Every woman treats various gynecological manipulations with special caution. Those who prevent unwanted pregnancy with the help of an IUD have a logical question about how to remove the IUD from the uterus. It is worth saying that this method of contraception is quite popular, especially among women who already have children.
If the device was installed for the first time, and the time for its removal has already approached, of course, it is worth asking how the IUD is pulled out of the uterus (a video of this procedure can be presented on specific resources), but it is not recommended to do this yourself. Therefore, we will consider in more detail when it is better to remove the IUD, and what difficulties you may encounter.
Deadlines
The duration of use of these contraceptives can vary in the range of 3-15 years.
Not everyone knows when the intrauterine device can be removed.
The period of use depends on what type of device is used, as well as on the material from which it is made:
- IUDs containing copper can be used for 3-5 years.
- IUDs based on silver, hormone-releasing – 5-7 years.
- IUDs made using gold – 10-15 years.
The intrauterine device must be removed if the following indications exist:
- Gynecological pathologies, including inflammatory processes, tumors, bleeding, pain.
- The onset of menopause.
- The onset of conception.
- Loss (expulsion) or displacement of the spiral.
- Switching to a different type of contraception.
- Pregnancy planning.
- End of service life.
If the patient is diagnosed with uterine fibroids, which have a small volume, installation of a gestagen IUD is not contraindicated. If the tumor begins to actively increase in size while using a contraceptive, the intrauterine device should be removed.
What is the process?
Removing the intrauterine device is a minor medical procedure. It is prohibited to remove contraception on your own, as there is a risk of compromising the integrity of the mucous membranes of the uterus, developing the process of inflammation, and infection. Improper removal of the IUD in some cases leads to rupture of the antennae and movement of the contraceptive into the cervical canal. Such situations are always accompanied by the development of severe pain.
The ICD-10 code for removal of the intrauterine device is A11.20.015.
Preparing to remove the fallopian device
As a rule, removal of the intrauterine device is carried out in an outpatient setting. The manipulation must be carried out under aseptic and antiseptic conditions. Before removing the IUD, the gynecologist conducts a general examination of the patient.
At the preparatory stage of removing the spiral, the following is performed:
- Colposcopy.
- Ultrasound examination of organs located in the pelvis.
- Laboratory examination of a smear for flora, oncocytology.
- General laboratory examination of blood and urine samples.
So, let's find out how to remove the intrauterine device.
Extraction
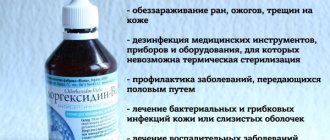
Removal of the contraceptive is carried out after examination of the vagina and cervix. To carry out the procedure, you will need to use gynecological mirrors - with their help, the gynecologist exposes the vaginal part of the uterine cervix. To prevent the development of inflammation and the penetration of pathogens, the mucous membrane is treated with any antiseptic drug.
What instruments are used to remove the intrauterine device?
To remove the spiral, the doctor grabs its antennae, which are the control threads of the product, with a forceps or tweezers. Using medical instruments, the specialist slowly removes it from the uterine cavity.
There is no set time frame for removing the IUD. However, it is recommended to remove the device during menstruation, since during this period the cervix opens slightly. This greatly simplifies the procedure for removing the coil, making it less painful. The most favorable periods for manipulation are considered to be the first and last days of menstruation, since there is no intense discharge at this time.
It is worth noting that a new contraceptive can be introduced immediately if the woman has no contraindications.
Many people are interested in how the intrauterine device is removed after menopause.
Recommendations after installation
In the first week after insertion of the intrauterine device, the patient should avoid excessive physical exertion, refuse sexual relations and use hygienic tampons. During this period, a woman may experience nagging pain in the lower abdomen and slight discomfort. Due to the body's adaptation to the foreign body, the patient may experience a little pain, so doctors recommend more rest during this time.
After 10 days, the patient undergoes a medical examination. To monitor the location of the IUD, she may be prescribed an ultrasound procedure. If a woman has no health complaints, she is not in pain and the intrauterine device is placed correctly, the doctor allows the patient to return to her usual lifestyle. Subsequently, you need to visit a gynecologist every six months.
Probability of ingrowth
In some cases, the contraceptive grows into the wall of the uterus. This usually happens if the patient misses an adequate time to remove the coil. This complication makes it impossible to remove the coil in the usual way in an outpatient setting.
In this case, the spiral is removed after the patient is hospitalized in the gynecological department of the hospital. The removal procedure is performed under general anesthesia using the curettage technique. In this case, the process is monitored using a hysteroscope. A hysteroscope is a device that is used for the diagnosis and treatment of uterine pathologies. Special equipment is inserted through the cervical canal to remove the tumor or take samples of tissue structures for subsequent histological examination.
In some cases, it is not possible to remove the intrauterine device through the cervical canal, for example, if there is an artesia or its fusion. In this case, gynecologists use a laparoscopic technique to remove the IUD through the abdominal cavity. This operation is performed under general anesthesia. During the rehabilitation period, the woman is recommended to use antibiotic medications and anti-inflammatory drugs. A mandatory examination in this case is ultrasound diagnostics.
Possible complications after IUD removal
In essence, the IUD is a foreign body to the body, sometimes causing various complications. After removing the IUD, a woman may develop the following consequences:
- Inflammation of the uterine appendages.
- Acute and chronic forms of endometritis.
- Bleeding.
After the IUD is removed, a woman may notice the following symptoms:
- Moderate bloody discharge.
- Pain in the pelvic area.
- Abdominal cramps.
The presence of aching pain reminiscent of menstrual pain is not considered a pathological situation and does not require consultation with a gynecologist. The appearance of discharge that has an unpleasant odor, an increase in temperature, and poor health are a direct reason to receive medical help.
Recovery period after IUD removal
For 5-6 days after removal of the IUD, a woman should refrain from intimacy, the use of vaginal tampons and suppositories (suppositories). It is also not recommended to douche, visit the sauna and bathhouse, engage in heavy physical activity and sports, take a hot bath and take medications that contain acetylsalicylic acid. Some women, after removal of the IUD, may experience a pulling, aching pain in the lower abdomen, as well as the appearance of minor bleeding or spotting. The appearance of such pathological conditions is considered normal. They do not require treatment as they should disappear on their own within a few days. The next menstruation may begin with a slight delay, which is also considered normal. If a hormonal IUD was inserted, it may take a little longer for your menstrual cycle to return.
After removal of the intrauterine contraceptive device, pregnancy occurs in 30% of patients within the first month, and in 60% during the first three months. Within 1 year after removal of the IUD, pregnancy occurs in 90-95% of women, provided that at this time they do not use other contraceptives.
In this article we will look at how the intrauterine device is removed.
The use of these devices as contraceptives has a number of specific advantages. However, despite the fact that this method of preventing unwanted pregnancy is effective, cost-effective and long-lasting, removing the intrauterine device within a certain period of time is a necessary procedure.
Development of inflammation after extraction
The manipulation of removing the spiral is a simple procedure. If there are no complications or surgical intervention, the patient is recommended to adhere to a number of rules:
- Avoid douching and using tampons.
- Exclusion of visits to the beach, sauna, bathhouse.
- Compliance with recommendations regarding intimate hygiene.
- Reducing the intensity of physical activity.
- Maintain sexual rest for several days.
If you wear an intrauterine device for a long time, serious consequences can develop. It is important that a woman removes the contraceptive as soon as its service life has expired.
It is worth noting that the spiral can cause the development of inflammation and discomfort, so you should not wait until the end of its service life if you have such complaints.
After removal of the IUD, in some cases the nature of the menstrual cycle may change. The duration of the recovery period can vary and reach several months.
How long the recovery period will last is determined by factors such as:
- Psycho-emotional state of the patient.
- Presence of concomitant pathologies.
- Level of endometrial thinning.
- Duration of wearing an intrauterine device.
- Patient's age.
- A type of spiral (simple or hormone-containing).
After removing the IUD, menstruation may be:
- Scanty due to depressed ovarian functionality.
- Abundant, which in some cases may indicate the presence of an inflammatory process.
It is worth noting that the maximum recovery period can last 4 cycles.
Recovery after removal of the spiral
The procedure for removing an IUD is a simple procedure. In the absence of complications and surgical intervention, the patient should follow a number of rules:
- maintain sexual rest for several days;
- reduce the intensity of physical activity;
- adhere to recommendations related to intimate hygiene;
- exclude visiting the bathhouse, sauna, beach;
- stop using tampons and douches.
Wearing an IUD for a long time can lead to serious consequences. A woman must remove the contraceptive after its expiration date.
After removal of the IUD, a change in the nature of the menstrual cycle is sometimes noted. The length of the recovery period varies and can be several months.
The length of the recovery period is influenced by the following factors:
- type of spiral (hormone-containing);
- woman's age;
- duration of contraceptive use;
- level of endometrial depletion;
- concomitant pathologies;
- psycho-emotional state.
Menstruation after removal of the IUD may be:
- abundant, which sometimes indicates inflammation;
- scanty due to inhibition of ovarian function.
Cost of the procedure
In some clinics, the cost of IUD removal procedures includes a gynecological examination and preliminary diagnosis. The average cost of an IUD removal procedure in Russian clinics is 1,500-2,000 rubles.
Where can I remove the intrauterine device? The doctor will also be able to provide preliminary consultation to the woman.
You can get a contraceptive from almost any gynecologist in a public or private clinic.
Thus, the coil should be removed in a timely manner; the service life of the product is determined by its type and the individual characteristics of the female body. If pathological symptoms appear, removal of the IUD before the end of its service life is indicated. If you follow the advice and recommendations of the gynecologist, the use of an intrauterine device does not cause any inconvenience to the woman and does not cause any complications.
Reviews about removing the intrauterine device
Women tend to respond positively to intrauterine devices, as this method of contraception has a number of advantages over other methods. However, contraception using the IUD is not as common as oral or barrier contraception. The process of removing the IUD (if the woman has no complications) also does not cause inconvenience - the manipulation is quick and, as a rule, painless.
Using an intrauterine device as a means of contraception has certain advantages. Despite the effectiveness of protection from unwanted pregnancy, cost-effectiveness and long-term use, removal of the IUD at a specific period of time is considered a necessary procedure.
How to remove the IUD in women: let’s understand the correct manipulations
Many women, especially those who already have children, choose the female intrauterine device (IUD) as their primary method of contraception. This is an effective way to avoid unwanted pregnancy with the ability to continue sexual activity without the use of hormonal pills.
The IUD is a T-shaped flexible device with a nylon thread attached to the shaft. The spiral is inserted into the uterine cavity for a long period (2-7 years). Due to the special design and properties of the spiral material (copper, silver, hormone content), the embryo cannot settle in the uterine cavity and develop there. The ends of the threads of the installed spiral remain in the vagina. They are needed so that after the service life has expired or due to complications, the spiral can be easily removed.
When should I remove the coil?
The IUD must be removed before its expiration date. An “expired” IUD can grow into the tissue of the uterus, lead to infection and inflammation of the reproductive organs, and result in infertility.
If a woman, after installing the IUD, experiences continuous pain, intermenstrual bleeding or discharge of pus, changes in the course or cessation of menstruation, discomfort during sexual intercourse and other pathological processes, the IUD is probably not suitable for the woman, and it should be removed without waiting for the expiration date.
Extraction procedure
Immediately before removing the spiral, the patient is examined with palpation of the abdominal cavity and uterine area. A doctor describes how a female IUD is removed to prepare the patient for the procedure. The gynecologist finds the IUD threads, inserts a dilator to stabilize the uterus and treats the cavity with an antiseptic. Removing the IUD does not require anesthesia, although the woman can take a mild pain reliever if necessary.
The woman should take a slow, deep breath, at which point the gynecologist picks up the IUD threads with forceps and carefully removes the IUD from the uterus. The standard procedure takes a few minutes.
A doctor's recommendations, rules of intimate hygiene, and taking vitamins will allow you to quickly restore the functions of the uterus and reproductive system after removal of the IUD, unless the woman decides to re-install the IUD.
In the Arabin 24 online store of gynecological products, women can buy an intrauterine contraceptive device from the best manufacturers at an affordable price.
Every woman treats various gynecological manipulations with special caution. Those who prevent unwanted pregnancy with the help of an IUD have a logical question about how to remove the IUD from the uterus. It is worth saying that this method of contraception is quite popular, especially among women who already have children.
If the device was installed for the first time, and the time for its removal has already approached, of course, it is worth asking how the IUD is pulled out of the uterus (a video of this procedure can be presented on specific resources), but it is not recommended to do this yourself. Therefore, we will consider in more detail when it is better to remove the IUD, and what difficulties you may encounter.
Complications and possible consequences
In most cases, there were no complications after removal of the IUD, but they may appear when removed for medical reasons. Non-steroidal anti-inflammatory drugs help reduce pain:
- Indomethacin;
- Ibuprofen;
- Ketorolac;
- Diclofenac.
With partial expulsion of the IUD, bleeding may occur, which will require treatment. For hemostatic therapy, Etamzilat tablets and aminocaproic acid are used orally.
For women who have used Mirena, the effects of removal may take several months to appear. The hormonal spiral inhibits the development of hyperplastic processes, so after its removal, the pathology can be activated with renewed vigor.
Indications
The time when the intrauterine device is removed is determined by its recommended duration of use. The presented contraceptive product can be of several types. Initially, they differ in shape, which is represented by an umbrella, a ring, or similar to the letter T.
As for the active components, these can be spirals containing copper, silver, gold and hormones. It is the latter type that is subject to the most stringent recommendations regarding compliance with the deadline when the intrauterine device is removed. On average, a product can last from 3 to 10 years, which depends on its constituent substances:
- With copper – 3-5 years;
- With silver – 5-7 years;
- With gold – 5-15 years;
- With hormones – 5-7 years.
However, experts identify a number of reasons when the IUD is pulled out of the uterus before it loses its properties.
Let us consider in more detail possible diseases or conditions in which a woman may need to remove the IUD in advance. Initially, this may be if a young girl is planning pregnancy. Since the level of contraceptive effect is quite high, fertilization will not occur with the IUD installed. Reproductive function is restored a month after the IUD is removed from the uterus.
Considering that there is still a certain percentage of the probability of conception, if you suspect that pregnancy has occurred, the product must be removed, since often in such situations the embryo is attached not in the uterine cavity, but in the tubes. It is very important to undergo a full examination, including an ultrasound scan of the pelvic organs.
When is the best time to remove the intrauterine device, you should discuss it with your doctor. For example, some women may experience allergic reactions to the product. In this case, the IUD must be removed so as not to aggravate the health condition.
You should think about removing the spiral if you have the following conditions:
- Between menstrual bleeding, a woman develops atypical discharge mixed with purulent exudate;
- The nature of the regulations has changed for the worse, they have become scarce or abundant, lasting more or less than the standard time (provided that the situation persists for several months);
- The girl feels mechanical discomfort, friction and tingling appear in the reproductive organs;
- If the spiral has shifted, as evidenced by the loss of female control over the antennae, which must be checked periodically;
- During intimacy, the threads of the product are felt;
- Amenorrhea and menstrual irregularities are noted.
Before the procedure, your doctor will tell you how to remove the intrauterine device. Women who have reached the age of menopause, and this condition has already lasted more than one year, do not require contraception, since pregnancy is excluded due to the decline of reproductive function.
Since there are several sizes of products on the pharmaceutical market, there is a possibility that in some clinical case it will be selected incorrectly, and then the girl will feel discomfort. The spiral is also removed in the presence of benign or malignant tumors in the cervix and the organ itself, in case of displacement or partial prolapse of the IUD, if a uterine probing procedure is prescribed.
How is an IUD removed?
Standard removal of the coil is painless and therefore does not require the use of anesthesia. The doctor removes the structure by the threads. If the threads have been lost or the spiral has grown into the wall of the uterus, it is removed using a hysteroscope. Manipulations are performed under local anesthesia or under medicated sleep. The specialist inserts the instrument into the uterine cavity and, under visual control, grabs the spiral with microsurgical forceps, after which he removes it out.
When removing an ingrown system, the procedure is completed by curettage of the endometrium.
Attempts to remove the coil at home can end in disaster. To avoid trouble, trust the professionals. Specialists at the Spectra clinic will conduct the necessary studies, after which they will remove the system extremely carefully and painlessly.
Even in ancient times, intrauterine contraception was known as a reliable method of protection. However, a separate direction in gynecology appeared only in the middle of the 20th century.
Intrauterine contraception is being improved: materials that are harmless to the body are selected, the technical design is improved, active metal and hormonal agents with a “shape memory” effect and calculation of daily excretion into the body are added. Thanks to innovations in gynecology and obstetrics, it has become possible to individually select intrauterine devices (IUDs). Now more than a hundred varieties of this method of contraception are known.
Intrauterine contraception can be neutral (without the use of medications) or medicated. In the latter case, the addition of drugs such as gestagens, copper, gold, silver is due to a decrease in side effects on the body and an increase in the effectiveness of contraceptives. Of the neutral IUDs, the Lipps loop, Margulis spiral, etc. have proven themselves to be the most effective. Non-medicinal ones – IUD Juno Bio-T, Sorreg-T 200.
Installation of an intrauterine contraceptive device
The selection and installation of the spiral is carried out by a doctor (obstetrician or paramedic) after a thorough examination for infectious processes and a gynecological examination. Intrauterine contraceptives are administered to non-pregnant women who do not have an inflammatory process in the body, preferably 5-9 days after the end of the next menstruation. If a woman has recently given birth, the optimal time for inserting an IUD is 5-6 months after birth.
The spiral begins to operate immediately after its installation. Minor spotting is possible for several days. The attending physician must provide the patient with written information about the type of IUD inserted and its duration.
4-6 weeks after insertion of the IUD, the patient should visit her doctor for an examination. The first month you should check the threads several times, then this check may only be due to unusual discharge, pain after sexual intercourse, or cramping pain in the lower abdomen. If you cannot feel the spiral threads, you should immediately consult a doctor. The same must be done in the absence of menstruation, the IUD falls out, or the hard body of the IUD is felt.
The lifespan of an intrauterine device depends on its type. Medicinal IUDs are worn for one to ten years. But it has now been proven that the longer the intrauterine device is worn, the greater the risk of developing inflammation. Therefore, doctors agreed on the optimal period for wearing spirals (especially those containing copper) – no more than 5 years.
The effectiveness of the intrauterine contraceptive is calculated using the Pearl index (the number of unwanted pregnancies per 100 years is calculated). Using non-drug IUDs, the indicator is 2-3, hormone-containing IUDs (Mirena IUD, for example) – from 0.8 to 2.9, copper-containing ones – 1-2. The effectiveness of the IUD is also affected by the woman’s age - the older it is, the lower the contraceptive effect.
The presence of side effects depends on many indicators. Individual characteristics, the correct selection of the IUD, its type, frequency of follow-up, and duration of use all play a role. The following complications can often occur:
- ectopic and uterine pregnancy,
- loss of threads,
- pain syndrome,
- perforation of the uterus,
- bleeding,
- increased vaginal secretion,
- inflammatory diseases.
The last side effect is the most common, which significantly slows down the pace of development of intrauterine contraception. Much depends on the woman’s age: the older the woman, the lower the risk of inflammation.
There are also contraindications for installing a spiral. These include:
- suspicion of pregnancy,
- ectopic pregnancy,
- appearing in the anamnesis,
- malignant tumors,
- tumor and inflammatory diseases of the genitals,
- uterine bleeding.
- It is undesirable to use an IUD for women who frequently change sexual partners.
Removing the spiral
The IUD is removed during menstruation by pulling the thread. If the thread breaks, the spiral is removed using a curette or hook. In other cases, which include an inflammatory process, difficulties in removing the coil using the usual method, the coil is obtained with an ultrasound examination and antibacterial therapy in a hospital setting. The coil can be removed at any time - it is not necessary to wait until the end of its use period. After removing the intrauterine device, the gynecologist must examine the internal organs.
It is worth remembering that the IUD may spontaneously fall out in the first weeks after insertion. If this happens, you need to urgently contact a gynecologist. Also, intrauterine contraception does not protect against sexually transmitted diseases and AIDS.
Intrauterine contraception has proven itself in gynecology and obstetrics due to its high efficiency, possibility of long-term use, immediate contraceptive effect, rapid restoration of fertility after removal of the device, and low cost. Women who have recently given birth turn to the IUD due to the absence of a negative effect on the lactation process. Also, for some gynecological diseases, the spiral can have a therapeutic effect.
However, the use of IUDs is now only in second place among all types of contraceptives. The reason for this is some disadvantages of spirals. The first of these is the need for medical intervention to insert and remove the contraceptive. Also a significant argument was the possibility of increased menstrual blood loss (which can lead to iron deficiency anemia), painful menstruation, and the development of ectopic pregnancy. Also, nulliparous women and patients who are sexually active with multiple partners cannot use an IUD.
Complications
Some women are wondering how to remove the IUD from the uterus at home. It is strictly forbidden to carry out this procedure yourself. All manipulations should be performed only by an experienced, qualified specialist, otherwise there is a risk of developing serious gynecological problems.
It is not recommended to use contraceptives longer than the specified expiration date. If you neglect this rule, then the following cannot be ruled out:
- The spiral can grow into the tissue of the reproductive organs;
- Inflammatory diseases will begin to progress;
- Chronic pelvic pain syndrome will appear;
- Reproductive organs will become more susceptible to infection;
- Women may develop infertility.
Every girl should be attentive to her health. It is imperative to undergo gynecological preventive examinations. It is also worth remembering that the IUD is installed for many years, so it is possible that a woman may forget when it was inserted. Such data must be recorded and stored in a secure place so that funds can be recovered in a timely manner.
IUD removal algorithm
To remove the IUD, you must visit a doctor at a antenatal clinic or medical clinic on the 3-5th day of your period. The manipulation is carried out step by step:
- the woman lies down on the gynecological chair;
- the vagina is examined in speculums and two-handed examination;
- the doctor reinserts the speculum into the genital tract;
- Using tweezers or special forceps, grab the protruding antennae and lightly pull them.
The coil is easily removed with a small amount of blood or small clots, the process is not painful. After removing the device, the vagina is treated with an antiseptic.
If simply pulling the antennae does not cause the coil to fall out or severe nagging pain appears, its removal is considered complicated. The woman is offered hospitalization. The repeated procedure is performed under anesthesia.
Some people try to remove the IUD from the uterine cavity at home. This may result in the development of vasovagal syndrome, which is manifested by a sharp decrease in pressure, bradycardia and fainting.
Preparation
Every woman who uses an IUD is interested in how the IUD is removed from the uterus. There are a lot of videos on this request, but you should always remember that the procedure should be trusted to a gynecologist, and under no circumstances should you do it yourself. Retrieving funds is a serious process, so it is necessary to properly prepare for it.
If a woman is not planning a pregnancy, then approximately 7 days before the scheduled procedure, it is necessary to stop intimate intimacy without using a barrier contraceptive (condom). Such a long period is determined by the ability of sperm to maintain their functions for a week. If ovulation occurs at this time, fertilization is possible.
When wondering how the IUD is removed from the uterus, it must be said that this procedure is best performed during menstrual bleeding. This period is optimal because it makes the process easier. Ideally, you should visit a gynecologist three to four days after the start of the regulation, when the discharge is not so abundant. But these conditions can be neglected if there are alarming symptoms.
Initially, the doctor will definitely examine the woman in a gynecological chair. Thanks to this, he will be able to determine the location of the uterus, and also palpate the abdominal cavity with one hand, while the fingers of the second limb will be in the vagina. Such actions are necessary to detect the spiral antennae. The final stage is dilation of the cervix and its stabilization, as well as treatment with an antiseptic.
Removal
When the preparatory stage is completed, the doctor will tell the patient to take a deep but slow breath, during which he hooks the threads of the spiral hanging from the cervical canal using forceps and carefully removes the product from the uterine cavity. After this, the spiral can be removed by hand. Since there is heavy discharge during menstruation, the procedure creates good gliding.
As for the duration, removing the spiral lasts several minutes, which includes the preparatory stage. After the product is removed, it is normal to experience muscle spasms, cramps and minor hemorrhages that last a short time.
Removing the IUD from the uterus. Source: gynlogy.ru
If the patient wishes, she can have a new IUD installed on the same day, provided there are no complications. As you can understand, there is no clear schedule for removing the contraceptive. Therefore, a woman can come for the procedure at any convenient time, regardless of the period of her menstrual cycle.
Many girls may be interested in whether there is pain during the process of removing the intrauterine device. In most cases, doctors do not use anesthesia. If the patient is very worried, then before the procedure you can take a mild sedative and analgesic. If the pain threshold is low, local anesthesia can be used. It is possible that the tendrils of the product may break, in which case it is removed using a hysteroscope.
Difficulties
Since removal of the intrauterine device is a gynecological procedure, during its implementation circumstances may arise that force the doctor to act differently than planned. In this case, difficulties may arise. To determine what exactly prevents the product from being removed, an ultrasound examination is prescribed, through which you can find out the following:
- Has the correct angle of direction of the clamps been selected?
- Has the spiral grown into the tissue of the organ?
- How tightly the product adheres to the wall of the uterus.
The second point is the most serious. Often, this condition is detected in those women who remove the IUD untimely. However, if the gynecologist is experienced, then he will solve this problem without causing any harm to the reproductive organs.
How to remove an ingrown helix?
In clinical practice, an ingrown intrauterine device is rare. This is due to the mechanism of action of the contraceptive. If a woman follows the terms of wearing the IUD, then there is no risk of ingrowth. Only when using the IUD for 8-10 years or more is it able to become covered with a layer of endometrium. In this case, it will not be possible to remove the spiral with tendrils by simply pulling. The woman will be offered hospitalization in the gynecology department.
The manipulation will be performed under anesthesia to reduce pain. On a preliminary ultrasound, the doctor will be able to notice the depth of the IUD ingrowth. It can penetrate the mucous layer or grow into the myometrium. In the first case, removal will require curettage of the uterine cavity. If the contraceptive has penetrated the muscle layer, then laparoscopic surgery is necessary for removal.
Ingrowth of the spiral in healthy women is excluded. Those at risk are those who have chronic inflammation, hyperplastic processes or oncology - direct contraindications for the use of an IUD.