The intrauterine device is one of the most popular methods of contraception. Its use allows a woman to live a full sex life. The device causes virtually no complications. In rare cases, a woman notes that she has inserted a coil and is bleeding. The symptom is frightening, but it is worth figuring out whether it is so dangerous, whether it is normal or pathological.
Installation of a uterine device is a popular method of contraception
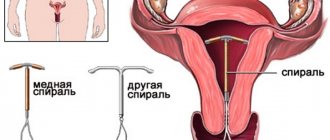
What types of spirals exist?
There are two main types of IUDs:
- medicinal;
- non-medicinal.
The former contain copper, silver, gold, progesterone, and other hormones or drugs. Their presence in the composition increases the effectiveness of the spiral and reduces the negative impact on the body. These means have different shapes: spirals, rings, etc. The most common contraceptives are:
- Copper-T. It is a device in the shape of the letter T, made of polyethylene with the addition of copper.
- Multiload. It has a T-shape and is made from polyethylene with the addition of barium sulfate.
- Juno. Available in various variations: T-shaped, ring-shaped. The main material is plastic, with additional inclusions including copper or silver. The duration of contraception for ring-shaped forms is 4 years, for T-shaped ones - 7 years.
- Mirena. Intrauterine hormone-containing system. The principle of action is based on the release of gestagen into the uterine cavity. Is a prescription contraceptive.
- Nova-T. The spiral is made of plastic with the addition of barium sulfate, copper and silver wire wound onto an axis.
You can find a Mirena-brand spiral at the pharmacy.
The timing for installing the spiral is shown in the table.
| Type of IUD | Validity |
| Copper-T | 6 years |
| Multiload | 5 years |
| Juno | 4–7 years |
| Mirena | 5 years |
| Nova-T | 5 years |
The latter belong to the first generation of IUDs. They are made of polyethylene and are no longer used in modern gynecology due to multiple side effects. These include the Lipps Loop.
How and when to install and remove a spiral
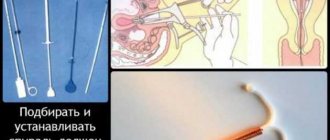
Before inserting an IUD spiral into the uterine area, a doctor’s consultation, a gynecological examination, a vaginal smear for flora, histology and sexually transmitted infections, and an analysis of the woman’s general health are required. Based on the results of visual, laboratory and instrumental studies, the gynecologist makes a decision on the possibility of using intrauterine contraception and, if the result is positive, sets a day for the procedure.
Most often, the IUD is placed a few days before or during menstruation. This depends on the anatomical features of the patient.
As a rule, there is no need for anesthesia - local anesthesia is sufficient. To carry out the procedure, the doctor needs to use instruments to open the cervix, perform an examination, measure the depth, insert the spiral itself and secure it in the cavity. All this will take no more than 5-15 minutes.
Before the procedure, many people worry whether it will hurt to install and remove the spiral. In this matter, almost everything depends on the competence of the doctor. An experienced and attentive gynecologist will not cause pain, but only slight discomfort.
Indications for removal of the intrauterine device:
- inflammation of the female pelvic organs;
- detection of sexually transmitted infections;
- heavy uterine bleeding;
- persistent or unbearable pain;
- expiration of the period of use.
In the absence of negative effects on the body, a copper coil can be kept inside for up to 10 years, a hormonal coil for up to 5 years. It needs to be removed a few days before your period, and a new one can be installed after a month. After removing the Mirena (the most popular hormonal IUD), the ability to conceive a child returns the very next menstrual cycle.
What are the indications for installation?
The differences between the functional properties of different types of IUDs are insignificant. They all have the same effectiveness, which in turn depends on the professionalism and experience of the doctor. Before inserting an intrauterine device, the gynecologist examines the woman for inflammatory diseases of the genital area, receives information about the frequency of the menstrual cycle, and conducts an ultrasound of the pelvis. After the collected medical history, the coil is selected and inserted.
The indication for the use of an IUD is a woman’s desire to control her reproductive function.
Uterine devices containing hormones, in addition to the contraceptive effect, have a therapeutic effect for the following diseases:
- endometrial hyperplasia;
- heavy menstruation;
- endometriosis.
If there is heavy discharge during menstruation, a hormonal IUD can be placed
Reviews from women and specialists
Feedback from patients and specialists allows us to conclude that the intrauterine device is a highly effective means of contraception, which has been used abroad and in domestic practice for decades.
In recent years, the IUD has become affordable. It is easy to install, the procedure itself takes no more than 15 minutes. The process is painless if there are no contraindications, and it is carried out by an experienced specialist.
An additional advantage is that installation of this product is possible at any age. Some women in their reviews say that they had the IUD for almost the entire period of their reproductive years.
A natural occurrence when placing the IUD inside the uterus is discharge. As a rule, they are brown and have no foreign odor. Depending on the cause, such bleeding lasts from several days to six months.
Victoria, 42 years old: “As long as I have been sexually active (since I was 17 years old), I have been wearing the IUD for as long. All my life she protected me from conception. When my husband and I decided to have a child, as planned, the specialist removed it, and after two menstrual cycles I was able to get pregnant. After giving birth, this wonderful invention was placed again. I didn’t notice any special discharge; as a rule, it was a slight spotting for about a week, and in the first days after the installation I felt a slight tug in my lower abdomen.” Marina, 25 years old: “After the implantation of the IUD, my period lasted for another two weeks. As it turned out later, it was discharge against the background of endometrial detachment, the vessels of which are quite weak. This is how the specialist explained it to me. Now my menstruation is going differently. There's a lot more blood. But it doesn't make me uncomfortable. The main thing is that I am reliably protected from an unwanted pregnancy.”
Thus, the IUD is an excellent, highly effective contraceptive. When placed correctly and all rules of use are followed, it gives the highest results among means of protection and does not cause harm to the body. IUDs were invented for those women who keep up with the times and value their health.
source
What complications can there be?
When using intrauterine contraceptives, complications occur extremely rarely. Despite the fact that all consequences are preventable, a woman should know how they manifest themselves and, if necessary, seek medical help:
- Bloody discharge after installation of the IUD is observed in 15% of women. They may appear periodically during the first year of using the contraceptive.
- Expulsion of the IUD. Rejection is manifested by pain in the lower abdomen, bleeding between menstruation, discharge after sexual intercourse, and the sensation of an IUD in the vagina.
- Pregnancy with an IUD. It occurs very rarely and is usually caused by undiagnosed expulsion. In this case, the IUD should be removed as quickly as possible.
- Perforation of the uterus or cervix. The frequency of complications depends on the form of the contraceptive, the anatomical structure of the uterus, and the qualifications of the doctor. It is characterized by severe pain when inserting the coil, disappearance of the threads, and bleeding.
- Infectious processes of the pelvic organs. Complications occur in women who have multiple sexual partners. Symptoms of sexually transmitted infections include discharge with an unpleasant odor, high body temperature, and nausea.
Sometimes, when installing an IUD, an infection can occur.
Pathological discharge when using a spiral
Infection
This contraceptive is designed to protect a woman from unwanted pregnancy, but it does not perform a barrier function against various infections, viruses and fungi. Moreover, it is a kind of conductor for them and in some situations may even be the root cause of inflammation of the pelvic organs. This may be indicated by excessive bleeding with discomfort, or the presence of an unpleasant odor or greenish or yellowish mucus color.
Fixture offset
One of the complications that can cause bleeding during the installation of the coil is its loss or displacement. This includes both spontaneous violation of the position and rejection by the body. A foreign body is a fairly large load on a well-functioning reproductive system, so it can take this device for too long, letting bloody smears know about it, or not take it at all.
What are the causes of bleeding after installation or removal of the coil?
If a woman suffers from severe pain and is bleeding after having an IUD inserted, the development of complications should first be ruled out.
Possible causes of bloody discharge immediately after administration:
- IUD rejection;
- incorrectly selected size;
- infectious process;
- endometrial injury during installation.
You can learn about the pros and cons of the intrauterine device by watching this video:
The main cause of bleeding after IUD removal is damage to the uterine mucosa. When the device is removed, microtraumas appear on the endometrium, which can bleed. Usually, unpleasant symptoms disappear after 7–10 days and do not require treatment.
Removal of the IUD
After the IUD, you can plan a pregnancy within the first month. Removal of the IUD is carried out for the following indications:
- at the request of the woman;
- expiration of the period of use. The contraceptive device is valid for 5 years. After this time, you should undergo examination by a specialist and remove the device;
- when the spiral is displaced or partially falls out;
- during menopause.
Removal is carried out in a gynecological hospital. The procedure is carried out during menstruation. The appearance of discharge after the IUD will last only for the period of the remaining menstruation. The regularity of the cycle is restored. The IUD can be removed on any other day of the cycle. The removal procedure is simple and painless.
Important! If the intrauterine contraceptive has grown into the wall of the uterus, then it is not possible to remove it in the usual way. In this case, removal is carried out in a gynecological hospital using diagnostic curettage of the uterine cavity.
There are no specific recommendations after removal of the IUD, but there are a number of simple rules that must be followed for 1 week: sexual rest, maintain intimate hygiene, do not use tampons, limit physical activity, do not douche, do not visit baths and saunas.
Can a violation be a variant of the norm?
Most women bleed after installing the IUD; this is not always a pathology. The contraceptive is administered from the 3rd to the 8th day of the menstrual cycle. During this period, small menstrual flow is still present, and due to mechanical stress, it may intensify. During the process of implantation of a foreign body, small amounts of blood often appear between menstrual cycles.
In case of heavy bleeding, weakness, severe pain, or pale skin, you should immediately consult a doctor.
What to do in case of heavy bleeding
In many cases, patients with heavy discharge should be monitored regularly for a set period of time. If tests after installation fail to reveal any serious abnormalities, and discharge continues, the coil must be removed. If this is not done, then the woman may develop anemia. To prevent the disease, you should take medications that contain iron, as well as eat a variety of foods rich in iron.
Many women experience increased discharge during menstruation. The spiral, after its installation, has an irritating effect on the endometrium. At the same time, the composition of cervical mucus secretion also changes.
Unstable hormonal levels should also be taken into account. The intensity of the discharge becomes especially emphasized. A woman uses pads quite often. If you feel pain and severe weakness, you should immediately consult a doctor. Perhaps the uterus rejects the IUD, associated with severe inflammation.
What to do if you bleed after using the IUD
Prolonged bleeding after removal of Mirena and other IUDs can be caused by serious dysfunctions in the reproductive system. The gynecologist will prescribe a pelvic ultrasound, examine the genital organs and prescribe the necessary treatment.
Antibacterial drugs are prescribed to treat inflammation
If bleeding is a consequence of infection, antibacterial drugs are used. If there are hormonal imbalances, you should undergo testing for the level of sex hormones. Based on the test results, hormone therapy is prescribed.
Unpleasant sensations after removal of the coil and bloody discharge resulting from severe trauma are treated with hemostatic and painkillers. If heavy bleeding and pain are associated with the use of an IUD, it should be removed.
Achieving the subsequent physiological norm
Over time, the body will strive to restore the hormonal balance, which was disturbed after the procedure for installing the intrauterine device. In addition, more noticeable pain appears during menstruation. After insertion of the IUD, heavy and prolonged menstruation should attract the attention of doctors, especially if the IUD has been in the uterus for about 3 months. Removing the intrauterine device
The service life of the IUD is approximately 5-7 years from the time of installation, and after this period it should be removed. If this is not done in a timely manner, then:
- The device can grow into the tissue;
- Infections may occur;
- Reproductive ability may be lost.
In order to remove the IUD painlessly, this should be done in conditions when the cervix is softened and discharge is minimal. This situation occurs at the end of the menstrual cycle. However, if there are serious adverse reactions, the device must be removed immediately.