Adenomyosis of the uterus is a benign gynecological disease affecting the myometrium of the organ. The pathology is characterized by increased proliferation of endometrioid tissue in the muscular layer of the uterus. This disease is otherwise called internal endometriosis, which is not cancer and does not pose a cancer risk.
Treatment of adenomyosis should be carried out exclusively by a specialist. The doctor conducts a differential diagnosis of pathology for cancer, fibroids, and endometrial hyperplasia.
Ignoring symptoms or self-treatment can lead to serious complications such as infertility, bleeding, and spread of the process to the pelvic organs.
Uterine adenomyosis is a widespread disease among women of reproductive age and often causes infertility.
Types of discharge
Normally, a woman may experience slight discharge. They are slimy, watery, with a whitish tint or transparent, odorless. Therefore, it is important to know what happens with endometriosis, what discharge may indicate its presence, and how they differ from the norm.
The disease is accompanied by various secretions, the appearance and characteristics of which can suggest the extent of the pathological process:
The initial stage of endometrial hyperplasia.
Characterized by changes in menstruation themselves. They become longer and more abundant. At the same time, previously scarlet blood becomes black.
If the bladder and rectum are affected.
In this case, bloody discharge will be noted during straining and emptying the intestines or bladder.
As the disease progresses.
Blood can be found on underwear and outside the onset of menstruation. This happens especially often during and after sexual intercourse or a gynecological examination. Such discharge in the middle of the cycle is usually dark in color and quite thick. Sometimes mucus is found along with it.
When adenomyosis affects the muscular wall of the uterus.
Then the lymphatic vessels are also involved in the process. And then the discharge will be watery, formed in large volumes. In addition, their strong smell attracts attention.
Transfer to neighboring organs.
The progression of the disease with the growth of the endometrium and its transition to other organs and tissues leads to the fact that various secretions in endometriosis become permanent. They can be observed at any time of the cycle, detected as spotting, blood clots, lumps.
Discharges with blood during menstruation and when the bladder and intestines are tense come from the pathologically overgrown endometrium, which causes the layer to be rejected, depending on cyclic changes. Intensification of the symptom occurs with physical activity , as well as with the accumulation of mucus in the cavities of the organs.
Diagnostic measures of the lesion
To determine diffuse focal adenomyosis of 13 and 15 mm, it is imperative to undergo an ultrasound examination, which will help determine the specific signs of the disease. A transvaginal scan will help identify an accurate diagnosis of the disease. If you do not begin timely treatment of focal adenomytosis of the uterus, then as a result, as already mentioned, the patient may experience infertility or she will have to undergo partial or even complete removal of the said organ.
Most often, this disease is diagnosed using ultrasound. To identify focal adenomyosis and possible uterine cancer, a biopsy and CA-125 test are performed. All this allows you to clearly examine the signs of pathology of both the organ itself and neighboring tissues. It is best to carry out such an examination before menstruation. The doctor will be able to accurately identify the nature of the disease, its shape, the size of the uterine body, the thickness of the walls and structures of the myometrium. To take a biopsy, the doctor prescribes a hysteroscopy.
Causes of unusual discharge
The reasons for the appearance of altered discharge during endometrial hyperplasia are as follows:
Increased volume of blood excreted during menstruation.
Occurs as a result of an increase in the area and depth of the endometrium with adenomyosis. Each additional area peels off the mucous membrane and at the same time the vessels are injured, bleeding becomes profuse.
It happens due to the fact that blood, when leaving unusual places, encounters mechanical obstacles and stagnates. The clots have coagulated and come out gradually from the vagina.
The duration of bleeding increases.
Since all the exfoliated mucous membrane is not able to come out within the standard 7-day period. Menstruation may double or more in duration; in recent days, brown spotting (residues from distant areas) is noted.
Associated with the inflammatory process. It can cause the development of endometriosis, or act as a complication of this disease.
There are advanced cases when the endometrium grows unevenly in different places.
Appear as a result of the addition of pathogenic flora. In this case, discharge occurs at any time, it has a yellow or greenish tint and an unpleasant odor.
Why is nodular adenomyosis dangerous?
Unlike other types of adenomatosis, the nodular form is the least common. The disease is the growth of benign endometriotic tissue in the thickness of the muscular walls of the uterus in the form of one or several nodes.
An adenomyosis node in the uterus is a collection of deformed endometrial glands, connective tissue and altered muscle structures, from which a neoplasm is formed, shaped like a node. In the periphery of the node, the tissues are compacted. In the center of the formation there is one or more cellular cystic cavities filled with pathological, bloody-brown exudate.
Adenomyosis node comes in the following varieties:
- Active. It is equipped with good blood flow, vigorous growth of pathological tissue and a rapid increase in size.
- Inactive. Blood circulation in the node is weak, the epithelium is atrophic, and the proliferation of pathological tissues is not observed.
- Combined. Combines the characteristics of the two previous forms.
The nodular form of adenomyosis rarely develops on its own. It is often combined with diffuse adenomyosis, as well as the following gynecological pathologies:
- uterine fibroids;
- endometrial hyperplasia;
- uterine polyposis;
- malignant neoplasms in the body of the uterus.
If the nodular form of adenosyosis is not treated, the risk of developing the following dangerous consequences increases:
- Malignization. Active nodes grow rapidly and, under a confluence of unfavorable factors, can develop into a malignant tumor. A particular threat is posed by hyperplastic nodes with cellular atypia, which often become the source of adenocarcinoma.
- Infertility. The progression of the pathology leads to deformation of the uterus and disruption of the menstrual cycle, which prevents normal conception and bearing a child. Even if the fertilized egg is implanted, the risk of premature birth and miscarriage at a later date is high.
- Secondary anemia. Accompanied by a deterioration in general well-being, partial or complete loss of performance.
- Decreased quality of life. At stages 2–3, a woman is bothered by severe pain, heavy menstrual bleeding, iron deficiency anemia, and vegetative-vascular disorders, which significantly reduce the quality of life.
- Disruption of the normal functioning of neighboring organs. In advanced cases, one or several large nodes protrude beyond the body of the uterus, often growing into neighboring organs, leading to disruption of their normal functioning and the development of associated complications.
Question: What type of discharge occurs with adenomyosis?
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
What type of vaginal discharge occurs with adenomyosis?
Discharge with adenomyosis is bloody. Moreover, there are two types of bleeding:
1.
Discharge colored dark burgundy or dark red. Such shades of discharge are given by the presence of relatively fresh blood with undisintegrated formed elements;
2.
Discharge colored dark brown, a characteristic color also called “chocolate”. This coloration of the secretions is provided by the so-called “old” blood, in which some of the formed elements have undergone decay.
Discharge of dark burgundy or dark red color is observed in cases where foci of adenomyosis do not have a capsule or are located close to the inner surface of the uterus. This state of affairs is due to the fact that the rejected areas of adenomyosis foci quickly end up in the uterine cavity, from where they are pushed out, forming characteristic discharge. Between the moment of their rejection and removal outside, a relatively short period of time passes, during which the formed elements of the blood do not have time to undergo decay. Typically, dark burgundy and dark red discharge is characteristic of the diffuse form of adenomyosis.
If the foci of adenomyosis have a capsule or are located deep in the thickness of the muscular layer of the uterus, then the discharge, as a rule, is “chocolate”. This is due to the fact that the rejected elements and spilled blood remain inside the capsule for some time, during which they disintegrate, as a result of which they acquire such a characteristic “chocolate” color. Indeed, from the moment of tissue rejection in the adenomyotic lesion to their release to the outside, a relatively long period of time passes, during which they partially disintegrate, taking on a very characteristic “chocolate” color. This is the color that gives the discharge the disintegrated formed elements of blood. Discharge of a dark brown, “chocolate” color is characteristic of focal or nodular forms of adenomyosis.
Both dark burgundy and “chocolate” discharge due to adenomyosis are observed for several days before or after menstruation. In other parts of the menstrual cycle, spotting, as a rule, does not appear.
In addition to spotting of various colors and patterns, adenomyosis can cause bleeding during any phase of the menstrual cycle.
Adenomyosis is a benign pathology of the uterus, which consists of pathological growth of the endometrium into the myometrium. In this case, an inflammatory process develops.
The disease occurs when there is a malfunction in the hormonal balance and immunological disorders.
A feature of adenomyosis is the germination of pathological foci only in some areas of the reproductive organ; total damage to the uterus is not observed.
Uterine adenomyosis is a hormone-dependent pathology that is most often diagnosed in women of reproductive age and prevents conception or pregnancy.
Currently, there are various methods for early diagnosis of the disease, which can significantly increase the effectiveness of treatment.
The main methods of treating the lesion
It is important to remember that only the first two stages of adenomyosis can be treated. But for those who suffer from such a lesion, unfortunately, complete recovery, as a rule, does not occur. This can be explained by the fact that the focal form of adenomyosis in the uterine cavity often reappears, for this reason it is important for the patient to carefully monitor the hormonal system.
All types of adenomyosis are treated with two common methods. In the first case, the specialist prescribes the use of drugs against adenomyosis. If such therapy does not improve the person’s condition, then specialists prescribe surgery. All methods for removing internal endometriosis will differ from each other depending on the severity and germination of the lesion, as well as the state of the woman’s reproductive system.
The most common method for removing the lesion is uterine artery embolization. Other procedures to remove the affected area, including curettage, are quite dangerous and can lead to infertility.
To begin proper treatment for uterine disease, the specialist will rely on the following factors:
- woman's age;
- presence or absence of children, desire to have children in the future;
- absence of childbirth;
- stage of development of the lesion;
- main symptoms of damage and their manifestation.
If a woman has any problems with the functioning of the kidneys, liver, blood vessels, or has diabetes mellitus, then he prescribes a course of taking hormonal medications. Whether to remove uterine adenomyosis will be decided by the attending physician after a diagnostic examination. He will examine the woman’s medical history and identify the presence of asthma or obesity. And the goal of treating the disease will be to introduce the woman into a medicated menopause.
Internal endometriosis should be treated with hormonal agents, but it is important to remember that they often provoke adverse reactions. During treatment, a woman must follow a special diet and exclude all harmful foods from her diet. The menu should include as many foods as possible enriched with proteins and vitamins. Additionally, the doctor prescribes immunotherapy and physiotherapy. With a focal form of uterine adenomyosis, a woman often develops neurotic diseases in the background, for which the help of a psychotherapist is very important.
What is adenomyosis?
The endometrium in a healthy woman’s body is constantly growing and being rejected.
In the first phase of the menstrual cycle, the growth of the endometrial layer begins, which is necessary so that the fertilized egg can attach to the walls of the uterus and continue its development.
If conception does not occur, the endometrium is rejected - menstruation begins, after which only the growth layer of the endometrium remains in the uterine cavity, and the process is repeated again.
There are such forms of adenomyosis:
- focal - characterized by a single germination of the endometrium into the muscular layer of the uterus;
- nodular – formation of dense nodular formations without a capsule;
- diffuse – uniform distribution of pathology;
- mixed - signs of several forms are present.
As for the stages of the disease, there are 4 of them:
- first stage – the lesion is shallow and there are no clinical signs;
- second stage - the endometrium penetrates up to half of the myometrium;
- third stage - the lesion is more than half;
- fourth stage - the endometrium penetrates through the myometrium and can affect neighboring organs.
Features of the disease
To understand what it is - focal adenomyosis, let's talk about the features of the pathology. The endometrial layer is found throughout the uterus. It is regularly renewed through the menstrual cycle. This helps prepare a woman’s body for possible fertilization and gestation of an embryo. Focal adenomyosis of the uterus occurs, as a rule, in older women who are over 40 years old and have experienced the first symptoms of menopause.
In such women, regular changes in the level of estrogen in the body can be noted. At the same time, they experience hot flashes, sweating increases greatly, and they also begin to feel dizzy. If such surges continue for too long, then against their background the woman begins to develop adenomyosis of a focal form of the lesion.
This pathology is a type of internal endometriosis, which can be diffuse and affect the entire uterine cavity. Focal adenomyosis is characterized by a specific location of the endometrium in various parts of the uterus.
The main problems in diagnosing and preparing treatment for the disease lie in identifying the stage of the lesion. There are several forms of this disease, two of which are amenable to medical treatment, and the rest can only be eliminated through surgery.
First signs
The leading symptom of adenomyosis is heavy and prolonged menstruation, which can lead to the development of anemic syndrome. Therefore, symptoms of anemia may also represent indirect signs of this pathology.
The symptoms of anemia are as follows:
- increased weakness;
- susceptibility to infectious diseases;
- drowsiness;
- pallor of the skin and mucous membranes;
- dizziness;
- decreased performance;
- fainting.
Also a characteristic sign of adenomyosis is the presence of spotting vaginal discharge. They can appear a few days before the start of menstruation and continue for some time after it ends.
In addition, the disease often leads to the development of neuroses, as well as instability to stressful situations. If neighboring organs are affected by the disease, their functionality may deteriorate.
Disease development process
Features of the formation of the lesion site in the focal form of adenomyosis look like this:
- the formed lesions do not form a capsule;
- they are distinguished by their infiltrative growth and can easily spread to nearby tissues;
- endometrioid cells lead to the onset of destruction of the affected tissue;
- they, just like malignant cells, rapidly spread throughout the body through the bloodstream and lymph.
Gynecologists report that the internal form of endometriosis of the uterus is a rather dangerous disease, which is very important to treat in a timely manner, since otherwise it can lead to serious complications.
In the absence of proper treatment, the patient may experience infertility. In addition, the symptoms of endometriosis most often represent severe pain, which can negatively affect the general condition of a woman, worsening her well-being and activity.
Main symptoms
The complexity and spread of pathology is an individual symptom, so each specific patient may not experience the same symptoms, and the severity may also be different.
The initial stages of the disease are not accompanied by any symptoms, and adenomyosis can be suspected based on the clinical picture only starting from the second stage. At this point, the endometrium grows deeper into the myometrium, and a nodular or diffuse form of the disease may develop.
If we talk about the patient’s age, a more vivid clinical picture is observed in women from 25 to 35 years old.
Symptoms of adenomyosis:
- chronic pain that is localized in the pelvic area. Observed in 76% of all cases;
- heavy menstruation. More often observed in nodular and diffuse forms of pathology. Blood loss can be very significant and cause the development of anemia. Observed in 60% of cases;
- intermenstrual uterine bleeding is observed in half of the patients;
- painful menstruation. Occurs infrequently – in 20% of cases;
- pain during intimacy – in 7% of cases;
- feeling of pressure in the uterus;
- frequent urge to urinate, painful urination and other bladder problems are observed if the enlarged uterus puts pressure on the bladder;
- uterine enlargement – diagnosed in 30% of cases;
- high sensitivity in the area of the reproductive organ;
- subfertility and infertility - diagnosed in 15% of cases. In addition, the disease can provoke premature birth and previously spontaneous termination of pregnancy.
Patients with adenomyosis often suffer from the following pathologies:
- in half of the cases, myomatous nodes in the uterus are observed;
- 11% are diagnosed with endometriosis;
- in 5% - polypous formations in the endometrium.
And changes in the menstrual cycle can be as follows:
- increased volume of menstrual blood;
- shortening of the cycle or, conversely, delay of menstruation;
- prolongation of menstruation - more than a week;
- soreness;
- presence of blood clots in menstrual blood;
- spotting before and after menstruation;
- acyclic secretions;
- severe premenstrual syndrome.
Risk factors
The most common risk factors for adenomyosis are:
- problems with the functioning of the endocrine system;
- woman's age;
- heredity;
- socio-economic status.
Uncommon factors:
- late onset of menstruation;
- late labor or childbirth with complications;
- regular abortions;
- strong radiation and thermal procedures aimed at the pelvic area.
Unfortunately, conservative or combined treatment in rare cases leads to a woman’s complete recovery. Late stages of the disease are a common cause of infertility. But timely treatment helps to achieve more or less long-term remission, get pregnant and give birth to a child. True, in this case it is important to remember that the risk of spontaneous abortion or the onset of premature labor is high.
Causes
The reasons for the development of the disease may be the following:
- heredity;
- hormonal imbalance;
- violation of metabolic processes;
- weak immunity;
- age-related changes;
- inflammation in the reproductive system;
- frequent abortions;
- early onset of menstruation;
- stress;
- heavy physical activity or a sedentary lifestyle.
At risk are women after surgical manipulations in the uterus or abdominal cavity, as well as after cesarean section.
What kind of pain can it be?
Pain in sick women with adenomyosis appears due to compression of the nerve endings by the enlarged uterus.
Most often, pain with adenomyosis is not constant and occurs only before and during menstruation, but in some cases a woman may be bothered by chronic pain.
The pain starts in the lower abdomen and spreads to the perineum, hips and lumbar region. If the pain is observed constantly, then a few days before menstruation it becomes more intense.
The intensity of pain directly depends on the extent of the pathological process.
Focal adenomyosis of the uterus - treatment
The choice of treatment method for focal adenomyosis is often a big problem and largely depends on the age of the patient, the degree of prevalence of adenomyosis, the severity of clinical manifestations, and the presence of concomitant genital and somatic diseases.
Stages or extent of adenomyosis
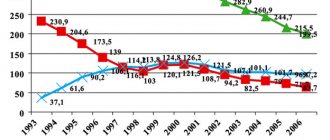
| Adenomyosis | Prevalence |
| 1 degree minimum | Invasion of the endometrium into the myometrium is limited to the transition zone (JZ) |
| 2nd degree mild | The growth of endometrioid tissue into the myometrium is limited to half the thickness of the uterine wall |
| 3 degree moderate | Damage to the entire thickness of the uterine wall up to the serous (outer) lining of the uterus, without germination into it |
| 4th degree severe | Invasion of the pathological process into the serosa and beyond the uterus |
Treatment tactics for adenomyosis are always agreed upon with the patient and are primarily based not on ultrasound results, but on the complaints presented and the objective clinical picture.
Focal adenomyosis 1 and 1-2 degrees - treatment
Detection of signs of grade 1-2 adenomyosis on ultrasound is not an absolute indication for hormonal treatment.
A number of experts believe that if the patient has no health complaints, no clinical manifestations of the suspected (not confirmed by histology) disease, then hormonal treatment is not prescribed. An examination by a gynecologist and ultrasound control is recommended once every 6 months.
At the same time, many researchers insist on the advisability of long-term restraining treatment of mild forms of adenomyosis with low-dose monophasic oral contraceptives or pure gestagens (oral, intrauterine) with a minimal load (dienogest, levonorgestrel) until the moment of planned pregnancy or the onset of natural menopause.
Focal adenomyosis 2 and 2-3 degrees - treatment
Management of mild and moderate focal adenomyosis depends on the form and severity of the clinical manifestations of the disease.
Analgesics and NSAIDs are used to treat minor pain.
In cases of more significant symptoms, conservative hormonal therapy is performed.
Drugs for the treatment of focal adenomyosis
(according to the recommendations of international clinical societies, consultation with the attending physician is required)
First-stage therapy does not require histological confirmation of the diagnosis. Applicable:
- Monophasic COCs in continuous mode: the drug of choice is “Janine” (dienogest + ethinyl estradiol). Generics: “Siluet”, “Bonade”, “Diecyclen”
- Continuous gestagens: the drug of choice is Visanne (dienogest).
Clinical case:
The patient's complaints: pelvic pain, prolonged heavy menstruation.
Ultrasound results: in the left corner of the uterus, closer to the outer (serous) covering, a heteroechoic formation 3.5 x 5.3 x 4.2 cm with finely dispersed contents inside, with a hyperechoic peripheral rim up to 2 cm was detected. Deformation of the outer myometrium. Signs of focal adenomyosis.
MRI results: focal adenomyosis was confirmed.
Surgical treatment was proposed, but the patient refused.
Prescribed: Visanne drug in continuous mode.
Clinical effect: positive.
Second-stage therapy is prescribed if first-stage therapy is ineffective or intolerable:
- LNG-IUS "Mirena" (levonorgestrel)
- A-GnRH course of no more than 24 weeks: Experts' choice - "Diferelin" (triptorelin) Generics: "Decapeptyl-depot", "Triptorelin-long" Popular A-GnRH: "Zoladex" (gozorelin), Buserelin.
Focal, diffuse-focal adenomyosis 3, 3-4 degrees - treatment
Isolated moderate-to-severe and severe adenomyosis is extremely rare. More often it is combined with uterine fibroids, ovarian pathology, endometrial and/or myometrial hyperplasia, is accompanied by severe symptoms and is treated promptly.
Clinical case:
The patient's complaints: severe pelvic pain.
Ultrasound results: A heteroechoic formation measuring 4.3 x 5.1 x 3.5 cm with an outer zone of increased echogenicity was detected along the left rib of the uterus in the lower third of the myometrium. Deformation of the external myometrium with bulging into the abdominal cavity. Signs of focal adenomyosis.
MRI results: presumably focal adenomyosis.
Conservative surgical treatment: successful organ-preserving therapeutic laparoscopy was performed with excision of the pathological focus and subsequent restoration of the uterine wall.
Histological diagnosis: focal adenomyosis.
Is surgery necessary?
Indications for surgical treatment of focal adenomyosis:
- Ineffectiveness of conservative therapy.
- Menstrual or acyclic uterine bleeding associated with adenomyosis, leading to anemia, resistant to drug treatment.
- Chronic pelvic pain, dyspareunia, significantly reducing the standard of living, resistant to drug treatment.
- Adenomyosis in combination with other gynecological pathology requiring surgical treatment.
- Diffuse nodular adenomyosis grade 3-4.
- Adenomyosis-associated dysfunction of organs adjacent to the uterus.
In young women interested in preserving their fertility, organ-preserving reconstructive plastic surgery is performed whenever possible. The optimal surgical approach is laparoscopic.
In pre- and postmenopausal women, supravaginal or total (complete) amputation of the uterus is performed - hysterectomy.
Hysterectomy is an unfavorable outcome of late diagnosis or inadequate drug therapy for adenomyosis.
Total removal of the uterus is a necessary measure, a sad result of a woman’s late visit to the doctor, the wrong choice of conservative therapy, or the patient’s refusal for personal reasons from recommended hormonal treatment.
Every woman who does not comply with the drug treatment prescribed by her doctor for adenomyosis should be aware of the possible negative consequences of such a decision.
Possible Long-Term Consequences of a Hysterectomy Return to Contents
Danger of pathology
How can adenomyosis be dangerous?
If the disease is not treated in a timely manner, it can cause the following complications :
- Iron-deficiency anemia;
- chronic miscarriage;
- infertility;
- spread of pathological foci to neighboring organs.
As for whether adenomyosis can develop into cancer, the risk of this is small, but this possibility cannot be completely excluded.
Nodular adenomenosis and pregnancy
According to studies, 30-50% of women experience infertility due to adenomyosis, but this figure has little evidence, because the connection of adenomyosis with infertility is difficult to explain.
According to studies, 30-50% of women experience infertility due to adenomyosis.
As a rule, if a woman becomes pregnant easily, then she is able to easily carry a child, but miscarriages in the early stages are characteristic of this disease.
When pregnancy occurs, there is every chance of pregnancy if appropriate treatment is carried out to improve the condition of the uterus, so that the fertilized egg can “fix” itself. If a woman lacks hormones, then they must be taken in the first trimester of pregnancy.
How do periods change?
Most often, with adenomyosis, periods are very heavy. This is due to the fact that the concentration of estrogen increases and the endometrium thickens.
To stop this process, progesterone is needed, which can reduce the amount of estrogen, and, therefore, menstruation will become less abundant.
Spotting before and after menstruation is the result of a hormonal imbalance; hormones enter the blood unevenly.
Scanty periods with adenomyosis are a rare occurrence and can be observed at the initial signs of pathology, when there are no other clinical signs yet.
Pain during menstruation is a common phenomenon, which is a consequence of the swollen reproductive organ squeezing healthy cells and nerve endings.
Prevention
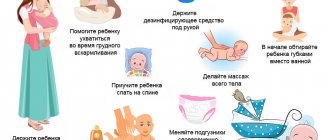
To prevent the development of nodular adenomyosis, gynecologists advise following these simple rules of prevention:
- Treat endocrine and hormonal disorders and infectious diseases in a timely manner.
- Have a protected sex life.
- Observe personal hygiene rules.
- Control your weight.
- Give up bad habits and lead a healthy, active lifestyle.
- Eat healthy foods rich in vitamins, micro- and macroelements.
Visit a gynecologist at least once a year and undergo a preventive medical examination, which will help diagnose the disease at the initial stage, successfully treat it, and prevent complications and relapses.
Nature of the discharge
Long-term spotting before and after menstruation most often has a thick consistency and brown color.
In this case, hormonal imbalance prevents the proper development of the endometrium, and bloody fluid can accumulate in pathological foci, which does not come out with menstruation, but begins to be released later.
Bleeding with adenomyosis is also a fairly common phenomenon, which often occurs with the nodular form of the disease or with uterine fibroids in combination with adenomyosis.
Diagnostics
The slightest suspicious signs indicating a gynecological pathology should be a reason to make an appointment with a gynecologist as soon as possible, who will be involved in treatment. At the initial examination, the doctor will listen to complaints, collect important data, conduct palpation and a gynecological examination, during which the following is determined:
- soreness of the uterine body;
- increase in organ size;
- change in shape and consistency.
To confirm the diagnosis, a referral is given for additional examination, including the following procedures:
- Ultrasound. An informative, painless method that will help identify pathology at the very beginning of its progression. With focal adenomyosis, zones with smooth, round contours are found in the body of the uterus. In the pathological focus, areas with different echogenicity are visualized.
- Hysteroscopy. The procedure is minimally invasive and is performed using an optical hysteroscope device, which is inserted into the uterine cavity through the vagina. Characteristic signs of focal adenomyosis are enlargement and deformation of the uterine body, changes in its relief.
- Biopsy. A fragment of excised tissue is examined under a microscope, a histological analysis of the biopath is performed, after which the correct diagnosis can be determined.
- MRI. A clarifying diagnostic method that is prescribed in the case of combined gynecological pathology. The technique has the greatest accuracy and is characterized by error-free data, but is prescribed only in special cases when other diagnostic methods do not provide comprehensive results.
Possible consequences
The disease has two development paths – favorable and unfavorable.
If the disease is detected and treated in a timely manner, the consequences are usually insignificant - the woman’s health and her reproductive function are restored and preserved.
In the second scenario, not only infertility due to hormonal imbalance is possible, but also removal of the affected organ, which eliminates the possibility of conception.
Treatment methods
Conservative treatment of adenomyosis consists of taking hormonal drugs.
Appointed:
- oral contraceptives;
- antigonadotropins;
- progestogens;
- antiestrogens;
- GnRH analogues;
- antiandrogens.
Also shown:
- non-steroidal anti-inflammatory drugs;
- drugs that affect the immune system;
- vitamins;
- physiotherapy;
- treatment with folk remedies.
It may consist of:
- in removing the pathological endometrioid layer;
- in excision of part of an organ affected by the disease;
- in complete removal of the organ.
The operation can be performed:
- abdominal;
- hysteroscopic;
- laparoscopic pics.