Modern gynecology offers an impressive list of methods and means of contraception. The intrauterine device is the most effective way to prevent unplanned conception. The absence of side effects and consequences largely depends on what day of menstruation the IUD is placed.
The effect of the IUD on the menstrual cycle
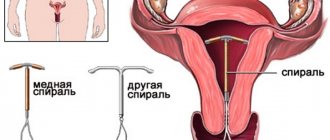
The nature of the influence of the spiral on the cycle depends on the type of product. Modern contraceptives are made of plastic and metal in the shape of the letters “T”, “S”. The protection effect is achieved due to the following factors:
- thickening of the secretion of the cervical canal, which makes it difficult for sperm to move;
- prevention of endometrial proliferation and implantation of a fertilized female germ cell;
- increased contractile activity of the tubes, ensuring the passage of the immature fertilized egg.
The spiral has a direct effect on the organs of the reproductive system. The influence of the product on the cycle differs from individual to individual. Many women note a decrease in the intensity of bleeding during menstruation. During the adaptation period, acyclic spotting may appear.
On what day of the cycle is the IUD placed?
Before installing the device, the gynecologist prescribes the necessary tests for the woman to exclude:
- pregnancy;
- infections and inflammation.
Often patients are interested in when it is preferable to insert a spiral. The product must be placed in the uterine cavity by inserting it into the cervical canal. This area is anatomically narrow. Sometimes, after insertion of the IUD, a discharge like menstruation is observed, which may be a symptom of injury.
Damage to the mucous membrane of the cervical canal is dangerous due to the development of the inflammatory process and the occurrence of erosion. It is known that trauma to the cervix can complicate subsequent labor.
It is recommended to insert the IUD during menstruation for the following reasons:
- opening of the cervix;
- soft texture of fabrics;
- installation accuracy and painlessness.
If you insert the IUD during your period, the adaptation is easy. It is advisable to install the product towards the end of the menstrual period due to mild bleeding and slight narrowing of the cervical canal.
Is it possible to get an IUD without menstruation?
You can insert the IUD without menstruation if pregnancy is ruled out. The doctor can prescribe a contraceptive without menstruation after childbirth. If the IUD has a hormonal effect, it must be placed on the 7th day of the cycle. Most women have stopped menstruating by this time, which can cause pain during the procedure. Anesthetics are used to eliminate pain during IUD insertion.
How to install a spiral
To prevent conception, if desired, a woman can install an intrauterine device. The procedure must be carried out by a medical specialist with the necessary qualifications.
Note! Installation of the spiral into the uterine cavity is carried out only after the patient has undergone a complete examination. Diagnostics is necessary to identify contraindications and possible risks of side effects.
Stages of IUD insertion:
- two-manual gynecological examination on a chair to determine the location of organs and the intended installation location of the spiral;
- antiseptic treatment of the skin and mucous membrane of the external genitalia;
- insertion of a gynecological speculum (to display the external uterine opening);
- using a clamp, the upper uterine lip is grabbed and pulled back;
- insertion of a probe directly to the fundus of the uterus to measure the length of the uterine cavity;
- removing the spiral from the packaging;
- a spiral is inserted through the cervix in a special tube;
- after the IUD reaches the bottom of the organ, the tube is removed by pulling;
- trimming the antennae of the contraceptive device;
- removal of gynecological instruments.
It is very important that the spiral is installed correctly
This procedure may cause discomfort and minor pain if all the doctor’s manipulations are performed correctly. The mini-operation takes about 5 minutes, after which the woman can safely go home.
What are the contraindications for installation?
The gynecological procedure for inserting an IUD should not be performed if the diagnosis reveals that the woman has contraindications:
- acute stage of inflammatory and infectious diseases of the genitourinary system and genital organs;
- cancer of organs located in the pelvic area;
- any form and stage of STD;
- large tumor formations;
- pregnancy;
- allergy to the material from which the IUD was made;
- abnormal deviations that prevent the correct installation of the contraceptive.
Neglecting contraindications can lead to serious consequences, including oncological processes.
Menstruation after installation of the IUD
Menstruation usually begins at the scheduled time after installation of the intrauterine device. However, the possibility of delayed menstruation cannot be ruled out.
First menstruation after installation of the IUD
The first menstruation during the adaptation period may differ in time of onset, intensity and duration. The nature of menstruation depends on the individual characteristics of the patient.
How long does your period last after installing the IUD?
It is possible to change the duration of the cycle towards its increase. It is known that the normal duration of critical days is up to 7 days. During the first cycles after installing the IUD, periods sometimes take a long time. In this case, there should be no pronounced changes in the general condition of the woman.
For pain of moderate intensity, you can resort to taking antispasmodics and painkillers. Cramping pain and increased discharge during menstruation may indicate the development of an inflammatory process, rejection of the product, or trauma to the uterine tissue. These symptoms require immediate removal of the IUD.
These hygiene products increase the risk of infection and interfere with normal adaptation to the intrauterine contraceptive device.
After the spiral, heavy periods
Often the first periods after insertion of the IUD are heavy. This is due to the irritating effect of the product on the inner layer of the uterus and a change in the characteristics of the secretion of the cervical canal.
If you experience severe pain and weakness, you should seek medical help.
IUD discharge between periods
Acyclic spotting may occur within 3 cycles after insertion of the IUD. Discharge between cycles occurs due to the adaptation of the organs of the reproductive system to a foreign body. The absence of pain is essential.
Delayed menstruation with IUD
A slight delay in menstruation with the IUD in some women is due to the following reasons:
- suffered stress;
- adaptation to a foreign body in the uterus;
- possible hormonal changes.
Changes in cycle length should not exceed 3 weeks. Otherwise, it is recommended to consult a gynecologist. Delays of minor duration may occur over several cycles, which is considered normal.
A prolonged absence of menstruation when using the IUD requires the exclusion of pregnancy. Before inserting an IUD, you should consider the need to use additional contraception for 2-3 weeks after installation of the product. If you use the IUD when your period is late, and the test is negative, pregnancy is unlikely.
How to remove the IUD in women
Removing the IUD involves several steps.
Preparatory activities
A week before the expected procedure, if you do not want to get pregnant, it is recommended to avoid unprotected sexual intercourse. This is due to the persistence of sperm activity for several days, and the possibility of ovulation occurring immediately after pulling out the contraceptive. In this way, a productive meeting between the sperm and the egg can occur.
It is recommended to remove the intrauterine device during menstruation. This circumstance will facilitate and soften the process. The optimal time would be 3–4 days after the start of menstruation, when the discharge is no longer profuse. However, this condition is not necessary; the IUD can be removed on any day of the cycle; you cannot wait for the onset of menstruation if you have constant bothersome symptoms.
The procedure begins with a routine examination in a gynecological chair. The gynecologist examines the position of the uterus by palpating the abdominal cavity with one hand and holding fingers in the vagina with the other. The doctor then locates the IUD threads (tendrils). The last point at the preparation stage is the introduction of an expander to stabilize the uterus and treatment of its cavity with an antiseptic.
Is it painful to remove the coil?
All owners of an intrauterine contraceptive, on the eve of the procedure for its removal, are concerned about the question of whether it hurts. Installing an intrauterine device is a more labor-intensive and time-consuming process compared to removing it. In most cases, there is no need for anesthesia when removing an IUD.
Of course, every woman’s body is individual, and so is her pain threshold. If desired, a woman can take a mild analgesic before the procedure.
Local anesthesia in the form of a paracervical blockade or lidocaine spray is possible with a low pain threshold or with panic fear before the procedure.
It happens that the antennae of the spiral come off or are lost in the uterine cavity, in which case the procedure may require hysteroscopy (visual examination of the uterine cavity using optical equipment) under anesthesia.
The reason for general anesthesia is the impossibility of performing removal manipulations through the cervical canal in the cervix. In such a situation, you need to remove the spiral through the abdominal cavity using laparoscopic forceps.
Removing the spiral
The gynecologist places the IUD for a period of 5-7 years. The need to remove the IUD is associated with the following risks:
- ingrowth of the product into the uterine mucosa;
- development of the inflammatory process;
- reproductive dysfunction.
The period of use of the spiral depends on its type, the presence of possible indications and the desire of the woman.
When to remove the IUD - after or before menstruation
It is recommended to insert and remove the IUD during menstruation. This is due to the physiological characteristics of the cervix during menstruation. It is advisable to remove the IUD in the last days of menstruation
Is it possible to remove the IUD without menstruation?
Removal of the IUD without menstruation is carried out if indicated. When a doctor places an IUD, he informs the patient about possible adverse reactions of the body to a foreign body. In such cases, you can remove the IUD without menstruation.
When does menstruation begin after insertion of an IUD?
If manipulations are carried out in the last days of menstruation, then the next cycle will not be disrupted and your period will come on time. But there are also nuances that need to be taken into account.
When an IUD from pregnancy is installed, there is bleeding for 1 day. This is spotting. Although in exceptional cases critical days may recur, they last longer than usual - up to 14 days. If it’s even longer, this is a good reason to see a doctor to find out how long such discharge can last. Usually, after installing the IUD, the first periods come as scheduled, they are a little heavier, sometimes clots appear, and there is pain.
In the absence of undesirable consequences, the second menstruation does not differ from normal. If your periods are too heavy, cause pain and last a long time, you may even need to remove the IUD.
Periods after IUD removal
Typically, menstruation occurs as scheduled after the IUD is removed. A recovery period is observed for several months, which is characterized by delayed menstruation.
Heavy periods after IUD removal
In most cases, the next menstruation occurs within 1-1.5 months. Postponement of critical days may be associated with emergency removal of the device.
Heavy discharge occurs due to hormonal changes, since the IUD prevented adequate proliferation of the inner layer of the uterus and maturation of eggs. The intrauterine contraceptive also indirectly affects the functioning of the ovaries.
The intensity of menstruation depends on the presence of the following unfavorable factors:
- inflammation;
- damage to the uterine mucosa.
Removing a contraceptive is easier than inserting it. Pain and discharge may indicate the presence of parts of the IUD in the uterine cavity after its removal.
Restoration of the menstrual cycle
After removal of the contraceptive, scanty bleeding is often observed due to prolonged suppression of ovarian function and the development of the endometrium. The normal period should be restored within 3 cycles. If, after this period, menstruation resembles spotting, an examination by a gynecologist is necessary.
In the absence of complications and side effects, periods should return to their previous levels. Sometimes the long-term effect of a contraceptive on the reproductive system changes the nature of menstruation.
Possible side effects and complications
Since the intrauterine contraceptive is a foreign body, complications and possible side effects cannot be excluded:
- pain syndrome in nulliparous or emotional women when choosing the wrong product size;
- loss of the device in case of violation of the insertion technique;
- heavy menstruation;
- inflammatory processes due to untreated infections, activation of opportunistic microflora;
- bleeding and anemia;
- the occurrence of fibroids;
- ectopic and uterine pregnancy;
- pain during sexual intercourse;
- lack of orgasm;
- puncture (perforation) of the wall of a muscular organ;
- ingrowth of the product into the tissue;
- copper intolerance.
When to see a doctor urgently
Complications after the introduction of intrauterine contraceptives are observed in women who have had extrogenital diseases in the past. The following pathological conditions most often develop:
- bleeding;
- pain syndrome;
- prolapse of the IUD;
- inflammatory diseases of the genital organs.
Immediate consultation with our specialists is required in cases of fever, heavy discharge, or severe pain after insertion of the IUD.
For the gynecologists of our clinic, a woman’s health comes first, so we are always happy to help you solve such an important issue as contraception. Trust us and we will make every effort to ensure that the result does not disappoint you.
How to place an intrauterine device
Before choosing one or another contraceptive, you need to weigh the pros and cons. The choice of contraceptives is quite large. The advantages of the intrauterine device include the fact that it acts from several positions at once to prevent pregnancy:
- prevents the penetration of sperm to the egg, interferes with fertilization;
- makes it impossible for the egg to attach to the walls of the uterus;
- some IUDs contain a small amount of hormones, it is negligible to have a strong effect on a woman’s hormonal background, as happens with oral hormonal contraception or the use of injections and implants, but at the same time it significantly interferes with pregnancy (for example, it increases the amount of mucus in the cervix, preventing sperm from penetrating inside);
- is established for a long period (from 3 to 7 years for different types), there is no need to visit the doctor every month or worry about taking a pill at the wrong time;
- does not require additional contraception (such as spermicidal suppositories, vaginal diaphragm and some other types of protection against pregnancy), the reliability of the IUD is from 98% to 99.9% (for IUDs with hormones);
The Mirena intrauterine hormonal system has high protection against unwanted pregnancy, 99.9%
Where can the procedure be performed?
An IUD can only be inserted in a clinic setting. The procedure should only be performed by a qualified obstetrician-gynecologist.
IUD installation in clinics is free. If you go to a paid clinic, the procedure will cost you from 250 to 3000 rubles.
Indications and contraindications for IUD installation
The spiral does not require any special indications for use. The main thing is protection from unwanted pregnancy, when taking hormonal drugs is impossible or undesirable for certain reasons. A hormonal IUD can be prescribed for medicinal purposes (for example, for heavy periods with an unknown cause, for endometrial hyperplasia - the inner layer of the uterus).
There may be several contraindications:
- inflammatory processes of the uterus, ovaries, vagina;
- pregnancy;
- pathological changes in the cervix;
- history of ectopic pregnancy;
- malignant and benign changes in the reproductive organs;
- diseases of the circulatory system;
- age (as a rule, young nulliparous girls are not given a spiral).
Video: difference between hormonal IUDs and other types
Is preliminary preparation necessary?
Before the doctor begins installing the IUD, the woman needs to undergo several important procedures, collect a brief medical history and, if necessary, undergo treatment. Common diagnostic procedures prescribed by a gynecologist include:
- Ultrasound of the organs of the reproductive system (makes it possible to verify that the woman is not pregnant, and also to identify contraindications to the installation of the IUD in the form of neoplasms or changes in the structure of organs);
Ultrasound of the pelvic organs allows you to verify the absence of pregnancy and pathologies in the structure of the organs of the reproductive system
If, based on the results of the examination, the doctor has doubts about the woman’s health, the procedure is postponed until the doctor is sure that everything is in order.
At what period of the cycle is an IUD inserted?
It will not be possible to insert an IUD on any day. This procedure is always tied to the beginning of the menstrual cycle (usually it is carried out on the 4th–5th day of the cycle). And there are two good reasons for this:
- the onset of menstruation is one of the signs of absence of pregnancy;
- From the first to the fifth day of menstruation, the cervix is as open as possible, which facilitates the insertion of the IUD.
The first day of the menstrual cycle is considered the first day of menstruation
There are two periods when a woman can get the IUD, regardless of the start of her cycle:
- Immediately after the abortion. At this moment, the cervical canal is open as much as possible, the woman is under anesthesia, pregnancy is 100% excluded.
- After childbirth, when the cycle has not yet recovered. After spontaneous childbirth, the IUD is placed after the end of lochia (postpartum discharge) closer to the third month after the joyful event. But after a caesarean section you will have to wait six months: the scar on the uterus should heal well.
How is the procedure performed?
Installation of an IUD does not require hospitalization. The manipulation is carried out on an outpatient basis in the treatment room. The whole procedure takes about 10 minutes:
- The woman is positioned in a gynecological chair, as during a routine examination.
- The doctor installs a vaginal dilator with a speculum and treats the cervix with an anesthetic. If necessary, it is possible to give an analgesic injection, usually lidocaine.
- The doctor then measures the size of the uterus with a special instrument to compare it with the size of the IUD.
- The doctor administers the contraceptive itself, opening the sterile package with the spiral in the presence of the patient.
- All spirals are equipped with control threads. The doctor trims them, leaving about 2 cm protruding from the uterus. When there is no longer any need for further use of the IUD, the doctor will remove the IUD by pulling these particular antennae.
- To reduce discomfort after installation, the doctor may give the patient a pain-relieving injection.
Video: technique for installing an intrauterine device
What does a woman feel during installation of an IUD?
During installation of the spiral, a woman may experience slight discomfort. The sensation is similar to menstrual pain. They can last for several days, but no more than a week. This is normal.
The first and subsequent 2-3 periods after installation may be painful and heavier than usual. At this time, you need to be especially vigilant, as spontaneous release of the contraceptive is possible.
9-12 weeks after installation of the IUD, it is recommended to undergo a control ultrasound to ensure the correct placement of the contraceptive. In the future, such ultrasounds must be performed once every six months.
Side effects and complications
Like any medical intervention, the presence of a foreign body inside an organ cavity is fraught with complications and may have side effects.
When to install the spiral
When is it better to insert an IUD - before or after menstruation? It is recommended to carry out this procedure on the 3rd or 5th day of the menstrual cycle.
During this period, the uterine cervix is slightly open so that the manipulation is the least traumatic and painless. Menstruation is a sign of absence of pregnancy, which means it is safe to insert an IUD, and there are no obstacles to this.
It’s probably not worth saying that an IUD should only be installed in a hospital setting. When a contraceptive is installed after childbirth, you should wait a couple of months. After an abortion, an IUD is inserted immediately. After cesarean - six months later.
Anesthesia is not used during manipulation; there is pain, but it is quite tolerable. Using a special device, the gynecologist inserts a contraceptive into the uterus. Be sure to check the position and shorten the antennae. Thanks to the antennae, a woman can independently determine how the IUD is located.
At the end of the procedure, there may be pain and slight discharge. For a couple of months after installation, periods are heavy and painful, during which time the IUD can spontaneously expel. You should take care for a week, do not expose yourself to physical activity, and do not take hot baths. You should abstain from sex. Laxatives are contraindicated.
After 10 days you need to come for a scheduled examination. If all is well, the next appearance is in a month or three. After menstruation, self-monitoring is carried out.
When and how to remove an IUD
The spiral can be removed at any time, both at the request of the woman and as prescribed by the doctor. If the woman wishes, the removal procedure is carried out during the same period of the cycle as the installation. There are indications for emergency removal:
- inflammatory processes and infectious diseases of the pelvic organs;
- displacement of the spiral, disappearance of the antennae or change in their length;
- uterine bleeding;
- absence of menstruation.
The removal of the uterine contraceptive is carried out by a doctor. Before the procedure, the woman undergoes the same tests as before installing the IUD.
The beginning of the removal procedure is absolutely identical to the installation. And the removal itself is carried out using antennae; the doctor pulls out the spiral by pulling the control threads.
Feedback from women about installing and removing the IUD
I gave birth and two months later I got an IUD, without menstruation, it was very unpleasant and even painful. Almost immediately, discharge and viscous mucus appeared. A month later I went to the residential complex, where they calmed me down that this could happen. But it turned out that the spiral was placed incorrectly! The discharge continued for six months, then a nagging pain appeared in the area of the right ovary, and a day later the pain began to ache in the lower back on the same side. I went to the residential complex again, but for a fee. The right ovary was enlarged, so she sent me for an ultrasound to see how the coil was positioned and to check the ovary. The ultrasound scared me So. The spiral has grown into the back wall of the uterus; remove it only under anesthesia! I was very stressed then. They sent me to the hospital and there they removed it for me in one minute, I didn’t even believe that it was all over. Verdict - arrived just in time! Girls, don’t delay, it will only get worse later, it’s better not to rely on Maybe in this matter.
Daria
https://www.woman.ru/health/woman-health/thread/4035858/6/
I was removing the Mirena spiral, which didn’t even have a mustache visible. Until today, I tried for a year to have it removed from different doctors - nothing worked, it was painful and I stopped the process. After the last ultrasound, they told me to endure it, but to remove it - the fibroid node had grown greatly. I was shaking for three days and couldn’t sleep at night (I remembered how the previous Mirena was taken off). There are tears in the morning, the doctor is in panic. As a result, the doctor suggested using an anesthetic spray, and after 5-8 minutes she began to pull it out. She says, take a deep breath, don’t breathe for 2-3 seconds (at this time she was dragging, it was a little painful, but tolerable and quickly), then she told her to catch her breath, but calmly, so that her head wouldn’t spin, as we usually breathe). Take another deep breath, 2 seconds and pull it out. I'm an expert at screwing myself up, but believe me, this method is practically painless.
Alyona
https://www.woman.ru/health/woman-health/thread/4035858/6/
After my first unsuccessful pregnancy, I decided to get an IUD. It stayed with me for a long time, later it cauterized the erosion, and my antennae were singed. When it was time to shoot, we filmed with a crochet hook. It’s not very painful, just an unpleasant and nagging pain. The spiral fits me very well, it stood for a long time, without any consequences. It performed its function well. Before planning, I removed the spiral and took a simple cheap one with silver ions from our Russian production. After removing the IUD, 6-8 months later I became pregnant.
Maria Pavlova
https://flap.rf/%D0%9C%D0%B5%D0%B4%D0%B8%D1%86%D0%B8%D0%BD%D0%B0/%D0%92%D0%BD% D1%83%D1%82%D1%80%D0%B8%D0%BC%D0%B0%D1%82%D0%BE%D1%87%D0%BD%D0%B0%D1%8F_%D1% 81%D0%BF%D0%B8%D1%80%D0%B0%D0%BB%D1%8C_%28%D0%92%D0%9C%D0%A1%29
and I have Mirena. it doesn't hurt. I haven't taken it out yet. menstruation became heavier, but not painful. and last a week, instead of the usual 3-4 days. There is still some daubing in between. with PA it is not felt and the husband does not feel the mustache. Overall I'm satisfied. Before that, I drank OK for 10 years. The gynecologist was categorical about them and said that’s enough! the spiral is safer. In general, so far there are no special complaints
cat
https://www.woman.ru/health/woman-health/thread/3889824/
A wide selection of contraceptive methods allows a woman to decide on the most convenient way for her to plan the birth of a child. The IUD is the most common, budget-friendly and comfortable option for contraceptives. You just need to remember that following all the specialist’s recommendations is the key to women’s health.
The issue of contraception is relevant for every woman of childbearing age. Today there are many effective ways to avoid unwanted pregnancy, among which intrauterine contraceptives are especially popular. When an IUD is placed, before or after menstruation, many girls turn to doctors with this question.
Intrauterine contraceptives have been used since the mid-20s of the last century. Then they were a ring made of an alloy of brass and bronze, to which a small amount of copper was added. In 1960, a safer product made from elastic material appeared.
Modern spirals have different shapes, some of them contain hormonal drugs. The contraceptive effect is achieved by releasing a small amount into the cavity of the reproductive organ. In addition, the spiral has a mechanical effect on the inner lining of the uterus, preventing the attachment of the egg after fertilization.
The spiral significantly complicates the advancement of male reproductive cells and weakens them, which does not allow pregnancy to occur.
It is recommended to insert the IUD between the 3rd and 5th day of the new menstrual cycle.
During this time, the cervix is slightly open so that the procedure for introducing a contraceptive is the least traumatic and easy to implement. The onset of menstruation is one of the signs that a woman is not pregnant, so it is at this time that it is preferable to install the IUD.
Question: When is the best time to remove the coil?
The site provides reference information for informational purposes only. Diagnosis and treatment of diseases must be carried out under the supervision of a specialist. All drugs have contraindications. Consultation with a specialist is required!
Hello, I have had the Multiloud coil for 2 years now, and now we want a second child. When is it better to take it out (during menstruation or something?)), and after what period of time will it be possible to conceive a second child?
It is recommended to remove the IUD on days 4-8 of the menstrual cycle. You can plan to conceive a child 3 months after the procedure.
I have already had the 3rd spiral for 4.5 years. I removed the previous 2 during menstruation, but now the doctor told me that it doesn’t matter. This procedure is quite painful judging by my experience. Tell me what is the best thing to do? And how can this procedure be numbed?
It is better to remove the IUD during menstruation; during this period, removal occurs faster and with fewer complications. If necessary, general anesthesia can be used; you should consult with your gynecologist about the possibility of using it in your case.
Hello, please tell me, I want to remove the spiral. The doctor told me that before this I need to do some kind of analysis, and then immediately remove the IUD. She also told me that the IUD is taken out the day before your period. Tell me, what kind of test is this, is it painful to take it... and is it generally painful to remove the IUD?
It is recommended to take a vaginal smear; removing the IUD is no more painful than putting it in, so there is no need to worry so much.
Please tell me, is it possible to remove the IUD the day before your period? The thing is. That when I told her that I read that the IUD is taken out during menstruation. she said that before removing the IUD they would still take a test from me and therefore the IUD should be removed one day before my period. This is true? Is it necessary to do an ultrasound before removing the IUD? She took a smear from me during the visit.
The easiest way to remove the IUD is at the end of the menstrual cycle. However, your doctor may set a different time frame for removing the IUD. If necessary, ultrasound diagnostics are performed before removing the coil.
I have an IUD, I want to have a second child with my husband, I read in your answers that after removing the IUD you need to wait 3 months before conceiving a child. How can you protect yourself during these three months, except for a condom? and what happens if pregnancy occurs before 3 months?
If you are planning a pregnancy in 3 months, then the use of hormonal contraceptives is not advisable. The most recommended method in such cases is the barrier method (condoms). After removal of the IUD, the interval until pregnancy occurs is necessary for the pregnancy to proceed most favorably. If pregnancy occurs earlier, nothing terrible will happen, but this interval is needed to restore the physiological state of the uterine cavity. You can learn more about this from the section of our website: Intrauterine device
Modern gynecology offers an impressive list of methods and means of contraception. The intrauterine device is the most effective way to prevent unplanned conception. The absence of side effects and consequences largely depends on what day of menstruation the IUD is placed.
IUD installation process
Before installing an intrauterine device, an examination should be scheduled to exclude the presence of infections and pathologies associated with the reproductive organs. The standard list of diagnostic procedures looks like this:
- smears of the cervix and vagina;
- tests for syphilis, hepatitis and HIV;
- colposcopy;
- general urine test;
- tests that detect sexually transmitted infections;
- ultrasound examination of the uterus.
An ultrasound is prescribed not only to make sure that a woman has no changes that would prevent the use of an intrauterine contraceptive. Its purpose is also to make sure that the woman is not pregnant at the time of installation of the IUD. To do this, you will have to do a test to determine the level of hCG.
Before inserting the IUD, it is recommended to abstain from sex for 7-10 days.
The installation procedure is carried out exclusively in a gynecological office under sterile conditions. The woman sits in a chair with her feet on the holders. Before inserting the IUD, the doctor treats the cervix and vagina with a disinfectant. Additionally, local anesthesia is performed. Usually a special gel is used for anesthesia, sometimes injections.
Contraindications for IUD insertion
The intrauterine device is a convenient and relatively inexpensive means of contraception. But, like many medications, it has contraindications, under which it cannot be used to protect against unwanted pregnancy. The main ones are listed below:
- cervical dysplasia;
- malignant and benign neoplasms in the reproductive organs;
- a woman has previously had an ectopic pregnancy;
- severe trauma to the cervix during childbirth;
- blood diseases.
For girls who have never given birth, doctors usually do not recommend the IUD. Other contraceptives are selected for them individually.
IUD after childbirth or abortion
After the birth of the baby, women try to take some “pause” before planning a new pregnancy. And this is understandable - the body needs to get stronger after pregnancy and childbirth, and the family needs to get used to new rules and routines.
It is believed that in the first months, while there are no periods and the young mother is breastfeeding, she cannot become pregnant. However, this is not the case, and very often a woman finds out that a little man has settled in her womb again when all the signs of pregnancy become apparent.
This is why it is very important for women who have recently given birth to use proper protection. And the optimal choice during this period is Mirena or another spiral.
It can be installed when the uterus reaches normal size. This occurs approximately 6-12 weeks after the birth of the child, although it is also practiced to install the IUD immediately after natural birth. If delivery occurred via cesarean section, the intrauterine device can be installed after 6 months.
According to many practicing doctors, with whom researchers from the United States also agree, positive results are obtained by inserting a device into the uterus immediately after an abortion, regardless of whether it was caused by natural causes (miscarriage) or performed surgically.
If a contraceptive is introduced into the uterus 15-20 minutes after surgery, this minimizes the possibility of an unwanted pregnancy. In addition, there is no need to use anesthetics again and dilate the cervix.
What are the features of installation after childbirth and abortion?
Women who have recently given birth or had an abortion, as a rule, do not want another pregnancy. In order to preserve sensations during sexual intercourse, but at the same time prevent unwanted conception, they strive to install an IUD.
Even more interesting:
The echo structure is not changed, what does this mean?
Tongue with pharyngitis photo
After childbirth, the IUD cannot be placed immediately, but after some time.
When the procedure can be performed after childbirth or a medical abortion, and whether it is possible to insert an IUD without menstruation - these are questions that often interest women. The menstrual cycle in this case does not play a big role if there are no contraindications. Regarding the past pregnancy, each case should be considered separately.
Advantages and disadvantages of the intrauterine device
The IUD is considered a reliable method of protection: its effectiveness reaches 95%. Many women note as a positive factor that you can live with the same device for up to 5 years, and in some cases longer. This saves time and money that would otherwise have to be spent on purchasing other contraceptives. In addition, intrauterine devices have other advantages:
- you do not need to strictly follow the dosage schedule, unlike birth control pills;
- allowed for use by women who are breastfeeding;
- Once removed from the uterus, you can quickly become pregnant.
Hormone-containing coils, for example, Mirena, not only prevent pregnancy, but also have an anti-inflammatory effect on the reproductive organs and prevent endometriosis. In addition, after installing the Mirena coil, periods become practically painless and shorter.
Despite all the positive aspects, using a spiral can sometimes have negative consequences. First of all, this is a restriction that applies to nulliparous girls. This is due to the fact that they have a small uterine cavity, as well as a too narrow cervical canal. Because of this, the procedure for placing a contraceptive is more complex and painful. In rare cases, it ends with perforation of the wall of the reproductive organ.
The spiral is suitable for women who have a regular sexual partner, since the risk of infectious diseases increases, especially in the first month after installing a contraceptive. A foreign body inside the uterus contributes to the rapid spread of infection. If not treated in a timely manner, the inflammation can result in infertility.
The use of an IUD is associated with regular visits to the gynecologist. First to install it, and then preferably every six months. In addition, the woman has to independently control the antennae, the ends of which are located in the vagina. This is necessary to make sure that the spiral does not fall out. To remove the contraceptive, you will have to go to the doctor again.
Who gets the spiral and how is it selected?
The gynecologist may decide on the possibility of installing an IUD for the purpose of intrauterine contraception if the following conditions are met:
- the woman has already given birth before;
- the patient is not currently pregnant;
- she is physiologically healthy, there are no absolute contraindications to this method of contraception;
- menstruation comes regularly, bleeding is moderate;
- a woman has one sexual partner; otherwise, you will still need a barrier method to prevent STI infection - the use of condoms.
The issue of nulliparous women is always considered more carefully and individually. Such patients are advised to use alternative methods of contraception. But if there is a reluctance to use them, there are no contraindications to the installation of an IUD and good physiological health, the installation of special spirals for nulliparous women is allowed.
Before installing an IUD, a woman always undergoes a thorough diagnosis: examination by a gynecologist, ultrasound of the uterus and pelvic organs, taking smears, taking standard tests (urine, blood), and sometimes consultations with highly specialized specialists. These measures are aimed at identifying hidden diseases that may cause complications after the installation of the IUD.
Only after confirmation of the possibility of using this method of contraception is the choice of the IUD itself made. This can only be done by a specialist who has familiarized himself with the results of previous examinations. Particular attention is paid to the shape and materials from which the IUD is made. For example, a T-shaped spiral is not suitable for all patients: if the uterus is located atypically or the organ is abnormally developed, the most suitable shape must be selected: umbrella, F-shaped, loop, etc.
It is important to decide on the metal from which the spiral will be made. Thus, silver and gold IUDs, which have an anti-inflammatory effect, have proven themselves well. This factor is especially important for patients who have a history of inflammatory gynecological diseases. However, such spirals are not suitable for women who are allergic to these metals.
Is it possible to remove the IUD myself?
Some women are interested in whether it is possible to remove the IUD without menstruation or on their own? Experts categorically do not recommend conducting experiments at home. To do this, you need to contact a gynecologist. The extraction procedure should be carried out when menstruation occurs (in the first days) under sterile conditions.
If you remove the IUD yourself, there is a high risk of damaging the genital mucosa and causing infection.
Removing the IUD by a gynecologist is a virtually painless procedure if there are no inflammatory processes. Before her, the doctor conducts an examination. If the spiral is intact, then pull it out by pulling the antennae. If there are no threads in the vagina or the contraceptive is destroyed, microsurgical intervention is used - hysteroscopy.
After removing the IUD from the uterus, the doctor takes a smear from it, which is sent to the laboratory for cytological examination. This procedure is followed in most cases, but is not mandatory.