Installation of an intrauterine device is a gynecological procedure that involves inserting a special device into the uterine cavity.
The administration is carried out on an outpatient basis. Before undergoing the procedure for inserting an IUD, a woman undergoes a comprehensive examination to determine the presence/absence of contraindications. The IUD is used to provide a contraceptive effect for both nulliparous and parous women.
Contraindications to the installation of an intrauterine device
It is prohibited to install an IUD if there are congenital or acquired anomalies in the shape of the uterus, which do not allow the future placement of the IUD to be determined as accurately as possible, or if there is an allergy to copper or other components of the device.
Content:
- Contraindications to the installation of an intrauterine device
- Algorithm for carrying out manipulation
- Types of spirals
- Benefits of having an IUD
- Side effects
- Installing an IUD after pregnancy
It is strictly forbidden to insert an IUD during pregnancy, the presence of benign or malignant formations in the uterine cavity, the presence of malignant tumors in the pelvic organs, uterine bleeding of no specific origin, genital infections, aggravated chronic inflammatory processes of the genitourinary system in women, as well as when there are diseases of the small organs. pelvis of acute inflammatory origin.
Features of care after insertion of an intrauterine device
To ensure normal recovery after IUD insertion and reduce the risk of adverse complications, the patient should adhere to the following recommendations:
- Maintain long rest;
- Visit a gynecologist a month after installing a contraceptive in order to prevent its displacement;
- Return to daily activities only after pain and discomfort have completely disappeared;
- Every month, check the location of the “antennae” with your fingers (they should be in the posterior vaginal area);
- Strictly adhere to all instructions of the treating doctor.
If one of the following pathological symptoms appears, the patient should consult a doctor for emergency medical help:
- Change in the length of the “antennae” or their absence during palpation;
- Heavy and painful menstruation;
- Suspicions of pregnancy;
- Descent of the spiral from the uterine cavity;
- Increased menstrual cycle;
- The appearance of signs of a sexually transmitted disease (in a partner or patient);
- Missed, short or late menstruation;
- Pain, bleeding during intimacy;
- Soreness or severe cramping in the lower abdomen;
- Unexplained fever, chills;
- Pathological vaginal discharge;
- The presence of ulcers and various rashes on the genitals;
- Unexplained vaginal bleeding;
- Symptoms of a heart attack or stroke;
- Attacks of headaches, migraines;
- Pain, aches, muscle weakness;
- The appearance of flu-like symptoms.
The IUD is a highly effective method of contraception, which, if the technique and rules for installing the intrauterine device are followed, does not bring any unpleasant sensations to the patient. Our clinic employs experienced and qualified doctors who, based on the results of comprehensive diagnostics, will select the most optimal option for an intrauterine contraceptive device and carry out high-quality and prompt installation of the IUD.
Attention!
This article is posted for informational purposes only and under no circumstances constitutes scientific material or medical advice and should not serve as a substitute for an in-person consultation with a professional physician.
For diagnostics, diagnosis and treatment, contact qualified doctors! Number of reads: 19701 Date of publication: 08/03/2017
Gynecologists - search service and appointment with gynecologists in Moscow
Algorithm for carrying out manipulation
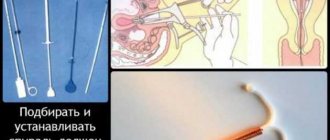
The procedure itself is quite simple. It is recommended to insert the IUD on the third or fourth day of the start of the menstrual cycle. General anesthesia is not used for the procedure; for sensitive women, only an anesthetic gel is used, which is directly applied to the cervix.
The woman is comfortably placed on the gynecological chair in a standard position. The gynecologist treats the cervical area and vaginal cavity with a three percent solution of hydrogen peroxide to remove residual menstrual fluid. After treatment with hydrogen peroxide, double treatment with an antiseptic is carried out.
Preparation includes: opening the package and carrying out verification manipulations regarding the horizontal position of the spiral, installing the spiral in a special conductor tube (the slider must be moved forward as far as possible), measuring the distance from the fundus of the uterus to the external pharynx with a special probe.
The IUD is inserted into the uterus through the cervical canal (the index ring should be two centimeters from the cervix), then manipulation is performed to open the horizontal shoulders of the IUD.
The fixation procedure involves:
- move the slider down as far as possible and release the contraceptive completely, carefully remove the guide tube from the uterus;
- cut the threads, leaving only a length of 2-3 centimeters from the uterine os;
- A correctly installed coil does not cause any discomfort, bleeding or pain.
The entire procedure will take approximately seven minutes in total. After carrying out manipulations to install the intrauterine device, it is recommended to undergo a control ultrasound diagnostics in order to ensure the correct position of the device. Women are recommended to spend the day after the procedure in gentle bed rest. For pain relief, you can use antispasmodics and analgesics. Pain syndrome is observed only in the first 14 days; all further pain is a sign of an urgent visit to a gynecologist.
After one month, it is recommended to visit your gynecologist for a follow-up examination. During this period, the doctor conducts a standard examination and ultrasound diagnostics. Sexual activity can begin four days after insertion of the IUD, provided there is no bleeding or pain.
Anti-pregnancy coils - essence and action
The principle of operation of an intrauterine device with metal is as follows: copper, silver or gold supports aseptic inflammation in the uterus. Aseptic means that it does not happen due to microbes and does not threaten anything. But the effects of metals essentially change the composition of cervical mucus, making it harder for sperm to penetrate the uterine cavity. In addition, copper or gold is good at preventing the egg from attaching to the uterine wall.
Installing an intrauterine device made of plastic, which contains progesterone, an analogue of the human hormone that prevents pregnancy, is the optimal choice for effective protection against pregnancy. The best IUD of this type (Mirena) inherently also interferes with the forward movement of sperm and the implantation of a fertilized egg, and at the same time also suppresses ovulation in some women.
How much does an intrauterine device cost? Spirals from different manufacturers and with different compositions are installed intrauterinely for a period of three to seven years. It is important to note that after the specified period of the device being in the uterine cavity, the device must be removed, since failure to comply with the deadlines is fraught with adverse consequences for women’s health.
When can I install a spiral?
In gynecology, spirals are recommended by doctors for use in the following situations: 1). The desire of the woman herself at this stage of life not to become a mother (provided that there is already a history of childbirth). 2). Frequent pregnancies with other types of contraception (if they are used incorrectly or are not taken carefully). 3). Protection against unwanted pregnancy during lactation (breastfeeding). 4). In order to save money. IUDs are installed for several years, which allows a woman not to worry about other types of contraception (oral contraceptives, condoms).
What are the contraindications
- Established or suspected pregnancy.
- Infectious diseases of the pelvic organs (including sexually transmitted diseases or those associated with complications after termination of pregnancy).
- Oncological diseases of the uterus or cervix and cervical canal.
- Vaginal bleeding of unknown origin.
- Congenital or acquired pathology of the uterus: bicornuate uterus, underdevelopment of the organ.
- The woman has a history of ectopic pregnancy.
- A history of complicated abortion (less than three months).
- Congenital or acquired defects of the cervix.
- Diabetes mellitus in the stage of decompensation.
- There are additional restrictions for the IUD with hormones, just like for taking hormonal contraceptives.
Pregnancy with an IUD
In case of intrauterine pregnancy up to 12 weeks, the IUD is urgently removed. Further development of the fetus depends on the desire of the woman. If she decides to keep the baby, then she should remember the need for strict monitoring by a specialist over the entire period of pregnancy, as there is a risk of complications. If the pregnancy is more than 12 weeks, the intrauterine device is removed during childbirth.
Pros of the intrauterine device
- high efficiency; — possibility of long-term use; - immediate contraceptive effect; — rapid restoration of fertility after removal of the IUD; - lack of connection with sexual intercourse; - low cost (with the exception of the hormonal intrauterine system); — possibility of use during lactation; - therapeutic effect for some gynecological diseases (for the hormonal intrauterine system).
Spiral for nulliparous women.
Contrary to popular belief, the IUD can be installed in women who have never given birth or become pregnant before (but it is better to use the IUD after 20 years, when the internal organs are fully formed). IUDs have a reversible effect, and you can get pregnant literally in the first month after removing the IUD. In addition, IUDs for nulliparous girls do not increase the risk of developing cancer and can be combined with any medications.
Disadvantages of intrauterine contraception
Every woman who decides to have an IUD should be aware of the possible side effects and complications that may result from using this method of contraception. Side effects of IUDs and negative qualities of IUDs include:
- increase in the duration of the menstrual cycle and the amount of discharge;
- the appearance of “spotting” between menstruation;
- spasms and discomfort in the pelvic area during menstruation;
- risk of ectopic pregnancy;
- the appearance of an unpleasant odor from the genital tract;
- a decrease in the thickness of the endometrium, which can make it difficult to carry a pregnancy in the future, as well as increase the risk of miscarriage.
In some cases, if the spiral is incorrectly selected or the gynecologist is insufficiently qualified, the following complications may occur: infection of the pelvic organs or the development of inflammation; perforation of the uterine wall; pain in the lower abdomen due to the wrong size of the product; displacement and spontaneous loss of the spiral. The downside of the IUD is that gynecology categorically does not recommend it as a means of contraception at a young age (up to 20 years).
Intrauterine devices do not protect against STIs (sexually transmitted infections)! It is recommended to use this contraceptive if you have a regular sexual partner (low risk of transmitting sexually transmitted diseases).
YOU SHOULD GO TO A GYNECOLOGIST URGENTLY IF:
- an increase in temperature for unknown reasons a few days after installing the coil;
- severe pain or discomfort in the pelvic area;
- vaginal discharge of an unusual color or odor;
- pain or discomfort in the lower abdomen, vagina during sex;
- loss or displacement of the spiral;
- delay of menstruation by 3-4 weeks.
Installation of the spiral
The intrauterine device is intended for one-time use and is installed exclusively by a gynecologist after examination and strictly in accordance with the instructions. You can insert the IUD on the 4-7th day from the start of menstruation. During this period, the cervix is slightly open, which makes it easier for the device to enter the uterine cavity and cause minimal discomfort to the woman. The IUD can be inserted immediately after an artificial termination of pregnancy or 2-3 months after childbirth, and after a cesarean section - no earlier than 5-6 months.
In our clinic, the gynecologist installs the spiral in accordance with all established standards and technological requirements. By making an appointment with a specialist, you will undergo the necessary preliminary examination (examination, ultrasound, tests). Only after this is the installation of an intrauterine device carried out, the high effectiveness of which has been proven by numerous clinical trials. When an IUD with hormones or gold is inserted, the patient receives an original certified product from an official supplier in Moscow and throughout the Russian Federation.
Analyzes before the spiral.
Before inserting the IUD, testing will help the gynecologist decide whether or not to recommend this method of contraception. The doctor should interview the patient to identify possible contraindications, perform a gynecological examination and bacterioscopic examination of smears from the vagina, cervical canal, urethra for microflora and degree of purity, PCR analysis for hidden infections, ultrasound of the uterus and appendages. The IUD can be inserted only with smears of I-II degree of purity.
If you plan to install the Mirena spiral, which is a hormone-containing drug, therefore, before installing it, in addition to all of the above, it is advisable to consult an endocrinologist and conduct a blood test to determine the level of sex hormones, hemostasis (clotting) indicators, and biochemistry. It is also necessary to conduct an examination of the mammary glands and their ultrasound scanning.
How a gynecologist places an IUD
The procedure itself is not very pleasant, but not much worse than a regular examination by a gynecologist. Stages of introducing the IUD in the clinic:
- The woman takes off her clothes below the waist and sits in a gynecological chair.
- After treating the genitals, the doctor opens and fixes the cervix with a mirror.
- 1-2 injections are made with a thin needle near the cervix for the purpose of local anesthesia.
- Having measured the depth and direction of the uterine cavity with a medical probe, the gynecologist inserts the spiral along the guide.
- Having installed the coil, the doctor pulls the guide tube back and removes it.
- At the end of the procedure, the doctor trims the “antennae” of the contraceptive, leaving 2-3 cm of thread length.
A woman should be informed about the recommended duration of wearing this type of IUD, as well as about the symptoms of possible complications that require urgent medical attention. A follow-up visit is recommended 7-10 days after installation of the IUD, then, if the condition is normal, after 3 months. During these visits, it is highly recommended to perform an ultrasound of the pelvis (uterus and appendages) to clarify the position of the device in the uterine cavity.
After the spiral
The IUD usually does not cause any discomfort to the patient during the entire period of use. After installing the spiral, it is not felt either by the woman herself or by her sexual partner; only two short tendrils are released from the cervical canal (from the cervix). These are strings that help make sure the IUD is in place. These same mustaches do not interfere in everyday life, including during sex. Subsequently, they will help the gynecologist remove the IUD. For 7-10 days after the introduction of an intrauterine contraceptive, it is recommended to limit physical activity, not take hot baths, laxatives and uterotonics, and avoid sexual activity. Sometimes after installation a woman may feel discomfort and dizziness, but they pass quite quickly.
Disorders of the reproductive system may manifest themselves in the first months after installation of the IUD in the form of a heavy or prolonged menstrual cycle. In some cases, aggravated dysmenorrhea may be observed, and less commonly, dyspareunia, cervical perforation, inflammatory reactions in the pelvic organs and unusual uterine discharge. Frequent side effects associated with individual intolerance are allergic reactions in the form of urticaria, pain in the back, lower abdomen, and joint pain.
Sometimes adverse effects develop that require examination by a gynecologist. If a woman experiences a delay in her menstrual cycle after installing an IUD, she needs to undergo an urgent examination. When diagnosing pregnancy, it is necessary, first of all, to determine whether it is uterine or ectopic.
Subsequent clinical examination of women using IUDs involves visiting a gynecologist twice a year with microscopy of smears from the vagina, cervical canal and urethra, ultrasound of the uterus and ovaries.
How to remove a spiral
The intrauterine device is removed at the request of the patient, as well as due to the expiration of the period of use (when replacing an old IUD with a new one, there is no need to take a break), if complications develop. The spirals are removed by pulling the “antennae”. If the “antennae” are missing or broken (if the period of use has been exceeded), it is recommended to carry out the procedure in a hospital setting. First, gynecologists consider it advisable to clarify the presence and location of the contraceptive in the uterine cavity using ultrasound.
Removal of the spiral is carried out after dilatation of the cervical canal under subsequent ultrasound control. Its removal is quick and usually almost painless. The gynecologist fixes the cervix, having previously treated the external genitalia. The doctor grabs the “antennae” with a forceps, then gently pulls them and removes the IUD.
Reviews from women
- Can a man feel the IUD during sex? If the coil is installed correctly, your partner will not feel it. The IUD is located in the uterine cavity, and only the antennae stick out into the vagina from the outside. No matter how deeply the penis penetrates into the vagina, according to men’s reviews, they do not feel these thin threads.
- What to do if your partner feels the spiral tendrils inside? Most likely, when installing the IUD, the gynecologist left the threads too long, and this is what the man feels during sex. The problem can be solved simply - the doctor will carefully trim the antennae of the spiral, and there will be no more unpleasant sensations.
- When can you have sex after installing the IUD? It is best to wait at least 7 days - the IUD should fit comfortably in the cavity, and at the end of the week you should visit a gynecologist and check the position of the spiral with a control ultrasound.
- When is intimacy allowed after removal of the IUD? Sex is allowed 5-7 days after the IUD is removed. An earlier resumption of intimate relationships, according to many gynecologists, risks injury and inflammation of the genitals.
- Can the IUD fall out during intimacy? It may fall out for other reasons not related to sex (for example, due to improper installation). It seems that the spiral has fallen out - consult a doctor, because... even incomplete prolapse of the intrauterine contraceptive makes protection against unwanted pregnancy ineffective.
- Is it painful to have sex with an IUD? Women's reviews are mixed? The product does not interfere with intimate life, and neither the woman nor the man should experience any unpleasant sensations. Pain during sex may indicate the development of complications or other gynecological problems in the pelvis. You should see a gynecologist and do an ultrasound.
- Does the IUD protect against sexually transmitted infections? No.
- According to women's reviews, does the spiral affect their sex drive? Non-hormonal IUDs do not affect libido or the ability to experience orgasms. Some women who have installed a hormonal IUD note in their reviews a slight decrease in the desire to copulate, others do not notice any significant changes and want to have sex the same way as before or even more often. Experts can explain the latter circumstance by the disappearance of fear of an unplanned pregnancy.
Conclusions about this method of contraception.
Which intrauterine device is considered the best protection against pregnancy? It is impossible to answer this question, since there are simply no universal IUDs that suit every woman. The gynecologist must select a specific spiral on an individual basis, based on the characteristics of the patient’s body, the presence or absence of established contraindications and long-term plans for future childbearing.
Spiral price
| Service | Price |
| Buy Mirena spiral | 19 500 |
| Buy a spiral with gold | 10 500 |
| Installation of the spiral | 5 000 |
| Place a spiral (Mirena) | 6 000 |
| Buy and supply a spiral (gold) | 15 000 |
| Buy and insert a spiral (Mirena) | 25 000 |
| Removing the spiral | 3 500 |
| Removing the spiral (complicated) | 5 500 |
Where to buy, install or remove a spiral
Moscow, Kutuzovsky Prospekt, building 35. Telephone, near the metro station and the Kutuzovskaya MCC.
Choose the best spiral:
| Mirena hormonal | "GoldLily" golden |
This service may have contraindications; before installing or removing the IUD, consult a specialist. All prices indicated on the website are provided as reference information and are not a public offer as defined by the provisions of Article 437 of the Civil Code of the Russian Federation and can be changed at any time without prior warning. For detailed information about the cost of services, please contact the reception staff by phone during clinic business hours.
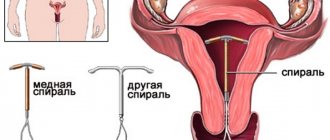
Types of spirals
Today, there are about fifty varieties of intrauterine devices, and which one is suitable for installation is determined by the gynecologist after a thorough examination of the patient.
Among the most popular are S-shaped, T-shaped and ring-shaped. Silver, gold and copper are usually used to produce spirals.
Before the procedure, the doctor prescribes the following examinations: tests for the presence of sexually transmitted infections, ultrasound of the pelvic organs, diagnostics using a colposcope, OAM, blood for hepatitis, HIV, RV, smear from the cervical cavity, smear from the vaginal cavity.
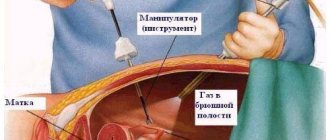
Consequences and complications
Expulsion is sometimes accompanied by mild discomfort , less often by severe pain in the suprapubic or periumbilical region of the pelvis. In a normal situation, the pain manifests itself for a short time, otherwise, a visit to a gynecologist is required for further examination.
Partial displacement of the contraceptive can lead to its migration into the fallopian tube , which leads to perforation of the walls of the fallopian tubes. The development of this pathology can be assumed based on the characteristic symptoms :
- persistent pain in the lower abdomen and the appearance of signs of intra-abdominal bleeding;
- weaknesses;
- tachycardia;
- blanching of mucous membranes;
- drop in blood pressure;
- “Volka-stand up ” syndrome - the patient strives to take a “sitting” position to reduce pain.
There is only a surgical way to resolve the pathology. Cervical perforation is mainly a consequence of contraceptive displacement. Therefore, a specialist, during a special examination of the genital organs, can detect an intrauterine device in the area of one of the corners of the vaginal vault. If a perforation of the cervical canal itself is detected, immediate insertion of the IUD into the uterus is prescribed for its further removal.
Asymptomatic drug rejection, coupled with the lack of other methods of birth control, leads to unplanned pregnancy .
Signs of a displaced IUD are painful sensations during sexual intercourse for the woman’s partner.
Also find out what a negative MAP test means, interpretation, results, how a spermogram differs from a MAP test
Why do you need labiaplasty - laser or surgical - written in detail here
6 facts about fetal hypoxia, consequences for the child, the nervous system, what it threatens:
Benefits of having an IUD
Installing an IUD inside the uterus allows you to avoid conception for five to ten years, but it is worth noting that there is no need to visit a gynecologist more often than normal. The device is an ideal and reliable contraceptive that changes the endometrium of the uterus, preventing the attachment of a fertilized egg, in other words, the fertilized egg is simply rejected by the uterus. This type of contraceptive is non-hormonal, therefore, it does not cause weight gain and does not impair the sexual function and sensitivity of women. But hormonal-type coils will eliminate the growth of the endometrium and suppress pain during the menstrual cycle.
After the expiration date of the spiral, it is removed, and if desired, the patient can have a new one installed.
Pros and cons of installing an IUD
It is important for women who want to install an IUD to understand the advantages and disadvantages of this type of contraception. Main advantages:
- Ease of use: once you install the coil, you no longer have to think about methods of protection for the entire life of its service. There is no danger of forgetting to take (use) the drug in a timely manner, as happens, for example, with oral or local contraceptives.
- The IUD does not dull sensations during intimacy.
The intrauterine device does not interfere with sexual activity, and there should not be any unpleasant sensations. Pain during sex or outside of intimacy may indicate the development of complications (partial prolapse of the IUD, damage to the uterus). You should see a doctor to find out the cause of this condition.
obstetrician-gynecologist Ekaterina Osennyaya
https://summerinside.ru/seks-posle-ustanovki-vnutrimatochnoy-spirali-10-intimnyih-voprosov-vrachu/
- This method of contraception is relatively inexpensive, because the duration of use of the IUD ranges from 3 to 10 years.
- Non-hormonal IUDs have no contraindications such as smoking and breastfeeding.
- If the IUD contains hormones, then it not only prevents fertilization, but also controls the volume and regularity of menstruation, and prevents ectopic pregnancy.
The disadvantages include:
- inability to install an IUD on your own;
- it is unacceptable to install it in nulliparous women;
- Being a contraceptive, the intrauterine device is not a barrier to sexually transmitted infections.
Side effects
Known side effects include pain for one week and an increase in the duration of menstruation. It is worth noting that during menstruation there will be an increase in the volume of discharge (usually within the first five days after installation of the IUD).
Best materials of the month
- Coronaviruses: COVID-19
- Antibiotics for the prevention and treatment of COVID-19: how effective are they?
- The most common "office" diseases
- Does vodka kill coronavirus?
- How to stay alive on our roads?
It is normal to have some bleeding within two weeks of having a contraceptive device inserted. If bleeding along with pain is observed for more than 14 days, the IUD is removed - the body does not accept such a contraceptive and can provoke a number of unpleasant consequences, for example, anemia.
Reasons for appearance
The main reasons for the expulsion of the IUD are the discrepancy between its shape and size , the distance from the cervix to the bottom of the uterine cavity and its volume.
As a result, painful sensations and strong muscle contractions are observed, which lead to the displacement of the contraceptive outside the organ - into the cervical canal, and from there into the vagina. A similar situation results from the inability of the isthmus muscles to retain the drug in the cavity. In addition to individual physiological etiology, the following are equally sources of expulsion:
- use of an IUD by women with a deformed or open cervix ;
- excessive mechanical loads ;
- Incorrect installation of the spiral.
Installing an IUD after pregnancy
An intrauterine device can be installed one and a half months after birth, provided that no postpartum complications have been detected. If a caesarean section was performed, installation of the IUD is allowed no earlier than six months later. This device does not have any effect on the production of breast milk and the development of the child during breastfeeding.
After an abortion, the installation of an IUD is allowed after the end of the first menstrual cycle after the abortion procedure. It is important to understand that pregnancy can occur only a year after the IUD is removed; this factor must be taken into account before installation.
More fresh and relevant information about health on our Telegram channel. Subscribe: https://t.me/foodandhealthru
We will be grateful if you use the buttons:
Types of installation
Today there are several dozen types of intrauterine devices. They are made from different materials. Therefore the installation could be:
- Hormone-containing protective agents.
- Copper.
- Golden.
- With silver.
Copper IUDs are believed to have additional contraceptive effects. That's why they cost more. Gold ones are expensive. Gynecologists do not recommend installing hormonal hormones, especially if the woman’s levels of hormonal substances are normal.
The following brands of intrauterine devices are popular on the Russian market:
- Mirena (contains hormones, releases levonorgestrel (an analogue of progesterone), which prevents pregnancy).
- Nova T.
- Multiload.
Depending on the purpose, the installation can be:
- To prevent unwanted pregnancy.
- For the treatment of gynecological diseases.
Removing the spiral
You can remove the spiral at any time during its service life. Typically, its removal, as well as its introduction, occurs during menstruation. In this case, the most favorable will be the first and last days, when bleeding is least abundant. However, these are general guidelines to make IUD removal easier. If necessary, you can remove the spiral on any other day. If its removal is due to the end of its service life, then the next one can be introduced immediately. In addition to the expiration of the spiral’s shelf life, there are other indications for removal:
- a woman's desire to become pregnant;
- displacement or prolapse of the IUD;
- the onset of pregnancy (both uterine and ectopic);
- menopause;
- pain, bleeding, inflammation and swelling caused by the insertion of the IUD.
How the extraction process works:
- The genitals are treated with an antiseptic.
- A gynecological speculum is inserted.
- The tendrils of the IUD are grabbed with tweezers and pulled out of the uterus.
The procedure for removing the coil is absolutely painless and takes a few minutes.
The procedure lasts several minutes and is absolutely painless. During the extraction process, the spiral tendrils may be torn off. In such a situation, the doctor removes it with a medical hook. It often happens that the IUD grows into the wall of the uterus (as a rule, this happens when the IUD has been used longer than expected). In such cases, curettage is performed using anesthesia. Sometimes the spiral grows into the uterus in such a way that its removal becomes possible only through the abdominal cavity under general anesthesia. To avoid this, it is necessary to monitor the service life of the IUD and not miss its end.
Contraindications for IUD insertion
Like any other manipulation, the installation of an IUD has its limitations. Absolute contraindications (i.e., under no circumstances should the procedure be performed) include:
Relative (at the discretion of the doctor) contraindications:
- algomenorrhea (excessively painful menstruation);
- polyposis, endometrial hyperplasia;
- multiple fibroids;
- abnormalities of the uterus (bicornuate, saddle-shaped);
- severe anemia;
- severe allergy (especially to copper);
- subacute endocarditis;
However, before drawing your conclusions, you need to consult with a gynecologist at SM-Clinic.