organs.
The role of the endometrium in female reproductive function
The structure of the endometrial layer is quite complex. The endometrium includes the following structures:
- Glandular and outer layer of epithelium;
- Main substance;
- Stroma;
- Vascular bed.
The main function of the endometrium is to ensure implantation of the embryo and its further successful development. The endometrium contributes to normal homeostasis in the uterine cavity, which ensures the normal functioning of the fetus. Proliferation of the endometrium leads to the proliferation of the vascular bed, which improves blood supply to the fetus. These vascular structures will subsequently become part of the placenta.
Throughout the month, cyclical changes occur in the uterus. They include the following stages:
- Proliferation stage;
- Presecretory stage;
- Sector stage;
- Stage of menstrual flow.
In order to correctly assess the cyclic changes of the endometrium, one should take into account the duration of the cycle and its clinical features (presence of dysfunctional uterine discharge, duration of the secretion phase, volume of menstrual bleeding during the month).
Causes of menstruation with clots
To notice the pathology, you need to understand why pieces of the endometrium come out during menstruation. The inner layer of the uterus, the endometrium, is functional. It grows, creating favorable conditions for a fertilized egg. If pregnancy does not occur, menstruation begins. Due to the contraction of the uterus, unnecessary endometrium is rejected along with bloody discharge. Within 3-5 days, the entire exfoliated layer will be completely removed.
Two conditions indicate disturbances in the female body - a complete absence of clots and too large pieces of meat.
In the first case, we can conclude that the endometrium is underdeveloped and there are possible problems with conception. The second is about changes in the functioning of a woman’s reproductive system. Why this happens is difficult to say without a medical examination.
The most common reasons:
- Hormonal imbalance. It is disruptions in the functioning of the endocrine system that most often cause the endometrium to peel off in large pieces. Improper production of hormones can lead to serious complications. Causes imbalance: stress, nervous tension, fatigue. The situation can be corrected by eliminating the irritants; sometimes hormone therapy is required.
- Availability of an IUD. After the installation of an intrauterine device, designed to protect the body from pregnancy, the nature, color and smell of menstruation always changes; during menstruation, clots similar to meat or liver come out. This is due to the fact that the IUD does not always take root; in addition, it causes egg rejection.
- Adhesive processes. They arise due to a violation of the structure of the walls of the uterus. If there are a lot of adhesions, this leads to scanty periods with clots. Often the pathology ends in infertility.
- Endometriosis, endometritis, fibroids, hyperplasia. These pathologies are characterized by changes in the structure of the endometrium. When it comes off and comes out with your period, large pieces form. These pathologies require serious treatment. Their danger lies in the absence of pronounced symptoms for a long time. Menstruation is the only way to suspect irregularities.
Childbirth, termination of pregnancy, abortion can also cause menstruation with clots and pieces of meat.
After an abortion, heavy discharge is normal, but if it lasts longer than 10 days or this symptom is associated with others (fever, pain), you should consult a doctor as an emergency.
Second phase of the menstrual cycle
The second phase of the cycle is responsible for a woman’s reproductive health. It is during this period that a woman can become pregnant. Ovulation is absent in pregnant and lactating women, as well as during adolescence and menopause. Normally, ovulation occurs up to 10 times a year. Two menstrual cycles during this period may be anovulatory. In order for ovulation to occur, a balance of the hormones LH and FSH is necessary. They are produced by the pituitary gland.
It is generally accepted that the presence of menstruation is a guarantee of proper ovulation. Actually this is not true. Your period can come regardless of whether ovulation has occurred or not. Special tests that respond to an increase in LH levels in the urine help confirm its presence. But ultrasound monitoring is considered a more reliable way to determine ovulation. With its help, you can monitor the growth of the egg and catch the exact day of its release into the abdominal cavity. This method is carried out for diagnostic purposes and to increase the chances of conception when planning a pregnancy.
Proliferative diseases
The endometrium grows very actively in the proliferation phase, its cells divide under the influence of various hormones. Potentially, this condition is dangerous due to the development of various kinds of diseases associated with pathological cell division - neoplasms, tissue proliferation, etc. The development of pathologies of this type can be caused by some failures in the process of passing through the stages. At the same time, the secretory endometrium is almost completely not susceptible to such danger.
The most typical disease that develops as a result of a violation of the proliferation phase of the mucous membrane is hyperplasia. This is a condition of pathological growth of the endometrium. The disease is quite serious and requires timely treatment, as it causes severe symptoms (bleeding, pain) and can lead to complete or partial infertility. The percentage of cases of its degeneration into oncology, however, is very low.
Hyperplasia occurs due to disturbances in the hormonal regulation of the division process. As a result, cells divide longer and more actively. The mucous layer thickens significantly.
What is endometrial proliferation?
The endometrium is the inner mucous membrane of the uterus, penetrated by a thin and dense network of blood vessels. It supplies the reproductive organ with blood. The proliferative endometrium is a mucous membrane that is in the process of rapid cell division before the start of a new menstrual cycle.
The structure of the endometrium
The endometrium has two layers. Basal and functional. The basal layer remains virtually unchanged. It promotes the regeneration of the functional surface during the menstrual cycle. It consists of cells that are as adjacent to each other as possible, equipped with a thin but dense vascular network.
The normal thickness of the endometrium is up to one and a half centimeters. Unlike the basal layer, the functional layer is constantly changing. Because during menstruation, labor, surgery, diagnosis, it is damaged.
There are several cyclic stages of the functional endometrium:
- Proliferative
- Menstrual
- Secretory
- Presecretory
The stages are normal, successively replacing each other, according to the period passing in the woman’s body.
What is the normal structure?
The condition of the endometrium in the uterus depends on the phase of the menstrual cycle. When the time of proliferation comes to an end, the main layer reaches 20 mm, and is practically immune to the influence of hormones. When the cycle just begins, the endometrium is smooth and pinkish in color.
With focal areas of the active layer of the endometrium that has not separated, remaining from the last menstruation. Over the next seven days, a gradual thickening of the proliferative endometrial membrane occurs due to active cell division.
There are fewer vessels, they hide behind the grooves that appear due to heterogeneous thickening of the endometrium. The thickest mucous membrane is on the posterior uterine wall, at the bottom. On the contrary, the “baby place” and the anterior uterine wall change minimally. The mucous layer is about 1.2 centimeters.
When the menstrual cycle ends, normally the active covering of the endometrium is completely shed, but as a rule, only part of the layer is shed in some areas.
Forms of deviation from the norm
Violations of the normal thickness of the endometrium occur either due to natural causes or are pathological. For example, in the first seven days after fertilization, the thickness of the endometrial covering changes - the baby's place becomes thicker. In pathology, thickening of the endometrium occurs during abnormal cell division. As a result, an extra mucous layer appears.
What is endometrial proliferation
Proliferation is a phase of rapid cell division in tissues that does not exceed standard values. During this process, the mucous membrane is regenerated and grows. The new cells are not of an atypical type; normal tissue forms on them. Proliferation is a process characteristic not only of the endometrium. Some other tissues also undergo the process of proliferation.
Causes of proliferation
The reason for the appearance of the endometrium is of a proliferative type, due to the active rejection of the active layer of the uterine mucosa. After this, it becomes very thin. And it should be regenerated before the next menstruation. The active layer is renewed during proliferation.
Sometimes, it has pathological causes. For example, the proliferation process occurs with endometrial hyperplasia. (if hyperplasia is not treated, it prevents you from getting pregnant). With hyperplasia, active cell division occurs and the active layer of the uterine mucosa thickens.
Secretion phases
Secretion is also divided into three stages:
- Early - from 15 to 18 days of the cycle.
- The average is 20-23 days of the cycle, at this time secretion is most active.
- Late – from 24 to 27 days, when secretion subsides.
The secretory phase is replaced by the menstrual phase. It is also divided into two periods:
- Desquamation - from day 28 to day 2 of a new cycle, if the egg is not fertilized.
- Recovery - from 3 to 4 days, until the active layer is completely rejected, and until the start of a new proliferation process.
After passing through all stages, the cycle repeats again. This happens before pregnancy, menopause, if there are no pathologies.
How to diagnose
Diagnostics will help determine signs of proliferation of a pathological type. There are several ways to diagnose proliferation:
- Visual inspection.
- Colposcopic examination.
- Cytological analysis.
To avoid serious diseases, it is necessary to regularly visit a gynecologist. The pathology can be seen during a routine gynecological examination. Other methods can more accurately determine the cause of abnormal proliferation.
Diseases associated with proliferation
The endometrium actively grows in the proliferation phase, cell division occurs under hormonal influence. During this period, pathologies may appear due to rapid cell growth. Tumors may appear, tissues will begin to grow, etc.
Diseases can appear if something goes wrong during the cyclic phases of proliferation. In the secretory phase, the development of membrane pathologies is practically excluded.
Most often, during cell division, hyperplasia of the uterine mucosa develops, which in some cases can lead to infertility and cancer of the reproductive organ.
The disease provokes a hormonal imbalance that occurs during the period of active cell division.
As a result, its duration increases, there are more cells, and the mucous membrane becomes much thicker than normal. Treatment of such diseases must be timely.
Most often, medication and physiotherapeutic treatment are used. In serious cases, surgical intervention is resorted to.
Why does the proliferation process slow down?
Inhibition of endometrial proliferation processes or failure of the second stage of the menstrual cycle is distinguished by the fact that cell division stops or occurs much more slowly than usual.
These are the main symptoms of impending menopause, ovarian deactivation and cessation of ovulation. This is a normal phenomenon, typical before menopause. But, if inhibition occurs in a young woman, then this is a sign of hormonal instability.
This pathological phenomenon must be treated; it leads to premature cessation of the menstrual cycle and the inability to become pregnant.
Source: https://MatkaMed.ru/endometrij/endometrij-proliferativnogo-tipa
Endometrium when taking COCs
The use of COCs has become a common occurrence in the life of a modern woman. However, few people know what happens to the body when taking contraceptives and how they prevent conception. To understand this, you need to understand how oral contraceptives work:
- During ovulation, a mature egg moves into the fallopian tube, where fertilization occurs with seminal fluid. Contraceptives suppress the maturation process, so the egg is dormant and ovulation does not occur.
- Taking birth control pills makes the mucus in the cervix too thick, which prevents sperm from entering the uterus. Therefore, even in cases where a woman forgets to take the pill, the risk of becoming pregnant is extremely low, even if ovulation has occurred.
- Poor peristalsis of the fallopian tubes, which is caused by contraceptives, reduces the likelihood of seminal fluid reaching the egg.
- COCs have a direct effect on the endometrium. In a normal state, the fertilized egg enters the uterus and attaches to the endometrium. After menstruation, in the first half of the menstrual cycle, the endometrium is restored. During the second half of the cycle, it actively grows, ensuring the successful attachment of the egg to the walls of the uterus. However, under the influence of contraceptives, the restoration of the mucous layer is inhibited - fertilization becomes impossible, even if it has occurred, the fertilized egg has no opportunity to gain a foothold.
Cycle phases
In a healthy woman, the inner lining of the uterus goes through 3 main phases. The thickness of the endometrium during these phases has its own standard indicators, which can be seen in the photo in the gynecological office.
By observing the process under ultrasound control and establishing that the thickness of the endometrial layer corresponds to the days of the cycle, one can form an opinion about the absence of hormonal disorders and the normal course of cyclic changes in the female body.
- proliferative phase;
- secretory phase;
- directly the bleeding phase, that is, the period of menstruation (desquamation).
During each phase, changes occur in the tissues of the ovaries and endometrium due to fluctuations in hormones. Because of this, the thickness of the endometrial layer varies by day of the cycle. Before the onset of menstruation, the thickening becomes maximum. Typically the entire cycle takes about 27-29 days. During this time, the mucous membrane is modified from minimal thickness to the state of an overgrown, loose structure that is rejected with menstruation.
Proliferation phase
It should begin immediately after the end of menstruation, approximately on the 5th day from the start of menstruation, and last from 12 to 14 days. During this phase, the endometrial layer grows from its minimum thickness of 2-3 millimeters, its preparation for the ovulatory process and possible fertilization begins.
The proliferation phase has 3 stages:
- at the early stage (before the 7th day), the endometrial norm is from 4-5 mm to 7 mm in thickness, the density is reduced (hypoechoic), the layer is relatively uniform, looks pale pink and thin;
- in the middle stage, the mucous membrane continues to thicken and grow, the endometrium 9 mm grows by the 9th day, by the 10th - up to 10 mm, acquires a rich pink tint;
- the final stage (late proliferation) lasts from 10 to 14 days, the endometrial layer acquires a folded structure, characterized by thickening in areas of the fundus and posterior wall of the uterus, on average the endometrium is 13 mm.
Secretion phase
When the secretion phase begins, which starts a couple of days after ovulation, the endometrial layer no longer grows at the same rate. On an ultrasound, you can see that significant changes in the structure have begun under the influence of progesterone, which is produced by the corpus luteum of the ovary.
This phase also consists of 3 stages:
- At the early stage of secretion, the mucous membrane grows slowly, and restructuring begins in it. The thick endometrium swells even more and acquires a yellowish tint. On ultrasound, hyperechogenicity can be noted along the edges of the endometrium, which reaches 14-15 mm;
- in the middle stage of secretion, which lasts from the 24th to the 29th day, the endometrium undergoes pronounced secretory transformations, becomes maximally dense and reaches a maximum thickness of 15-18 mm - this is the norm. The ultrasound picture reveals the appearance of a dividing line between the endometrium and myometrium, which represents a zone of exfoliation;
- the late stage precedes the onset of menstruation. The corpus luteum involutions, the level of progesterone decreases, and the process of trophic changes in the overgrown layer begins. The endometrium has a thickness limit before menstruation - 1.8 cm. On ultrasound, you can see areas of dilated capillaries and the beginning of thrombotic processes, which subsequently lead to necrotic phenomena in the tissues, preparing them for rejection.
Desquamation phase (immediately the period of menstruation)
During menstruation, the functional layer is destroyed and rejected, coming out in the form of menstrual bleeding. This phase lasts, on average, 4-6 days and is divided into 2 stages - rejection and recovery.
- At the stage of rejection (days 1-2 of the cycle), the endometrial layer is normally 5-9 mm, it is hypoechogenic (decreased density), capillaries are deformed, burst, and menstruation begins.
- At the regeneration stage, starting from the 3rd to the 5th day, the endometrium has a minimum thickness of 3 to 5 mm.
What changes in the endometrium occur during the secretion phase?
This phase is also divided into early, middle and late stages. It begins 2-4 days after ovulation. Does this phenomenon affect the thickness of the endometrium? At the early stage of secretion, the endometrium has a thickness of at least 10 and maximum 13 mm. The changes are associated primarily with increased production of progesterone by the corpus luteum of the ovary. The mucous membrane increases even more significantly than in the proliferation phase, by 3-5 mm, becomes swollen, and acquires a yellowish tint. Its structure becomes homogeneous and does not change until the onset of menstruation.
The middle stage lasts from the 18th to the 24th day of the menstrual cycle and is characterized by the most pronounced secretory changes in the mucous membrane. At this point, the normal thickness of the endometrium is a maximum of 15 mm in diameter. The inner layer of the uterus becomes as dense as possible. When performing an ultrasound during this period, you can notice an echo-negative strip at the border of the myometrium and endometrium - the so-called rejection zone. This zone reaches its maximum before menstruation. Visually, the endometrium is swollen and, due to folding, can acquire a polypoid appearance.
What changes occur in the late stage of secretion? Its duration is from 3 to 4 days, it precedes menstrual bleeding, and usually occurs on the 25th day of the monthly cycle. If a woman is not pregnant, then involution of the corpus luteum occurs. Due to the reduced production of progesterone, pronounced trophic disorders occur in the endometrium. When performing an ultrasound during this period, the heterogeneity of the endometrium is clearly visible, with areas of dark spots and areas of vascular disorders. This picture is caused by vascular reactions occurring in the endometrium, leading to thrombosis, hemorrhage, and necrosis of mucosal areas. The rejection zone on ultrasound becomes even more distinct, its thickness is 2-4 mm. On the eve of menstruation, the capillaries in the layers of the endometrium become even more dilated and spirally convoluted.
Their tortuosity becomes so pronounced that it leads to thrombosis and subsequent necrosis of mucosal areas. These changes are called "anatomical" menstruation. Immediately before menstruation, the thickness of the endometrium reaches 18 mm.
What happens during the desquamation phase?
During this period, the functional layer of the endometrium is rejected. This process begins on the 28-29th day of the menstrual cycle. The duration of this period is 5-6 days. There may be deviations from the norm for one or two days. The functional layer looks like areas of necrotic tissue; during menstruation, the endometrium is completely rejected in 1-2 days.
With various diseases of the uterus, delayed rejection of areas of the mucous membrane can be observed, this affects the intensity of menstruation and its duration. Sometimes during menstruation there is very heavy bleeding.
If the bleeding intensifies, you should consult a gynecologist. This should be especially remembered during the first menstruation after a miscarriage, as this may mean that particles of the fertilized egg remain in the uterus.
Additional information about menstruation is provided in the video:
Does menstruation always start on time?
Sometimes there are situations when the onset of menstruation occurs untimely. If pregnancy is excluded, then this phenomenon is called delayed menstruation. The main reason causing this condition is hormonal imbalance in the body. Some experts consider the norm to be delayed for a healthy woman up to 2 times a year. They can be quite common for teenage girls who have not yet established their menstrual cycle.
Factors that may lead to this condition:
- Chronic stress. It can provoke disruption of the production of pituitary hormones.
- Excess body weight or, conversely, sudden weight loss. Women who suddenly lose weight may experience a loss of menstruation.
- Insufficient intake of vitamins and nutrients from food. This can happen when you are addicted to weight loss diets.
- Significant physical activity. They can lead to a decrease in the production of sex hormones.
- Gynecological diseases. Inflammatory diseases in the ovaries lead to disruption of hormone production.
- Diseases of the endocrine organs. For example, menstrual irregularities often occur with thyroid pathology.
- Operations on the uterus. Often a delay in menstruation occurs after an abortion.
- After spontaneous abortion. In some cases, curettage of the uterine cavity is additionally performed. After a miscarriage, the endometrium does not have time to recover, and the onset of menstruation occurs later.
- Taking hormonal contraceptives. After their cancellation, menstruation may occur later than 28 days.
The average delay is most often up to 7 days. If your period is delayed by more than 14 days, you must be tested again to determine if you are pregnant.
If there are no periods for a long time, 6 months or more, they talk about amenorrhea. This phenomenon occurs in women during menopause, rarely after an abortion, when the basal layer of the endometrium was damaged. In any case, if the normal menstrual cycle is disrupted, you should consult a gynecologist. This will allow timely detection of the disease and begin its treatment.
What happens to menstruation after treatment?
How quickly menstruation recovers and what it looks like after treatment for endometritis largely depends on the method and quality of therapy, the woman’s age and the form of the disease.
After curettage, a bloody smear is noticed for 3-10 days. Heavy discharge requires urgent help, as in this case there is a risk of complications. Their absence will make specialists suspect a narrowing of the cervical canal, which also needs to be treated.
Menstruation with endometritis is far from the only sign of the disease. But the changes happening to them dictate the need for examination. Endometritis, if allowed to develop, can negatively affect not only the well-being, but also the reproductive capabilities of a woman. And in order not to give him a chance, you should beware of casual relationships, choose contraceptives together with a doctor and be regularly examined.
Before using any medications, you should consult a specialist doctor. There are contraindications.
Changes are observed in the female body every month, the cause of which is cyclical fluctuations in hormones. Menstrual bleeding is considered one of these manifestations. However, this is only a visible component of a complex mechanism aimed at procreation and the ability to conceive a child.
It is extremely important that the endometrium, the lining of the uterus, is of normal thickness throughout the entire menstrual period; only in this case can a woman have a healthy pregnancy. In this case, it is very important to know what thickness of the endometrium is considered normal before the onset of menstruation?
Kinds
Depending on what causes the pathology, it can occur as two completely different processes (which, in fact, are the two types of reverse development of the endometrium). Depending on what kind of impact or failure caused the pathology, fundamentally different treatments are prescribed. It is quite effective in both cases, and if eliminated in a timely manner, it does not in any way interfere with the occurrence of future pregnancies.
Pathology of the corpus luteum
A fairly common type of pathology. With reverse development in pathology of the corpus luteum, it occurs as a result of hormonal imbalance. This phenomenon is said to occur when persistence of the corpus luteum is observed. In this case, progesterone, which is produced by the corpus luteum, is formed in smaller quantities than it should. The pathological condition develops with sufficiently long-term exposure to such low concentrations.
How can a patient notice such a condition? A certain clinical picture is formed. The time of menstrual bleeding is prolonged, which is due to the fact that the secretory (renewing) endometrium is rejected and renewed more slowly. At the same time, most of it is subject to reverse development.
The reasons for this phenomenon almost always lie in the gradual decline of the function of one or both ovaries. Therefore, this condition is most typical for women of premenopausal age, as well as in menopause. However, sometimes it develops in women of reproductive age, which may be associated with endocrine diseases, cancer and inflammatory processes in the ovaries, as well as for other reasons.
Dynamics of changes
Disturbed pregnancy
This condition has other causes and manifestations if it develops during a disturbed pregnancy. Moreover, this does not happen immediately; often a disrupted pregnancy is present in an undiagnosed patient for quite a long time (several weeks) before it begins to cause reverse development of the endometrium. Often it is diagnosed just when visiting a doctor due to symptoms of reverse development. In what cases can we talk about such a pregnancy?
- Incomplete spontaneous abortion;
- Incomplete removal of the fertilized egg during mechanical or medical abortion;
- Death of the embryo in a very early stage of pregnancy.
Moreover, with an equal degree of probability, the condition can develop both during uterine and ectopic disturbed pregnancy. The process of development of pathology in this case is as follows: first, the structure of the endometrium changes, it ceases to be decidual. And after this, the mucous membrane goes into a dormant state and is not renewed. Then the proliferation phase begins.
Strictly speaking, this condition is diagnosed by scraping from the uterine cavity, in the case when the tissue of the dead fertilized egg has already begun to decompose.
Interpretation of endometrial biopsy results
On average, deciphering the results of an endometrial biopsy takes 1-2 weeks.
This depends on the operating mode of the pathology laboratory and the complexity of the stains used. The method of taking a biopsy of the uterine mucosa also plays a significant role - in some cases, the morphologist receives whole fragments of tissue with a preserved histological structure, while in others there is a high probability of receiving only blood clots.
Biopsy techniques
Most often, an endometrial biopsy is taken by traditional diagnostic curettage (CDC).
The resulting material consists of separate sections of the mucous membrane, in which the uterine glands, connective tissue stroma and their relationships with each other are clearly visible.
If the sample contains malignant elements, the pathologist can accurately determine the depth of their germination, and this directly affects the treatment tactics and prognosis of the disease.
Unlike RDV, during
endometrial aspiration and pipel biopsy, the doctor does not receive complete layers of the mucosa, but its scattered elements with a large admixture of blood.
Often the biomaterial is represented by nothing more than a meager accumulation of individual cells, from which it is impossible to reliably judge the nature of the pathological process. From the point of view of the diagnostic value of the results of endometrial biopsy, preference should be given to separate diagnostic curettage.
However, in some cases, a comprehensive interpretation of biopsy specimens is not required. Thus, a pipel biopsy is usually performed to assess the condition of the endometrium before the IVF procedure.
In this situation, even scattered elements of the mucosa are enough to determine the type of pathology.
In his conclusion, the pathologist can give a different interpretation of the endometrial biopsy, with or without a detailed description of the morphology. Often the results are accompanied by a pathological diagnosis, which is a brief summary of the descriptive characteristics.
Below is an explanation of the various terms that can be found in the results of an endometrial biopsy.
- Adenocarcinoma is a synonym for uterine cancer.
- Adenomyosis is the growth of the uterine glands in the myometrium (the muscular lining of the uterus). A rare find, mainly in RDV.
- Atrophic mucosa - thinned endometrium with single glands. Quite normal during menopause; at a younger age indicates serious hormonal imbalances.
- Chorionic villi are auxiliary components of the fertilized egg, thanks to which it attaches to the uterine mucosa. Subsequently, they transform into the placenta. The presence of chorionic villi in endometrial scraping is an unambiguous sign of pregnancy.
- Hyalinosis is a thickening and narrowing of the lumen of small uterine arteries.
- Atypical hyperplasia is the proliferation of endometrial glands with signs of malignant transformation. Potentially precancerous condition.
- Simple hyperplasia is the same thing, but without signs of a tumor. Occurs with hormonal disorders due to ovarian cysts and other conditions.
- Hypoplastic mucosa is a thinned endometrium, occupying an intermediate state between mature and atrophic.
- Gravidar mucosa is the endometrium of the pregnant uterus with fields of decidual tissue.
- Detritus is a designation for amorphous masses represented by the remains of dead cells.
- Decidual tissue is a collection of large cells containing an abundance of nutrients. Sign of pregnancy.
- Dysplasia is a change in the structure and cellular composition of the uterine glands, reminiscent of tumor transformation.
- A cyst is an enlarged gland filled with fluid.
- Leiomyoma is a benign tumor of smooth muscle located in the middle lining of the uterus.
- Lymphoid follicles are accumulations of lymphocytes that reflect a long-term inflammatory process (for example, chronic endometritis).
- Menstrual mucosa - endometrium at the height of menstruation.
- Metaplasia is a condition in which the normal epithelium of the uterine mucosa is replaced by epithelium characteristic of another organ.
- Placental polyp - remnants of the placenta after a miscarriage, abortion or natural birth (less often after a cesarean section).
- A polyp is any formation of the mucous membrane protruding into the lumen of the uterus.
- Hydatidiform mole is a pathology of pregnancy, a variant of trophoblastic disease. Characterized by the growth of chorionic villi alone; the fetus is not formed.
- The Arias-Stella reaction is a variant of changes in the endometrium, reminiscent of the transformation of the glands of the cervical canal during pregnancy. Indicates a hyperplastic process.
- Regenerating mucosa - endometrium in the first 1-3 days after menstruation.
- Spiral arteries are small blood vessels that penetrate the lining of the uterus. The main source of its blood supply.
- Stroma is the tissue in which the endometrial glands are embedded.
- Trophoblast is the cellular material from which chorionic villi and other auxiliary structures of the embryo are formed.
- The proliferation phase corresponds to days 5-14 of the menstrual cycle (after menstruation).
- The secretion phase corresponds to days 15-26 of the menstrual cycle (before menstruation).
- Fibrosis is the proliferation of dense connective tissue in the stroma. A sign of chronic inflammation, and also a normal phenomenon in postmenopause.
- Choriocarcinoma is a malignant tumor of atypical chorionic villi, a variant of trophoblastic disease. To put it roughly, choriocarcinoma is a “cancerous hydatidiform mole.”
- Endometritis is an inflammation of the uterine mucosa.
Following actions
Further tactics depend on the method used to take the biopsy. If the results of an aspiration or pipel biopsy reveal hyperplasia and signs of atypia, then this in most cases serves as an indication for separate diagnostic curettage.
If, in addition to indicating the phase of the cycle and the presence of blood or detritus, nothing else is indicated in the conclusion, then in fact this indicates the absence of any pathology on the part of the endometrium.
Subsequent actions by the patient and the gynecologist should be aimed at excluding other causes of dysfunctional uterine bleeding.
The presence of tumor changes, including atypical hyperplasia, requires regular follow-up and consultation with a gynecological oncologist. The stage of the cancer process is determined and complex treatment is prescribed, including surgery, chemotherapy and radiation therapy.
Treatment in Israel
Israeli gynecologists have significant experience in treating various diseases of the uterus. Using modern technologies, doctors at the Top Ichilov Clinic accurately determine the likelihood of malignant degeneration of tumors and carry out their excision using minimally invasive methods.
To find out more detailed information regarding your case, fill out the form below.
For non-surgical treatment, Top Ichilov uses the latest drugs, the effectiveness of which exceeds 90%, and advanced techniques: brachytherapy, photodynamic therapy, radiotherapy using the TrueBeam and many others.
If there is no choice left and it is necessary to
surgically remove a tumor or even the uterus, Top Ichilov often uses a Da Vinci .
This operation completely eliminates the possibility of medical error and prevents complications. Source: https://ProBiopsii.ru/rasshifrovka-rezultatov-biopsii-jendometrija/
Treatment
If the condition is diagnosed after childbirth, it is not treated. It should go away on its own as soon as the woman’s hormonal levels return to normal. If at this stage she is worried about severe bleeding, then drugs that stop them can be prescribed - Oxytocin, Vikasol, etc. However, if this endometrial condition does not go away for a long time, then hormonal treatment can be prescribed, but it is strictly individual , and is based on what type of malfunction persisted in the woman after pregnancy.
They act in a similar way for changes resulting from a disturbed pregnancy.
It is important to quickly remove the fertilized egg and embryo if it remains in the uterus. Then its hormonal activity will completely disappear and the body will return to normal quickly (even faster than after childbirth).
Treatment is also carried out individually only if the hormonal imbalance persists. The same drugs are prescribed to stop bleeding.
If the process is not associated with pregnancy, but is associated with low concentrations of progesterone in the body, then it is treated accordingly. Progesterone drugs are prescribed in individual dosages. These are such products as Norkolut, Utrozhestan, Duphaston. They are taken for a period of about 3 months, and if necessary, longer.
Probability of conception with deviations
When the endometrium after ovulation does not correspond to the norm, women immediately panic, which doctors consider not a very reasonable decision, since conception is still possible. There is a high probability of successful IVF, part of which will be the creation of a normal size of the uterine lining.
Although exceptions also occur - in certain cases, patients become pregnant and carry a healthy child naturally, but there are very few such situations in modern times.
If the egg is not fertilized, changes in the corpus luteum will be very rapid, which will reduce the production of progesterone. As hormone levels drop, new follicles mature in the second ovary.
Each month during reproduction, the ovaries alternate. The level of estrogen and uterine mucus rises to a hormonal situation that responds to menstrual bleeding, and the ovulation cycle begins again.
Thick endometrium
If the endometrium reaches a thick size during ovulation, there is still a chance of pregnancy. But in this case, hyperplasia is diagnosed, which, as is known, leads to infertility. If the fertilized egg fails to attach to the lining of the uterus, a miscarriage is likely to occur. This is due to a significant increase in the tone of the uterus and the rapid renewal of thickened tissues, and therefore the embryo is often rejected.
Thin endometrium
There are also cases when the mucous layer is too thin and does not exceed 4 mm in width. Then conception is unlikely, since the embryo simply will not be able to gain a foothold there.
Due to the thin layer, the fertilized egg will not receive the required volume of blood, and therefore, nutrients and oxygen. As a result, the embryo will not develop and the pregnancy will “freeze” and the fetus will be rejected.
Discussion
A. Simon, N. Laufer [4] are unanimous in the opinion that the thickness and structure of the endometrium, as well as its adequate vascularization, are useful prognostic signs that determine the effectiveness of PE in IVF cycles. However, data on the minimum acceptable thickness of the endometrium for successful pregnancy varies. If the endometrial thickness is less than 7 mm, pregnancy after PE does not occur in the vast majority of patients, however, other studies indicate a minimum endometrial thickness of 6 mm. In addition, some studies report the occurrence of pregnancy with an endometrial thickness of 4 mm. According to the results of a study by N. Singh et al. [11], endometrial thickness of more than 14 mm is associated with a high risk of pregnancy loss.
In our study, the maximum pregnancy rate during PE was observed with an endometrial thickness of 8-11 mm. When the endometrial thickness was less than 6 mm, pregnancy occurred in only one case.
D. Sardana et al. [6] showed that measurement of intraendometrial blood flow plays a primary role in indirectly assessing endometrial receptivity and can determine the prognosis of implantation. Endometrial perfusion assessment is a study that has prognostic value for determining the likelihood of implantation in IVF cycles.
The results of our study showed that there is a strong positive relationship ( r
=+0.73) between the presence of adequate endometrial peristalsis and its vascularization. Thus, in the presence of intraendometrial blood flow, peristalsis was observed in the vast majority of cases (73.7%), while in its absence, adequate endometrial peristalsis was recorded only in 20.6% of patients.
M. Ijland et al. [9] at the end of the twentieth century proved that the peristaltic activity of the endometrium is directly related to the likelihood of fertilization in a spontaneous cycle. Continuing work in this direction, the researchers also noted that in cycles of controlled induction of superovulation, endometrial peristalsis was more pronounced.
In our study, we found that in the presence of adequate peristalsis and perfusion of the endometrium, the pregnancy rate in PE was significantly high and amounted to 63.1% versus 39.7% in the group where adequate peristalsis and endometrial vascularization were not registered.