CYTOLOGY smear is a method of microscopic examination of the cervical epithelium for the purpose of PREVENTION AND EARLY DIAGNOSIS OF CERVICAL CANCER.
A cytology smear primarily performed to detect atypical cells , which allows early diagnosis of dysplasia (CIN, LSIL, HSIL) or cervical cancer. It is an inexpensive and convenient method for reaching large numbers of women with preventative care. Of course, the sensitivity of a single study is low, but annual mass screening in developed countries has significantly reduced the mortality rate of women from cervical cancer.
Due to the fact that atypical cells can be located in a relatively small area of the mucosa, it is very important that the material is obtained from the entire surface of the cervix, especially from the cervical canal ! For this purpose, special brushes have been created that make it possible to obtain material from areas inaccessible to inspection.
Particular attention is paid to the transformation zone, the cells of which most often undergo tumor degeneration. It is in the transformation zone that up to 80-90% of cervical cancer develops, the remaining 10-20% occur in the cervical canal.
When to take a smear for cytology? A smear for cytology should be taken starting from the 5th day of the menstrual cycle and 5 days before the expected start of menstruation. The analysis cannot be carried out within two days after sexual intercourse or insertion of suppositories into the vagina. Failure to follow these rules may lead to erroneous interpretation of the results. Also, the presence of a pronounced inflammatory process in the cervix and vagina seriously complicates diagnosis.
It should be noted that collecting material is a rather unpleasant procedure. The gynecologist must scrape the epithelium from the surface of the cervix and enter the cervical canal. The more epithelium from different zones gets in, the better the diagnosis. Sometimes bruising may remain after cytology, this is considered normal.
Thus, the main significance of a cytology smear is to determine qualitative changes in cells. To determine the infectious agent that caused the inflammation, it is better to use a smear on the flora or bacteriological culture . However, during a cytological examination, the doctor may note the presence of any microorganisms. Normal microflora includes rods (lactobacillus), single cocci, and in small quantities there may be opportunistic flora. The presence of specific infectious agents (Trichomonas, amoebas, fungi, gonococci, gardnerella, leptothrix, chlamydia, an abundance of cocci) is considered a pathology that needs to be treated.
Processing of smears. Cytology deadlines
After collecting the material, the sample is transferred to a glass slide, fixed and stained. When directly transferring a smear from a brush, partial loss of material and cell deformation are possible, which leads to a decrease in the sensitivity of the method and a large number of false results. The classical method was replaced by liquid cytology, which significantly increased the accuracy and quality of the study.
Liquid cytology is a new technology for processing smears, which involves placing samples in a container with a special stabilizing solution. In this case, the entire resulting epithelium enters the solution, which is then centrifuged and cleared of unwanted impurities (mucus, etc.). Today, liquid-based cytology is becoming the “gold standard” for examining smears from the cervical mucosa. But even in this case, the sensitivity of a single study does not exceed 60-70%. During reproductive age, false negative results are common, and in menopausal women, false positive results are common. Only triple cytological examination allows one to approach 100%.
There are various methods for staining preparations: according to Papanicolau (Pap test), according to Romanovsky, according to Wright-Diemsa, according to Gram. All methods are aimed at staining certain cellular structures, which makes it possible to differentiate different types of epithelium and distinguish between cells with keratinization and tumor transformation. The Pap test is widely accepted and is now used as the main standardized test.
How long does the test take? Depending on the organization of the process, the result can be obtained within 2-3 days.
Cytogram without features - what does this mean?
Cytological findings vary widely. As a variant of the norm, the following conclusions can be used: “ cytogram without features ”, “ cytogram within normal limits ”, “ cytogram without intraepithelial lesions ”, “ cytogram corresponds to age - atrophic type of smear ”, “ NILM - Negative for intraepithelial lesion or malignancy”, " proliferative type of smear ." All this is NORMAL!
The cervical mucosa is normally smooth, shiny, and moist. The squamous epithelium is pale pink, the glandular epithelium is bright red. The cellular composition that can be found in normal cytology is presented in the table.
| Cytogram without features (NILM) in women of reproductive age | |
| Exocervix | Well-preserved cells of squamous epithelium, mainly of the superficial, intermediate layers. |
| Endocervix | Cells of glandular (cylindrical) epithelium. |
| Transformation zone | Squamous epithelial cells, single cells or small clusters of metaplastic squamous epithelium, small clusters of glandular epithelium. |
Atrophic type of smear - what does it mean?
In women in perimenopause and menopause, due to a decrease in the overall level of estrogen, many metabolic processes slow down, which results in atrophy of the squamous epithelium. These changes can be seen in the cytogram. The atrophic type of smear refers to a variant of the normal cytogram. You can often find in the conclusion the phrase “ cytogram corresponds to age ” or “ age-related changes nilm ”. All these are variants of the norm!
You need to understand that in menopausal women, false-positive cytogram results are very common - this is the case when it is difficult for a cytologist to distinguish atrophic squamous epithelium from dysplasia. This needs to be understood because subsequent cervical biopsies usually do not find any pathology. In addition, older women may have a tendency to keratinize the epithelium with the formation of hyperkeratosis (leukoplakia).
| Cytogram without features (NILM) in women in peri-menopause ( atrophic type of smear ) | |
| Exocervix | Well-preserved squamous epithelial cells, mainly of the parabasal and basal layers. More often there are smears of the atrophic type, but they can also be of proliferative or mixed types. |
| Endocervix | The absence of columnar (glandular) epithelial cells is not an indicator of poor quality of the smear, since during this period the transformation zone moves deep into the canal and to obtain glandular epithelium the brush must be inserted to a depth of more than 2-2.5 cm. |
| Transformation zone | Cells of squamous, metaplastic epithelium. |
The mucous membrane of the cervix in menopause is thinned, easily injured and damaged, which is a consequence of a decrease in estrogen.
Decoding the cytogram
Terminology
Dyskaryosis and dyskaryocytes are abnormal cells with hyperchromatic (dense and dark) nuclei and irregular nuclear chromatin. Dyskaryosis will be followed by the development of a malignant neoplasm. Used as a synonym for dysplasia, but as a more general term.
Atypia is any difference in cell structure from the norm. The meaning often depends on the context. But more often it is used to describe pre-tumor and tumor changes.
Inflammatory atypia is a combination of degenerative, reactive, proliferative changes in cells during inflammation. These changes can cause a false-positive diagnosis of dysplasia or cancer.
Dysplasia is a process of impaired maturation of squamous epithelium. It is a true pre-tumor process. Has 3 degrees. The first usually includes a viral lesion, the second and third - a lesion with tumor potential.
ASCUS are atypical cells that are difficult to differentiate from reactive atypia and the pretumor process itself. Atypia of unknown significance.
Dyskeratosis is a disorder of keratinization of individual squamous epithelial cells. Is a sign of HPV.
Parakeratosis is a disorder of keratinization of the epithelial layer. Surface squamous epithelial cells always have some degree of keratinization - this is a protective mechanism. Parakeratosis can be observed normally, with irritation of the mucous membrane for any reason, or with HPV infection.
Koilocytosis (koilocytic atypia, koilocyte) is a specific nuclear change characteristic of the human papillomavirus.
Hyperkeratosis (leukoplakia) is pronounced keratinization of the epithelial layer with the appearance of a protective structureless layer of keratohyalin. This is a normal process for the skin, but in the mucous membranes it is considered a pathology. It is observed with HPV infection, as well as with irritation of the mucous membrane, especially with prolapse of the pelvic organs and uterine prolapse.
Squamous metaplasia is a protective mechanism, a physiological process of replacing delicate glandular epithelium with more stable squamous epithelium. Metaplastic epithelium often becomes a source of dysplasia and cancer, as it is easily affected by the human papillomavirus.
Glandular hyperplasia - proliferation, active growth of glandular epithelium. It is a reactive process during inflammation and erosion of the cervix. Often occurs when using hormonal drugs.
Source: gynpath.ru
Signs of atypia
Atypia is a number of factors that distinguish a normal cell from a cancer cell. Atypia is mainly divided into two types: functional and structural.
- Functional atypia is characterized by a peculiar metabolism that is practically independent of oxygen, unlike normal tissues. Proliferation of atypia will occur even in the absence of oxygen. In the case of general oxygen starvation of the body, the condition of the cancerous tumor will not change. This is due to the fact that the tumor is initially configured to develop in conditions of oxygen deficiency.
- Structural atypia is a violation of the individual development of a cell at all levels. Severe structural atypia can vary even within the same tumor. In turn, structural atypia can be cellular and tissue.
Definition
Simple glandular hyperplasia of the endometrium is a condition of pathological proliferation of glandular tissue. However, not only endometrial glandular tissue can grow, but any other tissue as well. At the same time, the thickness of the endometrium and the total volume of this tissue increase.
Difference from complex
Simple hyperplasia is called when only one type of cell grows (glandular, connective, etc.). If several types of cells undergo proliferation, then we can talk about complex hyperplasia.
Cell atypia: what is it?
It is not entirely correct to call cells with signs of atypia “oncological”. Their presence indicates a pathological process in the body, which can develop into a malignant disease.
When diagnosing the disease, epithelial cells without atypia can be detected. A study result without atypia means that the cells have not yet undergone structural changes and have not lost their function. However, epithelium without signs of atypia may begin to transform after some time, which indicates an unfavorable course of the disease or incorrectly selected therapy.
Tumor cells are characterized by a large number of immature elements. Oncological atypia is manifested by an increase in the number of multinucleated cells, which is one of the diagnostic criteria for tissue biopsy.
The presence of atypical cells is considered a precancerous condition, which requires careful monitoring over time and the appointment of adequate therapy.
The presence of atypia is especially dangerous in the gynecology of women of reproductive age, since in some complex cases radical surgery is required to prevent cancer.
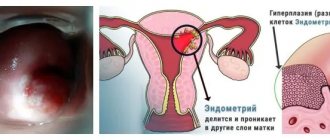
Endometrial hyperplasia
Endometrial hyperplasia is a disorder of the structure of the inner layer of the uterus (endometrium), which can potentially lead to endometrial cancer. Endometrial hyperplasia is characterized by increased growth and thickening of the uterine lining. With endometrial hyperplasia, the relationship between the glandular and stromal tissue of the endometrium is disrupted, and atypia of cell nuclei is detected. Endometrial hyperplasia with and without atypia occurs due to hormonal imbalance with an increase in the production of estrogen and inhibition of progesterone. Women in the transition period are more susceptible to this disease: puberty and menopause. Hyperplasia can also be the result of abortions, diagnostic curettages and gynecological operations. The disease can be caused by inflammatory processes and various neoplasms (for example, a polyp without atypia). Symptoms of endometrial hyperplasia without atypia and with atypia are manifested by menstrual irregularities with the appearance of pathological bleeding, the appearance of bleeding in the middle of the cycle, frequent anovulatory cycles, which provokes infertility. Hormonal imbalance affects the entire body and can cause breast atypia.
Hyperplasia has the following classification:
- Simple glandular hyperplasia without atypia. Simple hyperplasia without atypia is characterized by the proliferation of the inner mucous membrane of the tissue in the uterus. In this case, hyperplasia without atypia is caused by an increase in the number of glandular cells due to a pathological process. There is a proliferation of internal glands and thickening of all endometrial tissues. During normal operation of the endometrial glands, they look like vertical stripes. Glandular simple endometrial hyperplasia without atypia and with atypia leads to a change in the appearance of the glands: they begin to wriggle and layer on top of each other. Simple endometrial hyperplasia without atypia develops without pathological changes in its structure. Gland cells can become of different sizes and have different locations. With endometrial hyperplasia without atypia, the boundary between the basal and functional layers of the endometrium is erased, while the boundaries between the endometrium and myometrium are preserved.
- Complex hyperplasia with atypia. Glandular hyperplasia with atypia is characterized by the presence of signs of cellular atypia. Atypical endometrial hyperplasia is manifested by the appearance of adenomatosis: changes in cell structures, reduction of stromal elements, nuclear polymorphism. The formation of adenomatosis means the appearance of an area of altered mucous membrane in the uterus, the cells of which have disturbances in the structure and functionality of varying degrees of atypia. Endometrial hyperplasia with atypia is a precancerous condition, since the altered cells can soon degenerate into other forms.
Treatment of endometrial hyperplasia without atypia is carried out medicinally using drugs to restore hormonal levels. In the presence of atypia, treatment is combined, including conservative therapy and surgical intervention.
Development factors
Doctors include risk factors that can provoke abnormal growth of tissues of the reproductive organ:
- smoking;
- age. Patients over 35 years of age are more likely to suffer;
- oncology of the ovary, intestines, uterus, diagnosed in one of the family members;
- early menstruation, late cessation;
- absence of pregnancy.
Not only neurohumoral changes take part in the development of the pathology under consideration. Injury to the endometrium can cause the appearance of atypical endometrial hyperplasia for the following reasons:
Doctors associate the appearance of the disease in question with several risk factors. They must be detected promptly at every gynecological examination. Atypical endometrial hyperplasia occurs when there is an imbalance in hormones (gestagens decrease, estrogen levels increase). The reasons for this phenomenon are considered:
- tumor of the ovaries responsible for the production of hormones;
- follicular atresia. This condition provokes a lack of ovulation;
- hyperactivity of the adrenal cortex (Cushing's disease);
- disruptions caused by hormone treatment. Tamoxifen has a particularly negative effect;
- increased activity of the pituitary gland due to the production of gonadotropic hormone.
Doctors often detect adenomatous hyperplasia against the background of certain hormonal imbalances:
- hypertension;
- obesity;
- thyroid diseases;
- diabetes;
- liver damage accompanied by slow utilization of estrogen (cirrhosis, hepatitis).
Atypia of cervical epithelial cells
Cervical ectopia is the location of the cylindrical epithelium that lines the cervical canal on its outer (vaginal) side, where squamous epithelial cells predominate. Outwardly, it looks like a red spot (erosion). Over time, ectopic columnar epithelial cells are again replaced by squamous epithelium. This happens with the help of reserve cells. However, under the influence of any external factors, atypia of squamous epithelial cells or atypia of squamous epithelial cells of unknown significance may occur, which can cause cervical cancer. Epithelium with signs of atypia does not mean the onset of an oncological process, but any cataclysm can cause it.
Diagnostics
Endometrial hyperplasia without or with atypia can be diagnosed using several types of data. An important role is played by the medical history, which takes into account concomitant diseases, methods of contraception, and lifestyle. An ultrasound is also performed to determine the thickness of the endometrium.
Hyperplasia on ultrasound
Based on these data, the issue of the need for diagnostic curettage is decided, since this is a traumatic and complex procedure. But only with the help of a histological examination of the scraping can one determine whether there are atypical cells in the endometrium.
Where to go?
Simple typical hyperplasia is treated by a general gynecologist in most cases. If there is a threat of its transition to an oncological process and the presence of atypical cells, treatment should be carried out by a gynecologist-oncologist. If surgical intervention is necessary, the disease is treated by a gynecologist surgeon together with a gynecologist.
Smear for atypia: what is it?
To identify cells with signs of atypia in a smear of the cervical canal, an atypia cytogram according to Papanicolaou or PAP (Papanicolaou) is used. This type of cytological examination is used to diagnose cervical cancer all over the world; its effectiveness has long been proven.
A test for atypia is carried out as a routine gynecological examination using vaginal speculum. The material (smear) is collected from the area at the border of the columnar epithelium and stratified epithelium. Next, the contents are transferred to a glass slide using special brushes. For more accurate sampling of the material, a special spatula is used, one end of which (narrow and long) enters the external pharynx, and the wide and short end is lowered onto the cervix.
The biological material is sent to the laboratory to identify signs of atypia in the smear. The contents are stained with special dyes, after which it will be possible to easily determine cytoplasmic and nuclear atypia in the smear. First, the type of pathological process is determined: inflammation, reactive or malignant. Then - the composition and severity of atypia; differentiate between squamous and columnar epithelial cells without atypia.
A smear without atypia is considered normal and does not require additional treatment unless other symptoms indicate this.
When performing a Papanicolaou test, precancerous cytological atypia (if present) is detected in 80% of cases. All women over 22 years of age are recommended to undergo annual examination for early detection of atypical changes.
Causes
One of the reasons for the appearance of abnormal epithelial cells is cervical dysplasia. In this case, the cervical cells grow abnormally and they either have an odd shape or grow in huge numbers.
Cell growth is not clearly a cancerous symptom, but over time, the abnormal cell can develop into cancer within about 10 years or a little longer. Cervical dysplasia is more common in women between 25 and 35 years of age and usually has no symptoms.
Unusual cells due to infections such as herpes and human papillomavirus are sometimes reported. HPV is one of the leading risk factors for the development of cervical cancer.
The presence of parasites or fungal infections can also give a positive result. Cellular tissue may appear abnormal due to injury. If infection or injury is suspected, there is usually no problem diagnosing cancer as a result of detecting such an abnormality of epithelial cells.
Pap test evaluation methods
Classes (developed by D. Papanicolaou in 1954):
- 1 class. There are no cells with signs of atypia.
- 2nd grade. Morphological changes in cellular elements under the influence of inflammatory processes in the vagina. Stratified squamous epithelium without atypia. Columnar epithelium without atypia. Inflammatory atypia is possible.
- 3rd grade. The presence of single cells with abnormalities in the nucleus and cytoplasm. Most squamous epithelial cells show no signs of atypia. To clarify the diagnosis, it is necessary to conduct a repeat cytological examination or biopsy.
- 4th grade. Signs of epithelial cell atypia. An increase in the size and number of nuclei, chromatic aberrations, and abnormal cytoplasm are detected.
- 5th grade. Pronounced atypia. Invasive cancer.
Bethesda system classification:
- Benign changes. Cervical epithelium without atypia: columnar epithelium without signs of atypia, squamous epithelium without signs of atypia. Fungi of the genus Candida, herpes virus, and cocci may be present. There may be inflammation.
- Atypia of squamous epithelium. Atypia of unknown significance of squamous epithelial cells (ASC-US atypia). US atypia cells not excluding HSIL. Precancerous condition.
- Squamous cell carcinoma. Invasive cancer: stage and severity are clarified after biopsy and surgery.
Cells without atypia: what are they?
Cells without atypia retain their structure and functionality. Columnar epithelium without atypia and squamous epithelium without atypia continue to perform their functions without changes.
The result of a cytogram without atypia does not always indicate the absence of any disease that reduces the patient’s quality of life. Indeed, the presence of columnar cells without signs of atypia, squamous epithelial cells without atypia, and normal mucus are a good result. However, any gynecological diseases should not be left unattended. If atypia is not detected today, this does not mean that after some time cells without signs of atypia will not degenerate into precancerous ones.
The rather complex process of diagnosing infections of the genital organs and genitourinary system most often does not allow the doctor to quickly and promptly prescribe the necessary treatment.
This is especially true for oncological diseases that are asymptomatic. Therefore, women of reproductive age are recommended to take a cytology test at least once a year.
Cytological smear: what is it?
The cytological smear also has other names, such as Pap test, cytology smear, Pap smear. This type of study is carried out during a gynecological examination, as a result of which the doctor suspects an anomaly. To carry out the test, it is necessary to collect cells with a special instrument, a brush, from the walls of the vagina, from the cervical canal, and also from the cervix.
The procedure is carried out without special preparation and is painless for the patient. The resulting mucus is applied to a glass slide, dried and sent for examination. During the analysis, the drug is stained with special reagents and examined under a microscope. This determines:
- structures and sizes of cells;
- epithelial shape;
- number of cells per unit area;
- pathologies in cell structure;
- arrangement of cells relative to others.
A cytology smear allows you to determine the presence of inflammation of the genitourinary system , the development of tumors and the likelihood of developing precancerous epithelial pathologies. Squamous epithelium is a layer of cells lining the vaginal mucosa.
HSIL – high grade intraepithelial changes, suspicious for ingrowth into underlying tissues
When HSIL is detected in a cytological study, cervical neoplasia (CIN) is detected in almost all patients, and invasive cancer is detected in 2% of subjects. Therefore, HSIL provides only one option - colposcopy followed by a biopsy to obtain a sample of the endocervix. Other methods are completely inapplicable, since wait-and-see tactics can lead to disastrous results.
If a woman is planning a pregnancy and has HSIL, a biopsy is indicated. The result of the study of the obtained material determines the future fate of the patient.
If severe dysplasia is confirmed by colposcopy during menopause, loop excision of the cervix (excision of the affected layers while preserving unaffected tissue, PEE) is recommended for diagnostic purposes. The excised tissues are sent for histology. In addition, excision (conization) is recommended in any case of detection of HSIL when the colposcopy result is considered unsatisfactory or negative.
Detection of HSIL during pregnancy requires a colposcopic examination. If the result of colposcopy is unsatisfactory (the transformation zone is not visible), then re-diagnosis is performed after 6-12 weeks. In addition, a biopsy is prescribed without taking a sample of the endocervix, in order to avoid a threat to the embryo or fetus.
Conization for diagnostic purposes is required only when it is impossible to be sure that there is no malignant process; otherwise, according to the schedule suggested by the doctor, liquid cytology (or PAP test) and an instrumental examination of the cervix are performed. This is due to the fact that the risk of progression of the pathology is extremely small, and in the postpartum period the disease can regress. In any case, treatment of dysplasia should be carried out no earlier than after the end of the postpartum period.
Normal squamous epithelial cells
The presence of squamous epithelial cells in the smear is normal, since the entire cervix is covered with squamous epithelium. The normal volume of these cells in a smear can be up to 15 units per field of view. The absence or greater volume of cells indicates the presence of abnormalities in the body. However, an accurate diagnosis can only be established by assessing all study parameters. A small number of squamous epithelial cells in a Pap smear (up to 5 per field of view) indicates insufficient production of estrogen in a woman’s body.
Decoding the cytogram
NILM (cytogram without features) are normal indicators of the epithelium. All other terms are suspicious in terms of oncology and require further observation and additional examination.
ASC are atypical squamous epithelial cells. This is an intermediate state between normal and intraepithelial changes. Up to 17% of women with this result have cervical neoplasia (CIN, a precancerous condition of the epithelium), and 1 woman out of 1000 examined has an invasive cancer process determined by biopsy.
Epithelial cells with and without atypia
Atypia is a special condition of cells. They have an incorrect structure , and their shape, structure and dimensions are changed. This condition is one of the main signs of pathologies, including a high probability of developing cancer, since an atypical cell is a potential cell from which a tumor can form.
Even more interesting:
Tongue with HIV infection photo
Yarina or Dimia
If atypical cells are present in a cytology smear, it is usually assumed that a woman has developed HPV, vaginal infections, or the process of degeneration of epithelial cells into squamous cell carcinoma.
If there is a slight change in the morphological structure of the cells that were affected by inflammation occurring in the body of the uterus or vagina, the tests receive a second class with an explanation, that is, what disease could cause atypia. This could be inflammation, tumor, condylomas, HPV.
The third class requires a repeat examination, since the smear taken reveals cells with uncharacteristic abnormalities of the nucleus and cytoplasm. Dysplasia of several types can be observed: mild, moderate or pronounced.
The fourth class assumes the presence in the analyzes of cells with an uncharacteristic enlarged nucleus of a non-standard shape, while its cytoplasm is also changed and signs of malignancy are observed.
The fifth class is the study results in which the number of malignant squamous epithelial cells is significantly higher. In this case, invasive cancer .
If the study does not reveal atypical cells, then the diagnosis is established solely by measuring their number in the smear.
Cytological nasal smear
A cytological smear is prescribed for women not only if there is a risk of diseases of the genitourinary system . Quite often, this type of research is prescribed for studies of the nasal mucosa.
However, such an analysis is called a nasocytogram. Its task is also to study epithelial cells, as well as neutrophils, lymphocytes, monocytes, mast and plasma cells, and eosinophils. In addition, the characteristics of these cells are studied.
A nasal smear for cytology is carried out as follows. A special brush is used to collect epithelial cells from the lower nasal passage. In this case, the analysis is taken from both nostrils , so the left and right halves of the nose are examined separately.
Depending on the disease, the results of the study may show other results, according to which the doctor will be able to assess the patient’s health status and, if necessary, prescribe other studies to confirm the disease.
A clear example of damaged endometrium
Atypia, what is it in gynecology, is a question that a woman of any age may unexpectedly need an answer to. The term itself is generally clear; it corresponds to something incorrect, unnatural, i.e. not typical, but how this is connected with the female body and how dangerous it is requires a more detailed consideration.
What is meant by “atypical” in gynecology?
When speaking about atypia, gynecologists mean a variety of disorders that occur in the tissues of the female reproductive system at the cellular level. Essentially, this is the formation of abnormal cells, which manifests itself in a distortion of their structure and is accompanied by a number of signs indicating problematic malfunctions in the body, improper functioning of an organ or the entire reproductive system.
Most often, pathology develops on the cervix, because this part of the organ is primarily exposed to the adverse effects of external factors (viruses, bacteria, infections), the development of inflammation and other damage. As a result, when normal cells divide, atypical ones are formed, i.e. having an irregular structure, abnormal shape and size.
Cellular disorders in the tissues of the cervical walls and cervical canal can provoke the rapid development of abnormal layers. This in turn causes disturbances in the functioning of the organ. In addition, there is often a deterioration in blood circulation in these areas, which leads to the occurrence of such a type of atypia in gynecology as vascular, i.e. to distortion of blood vessels, which can enlarge and proliferate.
The described pathological processes often develop directly in the uterus; they can be closely related to endometrial hyperplasia (the internal mucous membrane of the organ).
Complications
If endometrial hyperplasia, the treatment of which is described above, is neglected, then unpleasant consequences may develop.
- The most dangerous complication is the development of an oncological process, endometrial cancer;
- Infertility due to endometrial damage;
- Anemia due to blood loss and its symptoms (pallor, drowsiness, weakness, etc.).
In general, with timely initiation of treatment, simple endometrial hyperplasia has a fairly good prognosis and is easily cured.
Endometrial hyperplasia and what it is
Hyperplasia is understood as a thickening of the layer of the inner mucous membrane of the uterus, which occurs with a violation of the ratio of glandular tissue and stromal tissue. The endometrium always reacts to changes associated with the cycle; in the first phase it grows, and if pregnancy does not occur, it is destroyed, and excess fragments leave the body with menstrual blood. When the hormonal balance is disrupted (increased estrogen synthesis and decreased progesterone levels), the proliferation of glandular cells continues, which leads to pathological proliferation. In gynecology, there are different types of this disease:
Symptoms
Manifestations of endometrial hyperplasia (its atypical form) do not have any specific differences from the symptoms of other forms of known hyperplastic processes. They are presented:
- disruptions in the rhythm of menstruation;
- uterine bleeding (usually irregular);
- spotting discharge at the time of postmenopause;
- profuse menstruation;
- bleeding during sex.
With the disease in question, abdominal pain does not occur.
Attention: in young girls, pathological growth of the “lining of the uterus” is often accompanied by infertility.
What can trigger the onset of atypical changes
Like any pathological processes, cell atypia is also not causeless. One of the main factors is hormonal disorders in the body, which is confirmed by the fact that most often pathologies develop in women 40 years of age and older, whose bodies begin to prepare for the menopause.
No less dangerous is the presence of factors such as:
- frequent gynecological diseases;
- having promiscuous sex life;
- injury to female organs (numerous abortions, wearing an intrauterine device);
- the course of chronic inflammatory processes;
- presence of HPV in the body;
- weakened immune system;
- too early onset of sexual activity;
- heredity.
How can the course of a pathological process manifest itself in the body?
Gynecological diseases and disorders usually present with symptoms that disrupt a woman's life and cause significant discomfort. Depending on the degree of development of the pathological process, the characteristics of the disease and its development, signs of atypia may be:
- disturbances of the menstrual cycle, its frequency and duration of menstruation;
- bleeding;
- painful menstruation;
- the appearance of spotting in the middle of the cycle, as well as continuing long after menstruation or occurring after sexual intercourse;
- problems with conception (infertility).
Very often, descriptions of cases of atypia in gynecology note that this is a phenomenon that can be asymptomatic. In the early stages, the absence of signs is almost always observed, so the disease can be detected only by diagnostic results.
Treatment
Treatment for epithelial cell abnormalities depends on the specific problem.
- If the cells are not cancerous, there is usually no immediate treatment, except for worse repeated tests.
- Treatment for cancerous lesions may vary from case to case. If they are detected early, the condition can often be treated with minor treatments such as laser treatment and radio wave therapy.
- More complex cases may require surgery, chemotherapy and radiation therapy.
How is the pathological process diagnosed?
To diagnose the pathological process, a gynecological examination is performed with colposcopy and smear collection for atypia. In the first case, we are talking about a visual study of the surface of the organ through a special optical device - a colposcope, and in the second - a laboratory study of scraping the epithelium from the affected areas, which is taken using a gynecological spatula or brush directly during examination with mirrors. Both procedures are completely painless.
Taking an analysis to identify the presence of pathology
The taken smear is sent to the laboratory for cytological examination. To establish for sure that this is cervical atypia, an assessment method such as PAP (or Papanicolaou cytogram) is used. The biomaterial is stained and then examined under a microscope for its cytoplasmic and nuclear structure:
- the type of pathological process is initially determined (it can be inflammatory, malignant);
- then the severity of atypia is determined;
- then differentiation is carried out between epithelial fragments.
Diagnostics
The diagnosis cannot be made based on patient complaints. For this purpose, the gynecologist recommends additional examination methods:
- hysteroscopy;
- Ultrasound of the uterus (transvaginal method);
- cytological examination;
- histological studies.
Hysteroscopy
This method is considered the most informative. The examination is performed under local anesthesia. Only occasionally is there a need for general anesthesia. After examining the uterus, the specialist identifies the focus of the growth, determines its size and location. He may take an endometrial biopsy. This research method can be carried out before curettage. It is also possible after this procedure. It helps to diagnose abnormal changes in 63–97% of cases.
During examination, the doctor sees swelling, thickening of the endometrial layer, a characteristic color (pale pink), and many points that are the outlet openings of the glands.
Histological examination
Carrying out diagnostics under a microscope guarantees an accurate diagnosis. The doctor receives a description of the structure of the epithelium, the structure of the nuclei, cells, and sees their deviations.
The procedure can be carried out during hysteroscopy, through pipel biopsy. The sensitivity of a biopsy to detect cell abnormalities and oncology does not provide a 100% accurate result.
Cytological examination
The aspirate obtained from the organ is examined under a microscope. This type of analysis is not as informative as histology. They use diagnostics during dispensary observation. It is necessary when assessing the quality of therapy.