The ovaries are one of the most important organs of the female reproductive system. The maturation of eggs occurs in them. A follicle is a separate structure in the ovary within which the formation of an egg occurs. With the onset of menopause, the female body experiences disturbances in the functioning of the genital organs, including the ovaries. The cause of these disorders is hormonal imbalance with age. What should be the normal size of the ovaries in women according to ultrasound during menopause? What does a deviation from the norm indicate?
At the stage of menopause, the functioning of the ovaries is rapidly suppressed, changes in the monthly cycle no longer occur, and there is no menstrual flow.
Normal number of follicles in the ovaries during menopause
The ovaries play a significant role in a woman’s body; they perform reproductive and hormonal functions. The main structural unit of these organs is the follicle. During childbearing age, when it matures, the egg cell necessary for fertilization is formed. With age, functions fade, follicles in the ovaries cease to be produced during menopause, which means a woman loses the ability to fertilize.
Click to enlarge
How to restore ovarian function at home?
First of all, you need to contact your doctor and undergo a comprehensive examination. You need to do a hormonal blood test and undergo an ultrasound examination.
If a diagnosis is made and treatment is prescribed, then you need to adhere to it unquestioningly in order to restore your hormonal levels and give birth to a healthy baby.
You need to forget about various diets, excessive physical activity, do not eat junk food, take vitamins and microelements to improve the health of the whole body. It is best to give preference to fresh vegetables and fruits, and cook food only by thermal processing.
Attention: sometimes all these recommendations are not enough to improve ovarian function; the doctor may suggest surgical intervention, removal of the affected area of the ovary.
Changes in the ovaries and follicles during menopause
The period of menopause, during which various changes occur in the reproductive organs, is conventionally divided into three stages:
- Premenopause. The production of sex hormones decreases, resulting in hormonal imbalance. This leads to the woman experiencing surges in blood pressure, hot flashes, increased sweating, and menstrual irregularities. The number of follicles during menopause in women decreases, the ovaries shrink in size - 25 mm (l) x 15 mm (w) x 12 mm (t). There is a replacement of the cortical substance - the storage of follicles - with connective tissue.
- Menopause. Occurs one year after the last menstrual cycle. The ovaries become even smaller; during menopause, the number of follicles in the ovaries decreases hundreds of times compared to what it was 10-15 years ago. There remain isolated formations that are no longer able to develop.
- Postmenopause. Menstruation stops completely, the ovaries continue to decrease in size, the difference between them becomes almost imperceptible. The blood supply to the organs stops, as does the production of hormones. By the age of 70-80 years, the weight and volume of the ovaries become 3-4 times smaller compared to the reproductive period.
Normal before menopause and after
The fact that the size of a woman’s ovaries is normal can be determined by ultrasound during menopause.
Note! The optimal period for conducting an ultrasound examination is from the fifth to the seventh day of the cycle, by this time the processes associated with menstruation have passed and ovulation changes have not begun.
In a woman of reproductive age, the follicles are clearly visible on ultrasound; the parameters of the oval, elastic glands can be easily determined. Averages:
- length – 2 – 3.5 cm;
- width – 1.5 – 2 cm;
- thickness – 2 – 2.5 cm.
But the size of the ovaries undergo changes depending on the period of the menstrual cycle. On the eighth or ninth day after menstruation, dominance appears among the two glands - it is the enlarged one that will produce an egg this month. Its diameter is from 15 to 24 mm, while the second will remain within 10-12 mm.
The norm of follicles in the ovaries throughout a woman’s life
Follicles are formed during the prenatal period. In the fifth month of pregnancy, a female embryo has about seven million germ cells; by birth this figure decreases by about seven times. By adolescence, there are approximately 300 thousand follicles. At 40 years of age, the norm of follicles in the ovary is significantly different from a younger age.
During reproductive age, there is a cyclical pattern when every month an egg ready for conception matures. The size of the ovaries in this period is on average 20-35 mm in length, 15-20 mm in width and 20-25 mm in thickness.
Normally, 6-10 follicles are formed monthly, then from this number one begins to dominate. During ovulation, it ruptures, resulting in the release of an egg. A corpus luteum forms at the site of the ruptured follicle. This happens regularly throughout each woman’s individual age.
Pathological conditions during menopause
With age, the ovaries should become smaller, but in some cases their enlargement is observed. This condition may be associated with the following pathologies:
- Follicular cyst. Most often, one gonad is affected. A large number of round-shaped formations with thin walls are formed inside it. In most cases, spontaneous resorption of the cyst occurs.
- Polycystic. A characteristic feature is a large number of small cysts formed from underdeveloped follicles. Occurs due to reduced production of female and predominance of male hormones.
- Benign neoplasms. Any tissue of the ovary can be involved in the pathological process; depending on this, tumors from germinal (teratoma), connective (fibroma) tissue, granular epithelium (granulosa cell formations), etc. are distinguished.
- Tumors of a malignant nature. There are primary, when the disease develops independently, secondary, in the case of degeneration of existing benign tumors, and metastatic oncology - in the ovaries it develops as a result of the introduction of metastases from other foci.
Carrying out an ultrasound and performing the necessary tests will help to recognize the disease in the early stages and undergo the necessary course of treatment on time.
Prevention of premature aging of the ovaries
Despite the fact that a woman’s body has a certain supply of follicles, it is possible to postpone the onset of menopause to a later date. This is facilitated by:
- eliminating bad habits;
- sexual life with one partner;
- proper nutrition with enough greens rich in phytoestrogens;
- adequate physical activity;
- avoiding chronic stress.
Regular visits to the gynecologist, timely treatment of diseases of the pelvic organs and monitoring of disruptions in menstrual cycles will be an excellent prevention of not only premature aging of the body, but also the development of severe pathologies.
Prevention of pathologies and early onset of aging
Negative factors (they should be avoided) are:
- use of tobacco products;
- alcohol abuse;
- unbalanced menu - few fruits, vegetables and plants (parsley, asparagus, celery) containing phytoestrogens, a lot of fried and fast food, leading to an increase in toxins and fats;
- frequent termination of pregnancy;
- nervous or physical fatigue, low activity, lack of sports;
- irregular sex life, lack of a regular partner.
- a healthy diet rich in vitamins (especially E - very useful for women), microelements (calcium, phosphorus);
- active lifestyle - try yoga, it is great for ages 40+ and practices poses that improve blood circulation, including to the pelvic organs;
- pay attention to your health, visit a gynecologist not only in case of symptoms, but also for preventive purposes, treat infections in a timely manner and control the formation and growth of cysts.
Important! Smoking significantly reduces the duration of youth at the hormonal level.
Follicles in the ovaries during menopause
The ovaries are one of the most important organs of the female reproductive system. The maturation of eggs occurs in them. A follicle is a separate structure in the ovary within which the formation of an egg occurs. With the onset of menopause, the female body experiences disturbances in the functioning of the genital organs, including the ovaries. The cause of these disorders is hormonal imbalance with age. What should be the normal size of the ovaries in women according to ultrasound during menopause? What does a deviation from the norm indicate?
What happens when single follicles appear before and during menopause?
The ovaries are made up of structural units called follicles.
Each follicle is an immature egg, which is hidden from the effects of negative factors by membranes of epithelial and connective tissue.
Normal structure and its timely ripening determine a woman’s ability to become pregnant. Deviations in their development lead to the formation of tumors inside the ovary and even infertility.
What it is?
Normally, a woman develops from 6 to 10 follicles, the maximum number of which is reached on the 6th or 7th day of the cycle. On the 8th or 9th day, the secondary ones begin to die off. Among them there remains one, which is called dominant.
The rest give way to the main one so that he can mature normally. During the process of ovulation, the dominant follicle bursts, releasing an egg ready for fertilization. However, if a woman develops only one, then there is a possibility that it will not develop into a dominant and will not be able to mature normally.
As a result, an egg ready for fertilization will not be formed, and the process of conception will be impossible. The pathology is called a single follicle.
Maturation is impossible because they produce hormones that affect neighboring ones. Hormones from one follicle are not enough for normal egg maturation.
Causes
There are a number of reasons that lead to this pathology:
- Side effects of oral hormonal contraceptives.
- Pathologies of the thyroid gland and other parts of the endocrine system.
- Rapid weight gain or loss.
- High concentration of prolactin.
- The state of menopause.
- Emotional or mental disorders: severe stress, prolonged depression, psychosomatic and mental illness.
- Inflammation of the pelvic organs.
- Hereditary characteristics.
- Ecological situation.
- Galactosemia.
Attention! It is impossible to independently determine the cause of the pathology; this requires a series of consultations with specialists and laboratory tests.
As you approach menopause, the functioning of the female reproductive system deteriorates, and the likelihood of various pathologies increases. The amount of sex hormones in the blood gradually decreases, which causes the changes that occur.
In addition, the number of follicles in the ovaries is initially limited. New eggs are not produced throughout a woman’s life; they mature sequentially.
By menopause, their number comes to an end, so the likelihood of single ones increases. The last menstrual cycles before menopause occur without ovulation, because the eggs no longer mature.
There are some ways to prolong the normal functioning of the ovaries. These include changing your diet. The diet should include vegetables, legumes, fruits, and phytoestrogens.
This stimulates the production of sex hormones. Folk remedies can also help: licorice and horsetail roots, lungwort and other medicinal plants. There are hormonal preparations based on estrogen, but they should be used only as prescribed by a doctor.
Peculiarity! Any measures during menopause can only normalize hormonal levels, and are completely powerless when the number of follicles themselves comes to an end.
The following methods are used to diagnose a single follicle.
External examination and anamnesis
The patient's complaints are recorded in detail. The specialist must find out at what time the first signs of the disease appeared, possibly in the opinion of the patient herself. How the symptoms of the pathology changed over time.
You will also need information about other diseases suffered by the woman, surgical operations, injuries, poisoning, hereditary diseases, and stay in places with unfavorable environmental conditions.
Gynecological examination in a chair
The specialist determines the condition of the external genitalia, symptoms characteristic of the pathology, and changes in the mammary glands.
Ultrasound
What matters here is the thickness of the endometrium, the size of the ovaries, and the presence of follicles in them.
Laparoscopy
This method allows you to examine the condition of the ovary through a series of small incisions in the woman's abdominal wall. The procedure is considered almost harmless, since the incisions are small in diameter and heal quickly.
Karyotyping
This is a study of the patient’s chromosomes for the presence of hereditary disease mutations.
Echosalpingography
The procedures are special cases of ultrasound examination; they differ from conventional ultrasound in that it requires the introduction of a special saline solution into the fallopian tubes. The procedure can be very unpleasant for patients. However, it sells much more accurate information than a conventional ultrasound examination.
Other methods
- Study of the menstrual cycle.
- Study of blood composition to determine the content of sex hormones.
Treatment options
This disease can be cured. There are two main types of treatment: hormone therapy and physical therapy. In the first case, the patient takes medications that normalize the concentration of sex hormones.
If the pathology is accompanied by amenorrhea, estrogen is prescribed first. The course of treatment is usually long, it can last about 2 weeks, if necessary, repeated after a month.
Physiotherapy methods include ultrasound and electrophoresis.
Prevention
The following methods are used to prevent pathology:
- Proper nutrition. No strict diets, no sudden weight changes.
- Timely treatment of all viral and bacterial diseases, especially those related to the genital area.
- Elimination of the influence of toxic substances and ionizing radiation.
- Refusal of self-medication, especially diseases of the genital organs.
- Regular examination by a gynecologist.
Important! A woman’s psychological state has no less influence on the maturation of follicles than her physical health. Therefore, it is necessary to avoid excessive emotional stress and fight stress and depression.
Pathology can lead to the following complications:
- Secondary infertility. This complication is irreversible if left untreated.
- Early menopause and aging of the body.
- The development of cardiovascular diseases is possible.
- Osteoporosis.
- Depression and other psychological problems.
- Problems in the sexual sphere, decreased quality of life.
Conclusion
Thus, the maturation of single follicles makes fertilization impossible and, without treatment, can lead to irreversible infertility, as well as premature aging of the patient. To prevent this from happening, a woman, especially in adulthood, needs to avoid strict diets accompanied by rapid weight loss, stress and self-medication for diseases of the genital area.
Source: https://mirmamy.net/planirovanie/folliculus/edinichnye-v-yaichnike.html
The structure and features of the functioning of the ovaries
The ovaries are a paired structure located in the pelvic region. Both of its parts are located at the same height on both sides of the uterus. During a woman’s life, the gonads are capable of slightly changing their location, which is associated with pregnancy and the influence of other factors.
The size of the ovaries is individual for each woman. The ovarian artery supplies blood to the glandular tissues. The inside of each ovary is made up of connective tissue, and the outside of the gland is covered by a cortical membrane.
The gonads perform three main functions in a woman’s body:
- Reproductive. The ovary is the place where the egg matures, which is the basis for the conception of a new organism.
- Vegetative. This function implies that the ovaries indicate that the body is female.
- Hormonal. The formation of certain hormones occurs in the ovaries, without which the reproductive activity of the body is impossible.
What functions do these organs perform?
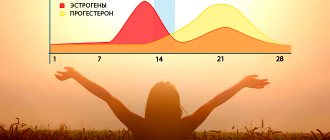
The ovaries are oval-shaped organs of the female reproductive system. They are located on either side of the uterus. In the tissues of the ovaries there are special vesicles - follicles, intended for the development of eggs. They are clearly visible on ultrasound, and also produce female sex hormones: progesterone and estrogens.
From the first day of the menstrual cycle, the process of growth and maturation of follicles begins under the influence of estrogens. One follicle grows faster than the others. The egg matures in it, and it is called dominant. The growth of other follicles is slowed down. During ovulation, the follicle ruptures and the egg is released. The ruptured follicle transforms into the corpus luteum, which produces progesterone.
Changes in ovarian function during menopause
During menopause, significant structural transformations of the reproductive system occur, and there is a decrease in the number of follicles in the ovaries. These transformations are irreversible and natural, leading to the extinction of reproductive ability. With the development of menopause, when the supply of follicles is depleted, connective tissue appears in place of the follicular tissue, and instead of the corpus luteum, hyaline balls are formed. This process causes a change in the size of the gonads. The ovaries shrink, dry out, and their tissues undergo atrophy.
What size of ovaries during menopause can be considered normal? The normal sizes of the ovaries in women according to ultrasound during menopause should have the following values:
- volume – from 1.5 to 4.5 m3;
- length – from 2 to 2.5 cm;
- width – from 1.2 to 1.5 cm;
- thickness – from 0.9 to 1.2 cm.
As a woman ages, the number of follicles in the ovary gradually decreases, which causes hormonal deficiency in the body. And estrogen deficiency is a provocateur of the appearance of menopausal symptoms.
The hypothalamus reacts to the lack of estrogen and tries to normalize the functioning of the ovaries, increasing the synthesis of follicle-stimulating hormone. Due to the increased work of the hypothalamus, the body's thermoregulation is disrupted, resulting in hot flashes.
The size of the ovaries in postmenopause is minimal, estrogen synthesis is excluded. Is pregnancy possible at this stage of life? Pregnancy becomes impossible, because eggs are not formed and there is no ovulation. But this does not mean that there are no estrogens in the female body at the later stages of menopause. The hormone is synthesized in some quantity, but not by the ovaries, but by the adrenal glands.
How female internal organs work, the influence of menopause
The classic cycle of the reproductive system goes like this: eggs are generated, they mature, and attach to the endometrium. If fertilization occurs, the cell settles in the uterus and grows. If not, menstruation begins. Sex hormones – estrogens and progesterones – play an important role in this process. The monthly process leads to the renewal of blood, cells, and the intensive work of all organs.
Important! During menopause (it begins at 40-45 years old, lasts about 5 years and ends at 50+), this cycle is disrupted - the ovaries are not able to produce a sufficient number of eggs, they do not mature. The result is infrequent and painful menstruation with the possibility of vaginal bleeding.
The ovaries are cell-generating glands. They are located on both sides, but have slightly different sizes and can be lowered or raised. The size of the ovaries depends on many factors:
- age – with aging, the need to maintain the normal condition of the genital organs disappears;
- menses;
- ovulation period;
- taking oral contraceptives or hormone therapy;
- number of gestations.
Causes of ovarian enlargement during menopause
Changes in the functioning of the ovaries during menopause are dangerous because they can provoke serious pathologies that one does not have to think about during the fertile period. Every woman needs to remember that the ovaries should shrink during menopause. If the gonads are enlarged, then this is a sure sign of pathological processes. Ovarian enlargement is a consequence of:
Ovarian cysts are found in 30% of elderly patients. Moreover, usually if there is a cystic growth on one gland, then it is also on the second.
Polycystic disease is a disease in which not one cyst, but a group of cystic formations is found on the ovary. During menopause, the risk of this disease increases, since the concentration of female sex hormones decreases, and this occurs against the background of a significant increase in male gametes.
It should be taken into account that provocateurs of polycystic disease are long-term hormonal contraceptives and hormone-based replacement therapy drugs. Women often take hormone replacement medications to relieve menopausal symptoms, but at the same time they risk developing serious ovarian pathologies.
Oncological diseases of the genital organs develop mainly after the onset of menopause. But oppression of a woman’s reproductive system, the end of menstruation, age-related ovarian diseases and hormonal problems are not the main, but secondary causes of oncology. And the main provocative factors are frequent abortions and frequent childbirth during the fertile period, lack of pregnancies, uncontrolled use of hormonal drugs, and bad habits.
What diagnostics are needed after menopause?
In order not to miss the pathological processes occurring in the organs of the reproductive system, a woman should undergo a routine medical examination by a gynecologist at least once a year. Doctors advise doing it more often – once every six months. The doctor will conduct a gynecological examination and refer the lady for an ultrasound of the pelvic organs.
This study allows you to assess the condition of the ovaries and uterus. The specialist will determine the size and structure of the organs, and also assess compliance with normal parameters for a particular age. If a neoplasm appears on the organs, then with the help of this study it is possible to accurately determine its location and size.
You should know that in some cases, even in a completely healthy woman, it is almost impossible to determine the condition of the ovaries after the onset of menopause by ultrasound. Due to the lack of follicles, they are not visible even with a full bladder. The lady will be offered to undergo a transvaginal ultrasound procedure, which is a more accurate study.
A woman can always find time to visit a gynecologist if she wishes. Regular ultrasound examinations during menopause will detect the occurrence of pathology at the earliest stages, despite the natural reduction of organs. When the ovary is abnormally enlarged, the woman will be referred for consultation to an oncologist.
If the tumor is detected at the initial stage of development, it will be easier to treat it. Most oncologists are of the opinion that once a woman is diagnosed with menopause, any cyst or tumor on the ovary should be removed. The size of the tumor is not significant. This position is associated with a high risk of degeneration of a benign neoplasm into a malignant one against the background of prolonged low estrogen levels.
Ovarian examination
It is not difficult to identify an ovarian cancer tumor, since this disease is accompanied by specific symptoms: polyposis of the gonads, increased blood circulation in the area of the affected tissue. If signs of a malignant formation are visible on the ultrasound machine monitor, the doctor sends the patient for a blood test for tumor markers.
Follicular cyst
Most often, follicular cysts form due to hormonal imbalance. These formations are a follicle on the ovary, which is swollen and filled with specific contents during menopause. Follicular ovarian cysts almost never resolve. In most cases, the patient is prescribed hormonal therapy. Sometimes the cyst has to be surgically removed.
What does it represent?
A follicular cyst forms when the egg does not leave the follicle. An overripe follicle fills with fluid and swells.
As fluid accumulates, an inflammatory reaction develops in the cyst. When inflammation occurs, severe symptoms occur and immediate treatment is required.
Why does it appear?
Like all cystic growths on the ovaries, a follicular cyst is of hormonal origin. Menopausal hormonal deficiency causes tumor growth, so in this case hormone therapy is necessary.
What are the symptoms?
The symptoms are severe. A follicular cyst usually hurts a lot. Vaginal bleeding is also possible.
How to treat?
The basis of therapy at the menopausal stage is hormonal medications. But if the condition of the ovaries in menopause does not return to normal after drug treatment, then surgery has to be performed. Usually the patient is sent for laparoscopy. Surgery is definitely necessary after menopause if the cyst is large, continues to grow rapidly, and can degenerate into a malignant tumor.
Diagnosis of pathology
In addition to examination and smears, there are a number of studies that can make a diagnosis with great accuracy. These include:
- computed tomography (CT);
- blood test for thyroid hormone levels;
- determination of the amount of estradiol and follicle-stimulating hormone (FSH);
- ovarian puncture and biopsy;
- laparotomy for diagnostic purposes;
- blood for tumor markers.
If necessary, the gynecologist may prescribe additional studies - cytological screening, Doppler of the vessels of the pelvic organs, hysterosalpingography and other methods.
Prolongation of ovarian function during menopause
How to force the ovaries not to slow down during menopause, thereby delaying the manifestation of age-related pathologies? In order for the follicles in the ovaries to continue to mature during menopause, maintaining reproductive capacity, it is necessary to change your lifestyle and adhere to the recommendations below.
- Proper nutrition . Animal fats, smoked foods, salty foods, and fried foods should be removed from the diet. The menu should regularly include fish, lean meat, dairy products, and plant foods. You must drink at least 1.5 liters of water per day.
- Physical training. Strong sports exercises prevent stagnation in the tissues of the pelvic area. As a result, the likelihood of pathologies of the genitourinary organs is reduced.
- Folk recipes. To support the functioning of the ovaries, you can periodically take decoctions and infusions of medicinal plants containing phytoestrogens. Such plants include red brush, hogweed, red clover, and sage .
- Application of phytohormones . Pharmacies sell many drugs based on phytohormones. These medications are used not only to eliminate hormonal disorders and treat the symptoms of menopause, but also to get rid of the causes and signs of endometriosis and other pathologies of the uterus and ovaries. The best drugs are considered Qi-Klim, Klimadinon, Menopace, Estrovel.
- Hormone replacement therapy. Drugs in this category are available in tablet form, in the form of gels and patches . The composition includes either only estrogens or a hormonal complex. Hormonal medications act quickly and effectively, but are taken only as prescribed by a doctor, as they have many contraindications.
Every woman should remember that the onset of menopause does not eliminate problems in the reproductive sphere, but only intensifies them. To avoid encountering cancer and other serious diseases of the gonads, older women should be periodically examined by a gynecologist.
Functions at different stages
The ovaries give a woman the chance to have children. These paired organs exist so that a follicle, and then a female reproductive cell, is regularly released from many. This happens every month from 12-14 to 45-55 years.
Naturally, not all germ cells are fertilized, and most cycles end with menstruation. The ovaries play an important role in this process of renewing the inner lining of the uterus.
In the first segment of the cycle, they synthesize estrogens, thanks to which the follicle matures. In the second, the corpus luteum, formed after the breakdown of the egg, secretes progesterone. Both of these substances act on the endometrium, allowing it to develop and eventually be rejected, replaced by a new one.
Ovaries and menopause
During menopause, the ovaries practically exhaust their potential. This begins a little earlier, in a period called premenopause. If in a young woman they consist of connective tissue and the cortex, which contains millions of follicles, then by the time they wither, the first begins to predominate.
The size of the organs changes, they seem to shrink. The sizes of the ovaries in menopause at the initial stage look like this:
- Length 20-25 mm;
- Width 12-15 mm;
- Thickness 9-12 mm.
The longer the period of time since the last menstruation, the smaller these parameters are.
But the decrease and correspondence of the sizes of both organs to each other are characteristic of the later stage of menopause. The size of the ovaries during menopause changes over time as follows:
- In the first year after the disappearance of menstruation, it will be 4.5 cubic centimeters;
- After 5 years of absence of menstruation – 2.5;
- After 10 years – 1.5.
And the weight of one organ by the age of 60 years of its owner decreases to 4 g, although at the age of 40 it was 9.5.
During menopause, follicles decrease in quantity and then disappear altogether. The ovaries become less susceptible to the effects of the pituitary hormones FSH and LH. Despite their high concentration, follicle maturation slows down and stops. They can still be detected at its initial stage. True, they will also be noticeably smaller in size than in their youth. Their size and a decrease in hormonal activity are due to the fact that functional cysts no longer appear on the organs.
How organ size changes during menopause
In women of reproductive age, the normal size of the ovaries has the following parameters:
- organ length – 20-35 mm;
- its width is 15-20 mm;
- thickness – 20-25 mm.
Both organs differ in size. This difference is considered normal. In a forty-year-old woman, the normal weight of one organ is 9.5 g.
During premenopause
The menopausal period has three stages, during which the ovaries change their size. The first stage is called perimenopause. It starts with the first symptoms of menopause - hot flashes, increased sweating, surges in blood pressure, excessive irritability and others. They are provoked by hormonal imbalance, which occurs due to the fact that the ovaries begin to produce fewer sex hormones.
How female genital organs change with age.
During premenopause, the menstrual cycle is disrupted. It becomes shorter or longer, and the number of critical days and the abundance of menstrual flow also changes. Delays are more common in women. First for a few days, and then weeks and months. The amount of menstrual flow decreases and lasts fewer days.
The first changes in the ovaries occur in premenopause against the background of decreased estrogen levels. The number of remaining follicles decreases with each menstruation. The cortex, which previously contained follicles, is replaced by connective tissue.
The ovaries begin to decrease in size to the following parameters:
- length does not exceed 25 mm;
- width no more than 15 mm;
- thickness within 9-12 mm.
The ovaries are constantly decreasing in size. After a few months, both organs become the same size.
During menopause and postmenopause
During menopause, the last independent menstruation occurs. They can only be established retrospectively. Therefore, the diagnosis of menopause is made 12 months after menstruation, if there has been no menstrual flow. Throughout this year, the ovaries continue to decrease in size.
The following sizes of ovaries at menopause are considered the accepted norm:
- length is in the range of 20-25 mm;
- width – 12-15 mm;
- thickness – 9-12 mm.
The volume of the organ decreases to a value of 1.5-4 cm 3. In some women, the follicles in the ovaries during menopause still remain in small quantities, but they can no longer develop. Accordingly, ovulation does not occur. If a woman takes a urine test, it will reveal a high level of estrogen produced by the adrenal cortex.
Postmenopause is the final stage of the menopause. In postmenopause, menstrual function is completely absent. Many people are interested in what happens to the ovaries, the work of which is completely completed in the female body.
They continue to decrease in size. So, 5 years after the start of this stage, the volume of the ovaries will be approximately 2.5 cm3, and after 10 years - 1.5 cm3. The weight of the organ in a 60-year-old lady normally does not exceed 4 g.
Features of the functioning of the ovaries during menopause
An important point is how the ovaries work during menopause. After all, this determines all the changes occurring in the body.
Since the number of follicles in each of them is initially limited, it is natural that over the course of 35-40 years they are spent without replacement. Menstruation still occurs at the beginning of menopause, but most of them do not produce an egg. That is, they cannot be fully called menstruation, since they pass without ovulation.
The follicles that remain in the ovaries during menopause at this stage also change qualitatively. Menstruation is also done differently. The volume of discharge may change, and the intervals between them may shorten or lengthen. Critical days become irregular, which was previously considered undesirable and requiring treatment, but is now natural.
The follicles are also “to blame” for all this. A reduction in their numbers leads to a decrease in the production of estrogen by the organs. And since there is no egg, there is no corpus luteum. This means that progesterone becomes significantly less.
Is it possible to boost work?
Menopause is characterized by special manifestations that are perceived very difficult by some. Or she herself overtakes the woman too early. A problem arises: how to get the ovaries to work during menopause.
If the ovaries are larger than necessary
A cyst is one of the reasons for an increase in the size of the ovary in a woman during menopause
Enlargement of both ovaries after menopause is an undesirable and alarming sign. The reduction and disappearance of follicles leads to the fact that normally the organs become smaller.
But menopause is dangerous because many diseases that were previously dormant or did not declare themselves at all become more active. Therefore, if the ovaries are enlarged during menopause, the reasons should be looked for in one of them:
- Cysts. In 30% of cases during menopause, both organs are affected. The neoplasm in this period is not functional, that is, resorbable. As a rule, this is an epithelial cyst that can degenerate into something more serious;
- Polycystic. Sometimes multiple formations are found on organs. Menopause makes them likely due to a drop in estrogen levels and an excessive increase in the amount of male hormones. This is facilitated by long-term use of oral contraceptives, as well as hormone replacement therapy. It eases the course of menopause, but increases the risk of gynecological ailments;
- Cancer. Malignant tumors of these organs are in second place among the causes of death among women from cancer. And they usually occur after the cessation of menstruation. Ovarian cancer is provoked not only by menopausal age, but also by previous life circumstances: abortion, lack of childbirth, taking hormonal drugs.
We recommend reading the article about postmenopause in women. You will learn about the manifestations of this condition, the characteristics of discharge, the reasons for the decline of reproductive function, as well as the need to take medications to relieve symptoms.
Ovarian pathologies
The period of menopause is dangerous because many diseases that did not make themselves felt during reproductive age may well manifest themselves during menopause and cause their owner a lot of trouble and problems.
If during menopause a woman experiences any changes in the ovarian area, this is a very alarming sign, especially when the ovaries increase in size.
It must be remembered that during menopause the ovaries should normally shrink, but not enlarge. If this happened, then there are several justifications for this.
- Cyst . This disease of the reproductive organs affects about 30% of women whose age has crossed the border of 45 years. A cyst is a formation that most often has a symmetrical nature, that is, if a cyst is on one ovary, then there is a high probability that it will form on the second. This neoplasm does not resolve on its own, as some people tend to mistakenly believe. It can only be treated by surgical removal.
- Polycystic disease . It also happens that not one, but several such formations are found on the female reproductive organs at once, which is why this condition is called polycystic. During menopause, they are more likely, since the amount of female sex hormones decreases, and male hormones increase rapidly.
In addition to menopause itself, this disease is facilitated by long-term use of hormonal contraceptives, which are used without a doctor’s prescription, as well as drugs containing female sex hormones (they are often used during menopause as hormone replacement therapy). It must be remembered that hormonal therapy facilitates the course of menopause itself and reduces its symptoms, but the side effect is that such drugs increase the risk of developing gynecological diseases.
- Malignant tumors (cancer). Women often die prematurely from this disease. Typically, such diseases occur after the complete cessation of menstruation, that is, in menopause. However, in addition to menopause itself, the development of such a disease is also influenced by some other factors that occurred throughout a woman’s life. These include: a large number of abortions, very frequent childbirth, complete absence of childbirth, taking hormonal drugs without a doctor’s prescription, and an unhealthy lifestyle.
What to do to avoid missing the disease?
The decline of ovarian function is not a reason to completely forget about these organs. By participating in the menopausal process, they can present unpleasant and even terrible surprises. An ultrasound scan during menopause can recognize danger, despite the reduced size of the organs. The examination may reveal the abnormal size of the ovaries, if any, as well as their asymmetry.
It is twice as difficult to detect healthy paired organs during menopause as it was while the woman still had reproductive capabilities. Follicles that disappear from the ovaries during menopause make visualization through the abdominal wall difficult, even with a full bladder. Significant morphological changes occur in them.
But the transvaginal ultrasound method can reveal all the negative processes occurring in them.
Changes in the ovaries, as in the entire body during menopause, have natural causes. But sometimes diseases interfere with the process, and some of them show obvious signs at the last stage, when it is too late to be treated. To prevent this, you should get examined regularly, and not just when you feel unwell.
Menopause has several phases of development that differ from each other and. Perimenopause is the very first stage when the ovaries have not yet stopped.
Is it possible to stop menopause 1. Turning off ovarian function at a certain age is inevitable. . What to drink during menopause to avoid aging 1.
An ovarian cyst can be treated without surgery during menopause if it does not cause oncological suspicion among doctors, that is, it is not dermoid.
In any case, menopause is inevitable when the uterus and ovaries are removed. . But menopause after surgery does not have such a smooth course as natural.
Signs of ovarian cystadenoma in menopause. The reasons for its development during menopause. What to do with ovarian cystadenoma during menopause.
Causes of ovarian tumor formation in women during menopause, colpitis, uterine fibroids. Treatment of vaginitis and other diseases of the reproductive system during menopause.
Previously asked:
Hello! I am 51 years old. I have large uterine fibroids and cervical dysplasia. I understand that an operation is needed to remove the uterus along with the cervix. But the doctor says that it is better to remove everything, that is, the ovaries. I'm at a loss. Is it really necessary to have my ovaries removed at my age? I'm scared because I can't take HRT. I had my period 3 months ago. According to ultrasound data, ovarian hypofunction. I want to hear an outside opinion. Thank you.
PREMATURE MENOPAUSE
The term “menopause” is derived from the Greek “menos” (month) and “pausos” (end) and means the permanent cessation of menstruation or menstrual cycles, caused by a pronounced decrease and/or cessation (switching off) of ovarian function.
Depending on the time of onset, the following types of menopause are distinguished:
- timely (45-55 years, average 49-52 years);
- premature (36-40 years);
- early (41-45 years);
- late (over 55 years old).
Timely menopause is the most striking manifestation of the menopause or transitional period in a woman’s life. “Climacteric” (from Greek - step, ladder), the terms “menopause”, “menopause”, “menopause” are synonyms denoting the transition from the reproductive period to old age. This period is divided into premenopause, menopause, postmenopause and perimenopause. What is most characteristic of this physiological period? It is characterized by a gradual decrease and exclusion of ovarian function from a complex ensemble of endocrine glands. First, reproductive function decreases and turns off, then, against the background of progressive depletion of the follicular apparatus of the ovaries, menstrual cycles stop (menopause), and 3-5 years after menopause, the hormonal function of the ovaries also turns off.
Both premature and late menopause require close attention and correction of possible disorders. Due to the fact that it is always difficult to estimate which menstruation was the last, it is customary to estimate the date of menopause retrospectively, namely: one year after the last menstruation.
The age of menopause often depends on heredity, which is convincingly shown in identical twins, when the difference in the age of the first and last menstruation in twins ranges from 4-6 months. However, illnesses suffered by the individual and environmental factors play an important role.
Premature menopause is quite rare (1-2%), but there are many reasons for its occurrence. Often the true cause is quite difficult to establish.
The ovary is a complex structure within which the cortical and medulla layers are distinguished. In the ovarian cortex, eggs are laid in utero, surrounded by granulosa cells, forming follicles with eggs. By the time of the first menstruation in puberty, 300-400 thousand of these follicles are found in the ovaries. During the 25-30 years of the reproductive period, follicle maturation, ovulation and death (atresia) of follicles through apoptosis constantly occur in the ovaries. Only 0.1% of the number of follicles ovulate and can give birth to offspring, and 99.9% are atretic. By the age of 40, an average of about 10 thousand follicles remain. In addition, both female (estrogens and progesterone) and, to a lesser extent, male sex hormones are synthesized in the ovaries. These hormones are involved in the formation of a typical female physique and monthly prepare the reproductive organs for pregnancy.
Receptors for estrogen and progesterone have been identified not only in the reproductive organs. Hormonal receptors (representations), through which sex hormones exert their effects, are found in the heart and walls of blood vessels, in the central nervous system, bone, genitourinary and other organs and systems of the body. Since a young woman secretes sex hormones in a cyclical mode, then the organs and tissues experience their effects also in a cyclical mode.
With premature menopause, the cyclic release and influence of female sex hormones on various organs and tissues that have been exposed to this effect for decades ceases. In addition, the woman also loses the ability to conceive.
In recent years, the opinion has become increasingly widespread that it may be more appropriate to call this condition not “premature menopause”, but “premature ovarian failure”. Although, in essence, we are talking about the same process, from the point of view of deontology, it is more appropriate for both the doctor and the patient to call this condition “premature ovarian failure.”
The main causes of premature ovarian failure:
- genetic factors;
- autoimmune process;
- viral infection;
- iatrogenic (chemotherapy, radiotherapy, surgery on the uterus and ovaries);
- idiopathic (environmental toxins, fasting, smoking - more than 30 cigarettes per day).
According to our practice, premature ovarian failure is often observed in mothers and daughters. Despite the fact that there are many reasons, processes in the ovaries mainly occur according to two main scenarios:
- complete depletion of the follicular apparatus of the ovaries, the so-called ovarian depletion syndrome;
- syndrome of resistant (silent, refractory) ovaries, in which follicles are detected in the ovaries, but they do not respond to their own gonadotropic stimuli.
Clinical picture
Common to both options:
- secondary amenorrhea, infertility;
- well developed secondary sexual characteristics;
- FSH and LH levels are high;
- estradiol levels are low;
- symptoms of estrogen deficiency: hot flashes, sweating, insomnia, irritability, decreased memory, and ability to work;
- during the first 2-3 years, osteopenia develops, sometimes osteoporosis; an increase in atherogenic lipid fractions (cholesterol, triglycerides, LDL) and a decrease in HDL;
- occasionally genitourinary symptoms appear: dryness during sexual intercourse, itching, burning;
- improvement occurs when taking sex hormones.
The main differences between the two forms of premature ovarian failure are as follows.
When the follicular apparatus is depleted:
- with ultrasound - small size of the ovaries, absence of follicles in them;
- persistent cessation of menstruation, symptoms of estrogen deficiency progress;
improvement occurs with hormone replacement therapy (HRT); with ovarian resistance: - the ovaries are reduced in size, but the follicles are visible;
- There are rare episodes of menstruation.
When the ovaries are depleted, the symptoms of estrogen deficiency or the symptoms of typical menopausal syndrome are more pronounced.
With resistant ovarian syndrome, estrogen deficiency symptoms are less pronounced, since it is possible, although extremely rare, to activate ovarian function and, accordingly, improve the general condition.
Tactics for managing patients with premature ovarian failure
- Examination.
- Study of anamnesis.
- Determination of FSH, LH, TSH, prolactin, estradiol in the blood.
- Craniography, for headaches - computed tomography or nuclear magnetic resonance, color fields of vision.
- Ultrasound of the genitals with detailed characteristics of the ovaries and uterus.
- Determination of blood lipids.
- Mammography.
- For long-term amenorrhea (more than 2-3 years) - densitometry of the lumbar spine and femoral neck.
Since menopause is premature, and at this age the ovaries normally function, therefore, premature deficiency of sex hormones can contribute to the earlier appearance of typical menopausal disorders, the frequency of which is 60-70%.
Classification of menopausal disorders
Group I - early symptoms (typical menopausal syndrome)
Vasomotor: hot flashes, chills, increased sweating, headaches, hypotension or hypertension, rapid heartbeat.
Emotional-vegetative: irritability, drowsiness, weakness, anxiety, depression, forgetfulness, inattention, decreased libido.
Group II - medium-term (after 2-3 years)
Urogenital: vaginal dryness, pain during sexual intercourse, itching and burning, urethral syndrome, cystalgia, urinary incontinence.
Skin and its appendages: dryness, brittle nails, wrinkles, hair loss.
Group III - late metabolic disorders (after 5-7 years)
Cardiovascular diseases (CHD, atherosclerosis), postmenopausal osteoporosis or osteopenia.
Individual selection of therapy
Taking into account the above, it seems important to develop an individual “program for restoring and maintaining health” for the long term, taking into account the family and personal risk of the main diseases of aging. Such a program should include regular examination, namely ultrasound, mammography, densitometry and/or determination of biochemical markers of bone remodeling, lipid profile, tumor markers, etc., as well as recommendations for lifestyle changes, such as increasing physical activity, a balanced diet, avoiding Smoking and other bad habits help reduce the risk of cardiovascular diseases and osteoporosis.
In recent years, there has been a constant search and improvement of therapeutic approaches to the rational use of HRT in each specific patient (individualization of therapy). HRT preparations differ from each other only in their progestogen component, since the estrogenic component is represented by 17β-estradiol or estradiol valerate, which correspond in structure to ovarian estradiol. In addition, recently much attention has been paid to the choice of route of drug administration (oral or transdermal).
The type of hormone therapy is also selected taking into account the following factors:
- a woman's desire to have a monthly "menstruation";
- when indicating surgical interventions - indications and scope of the operation and the presence of the uterus;
- the presence of fear of pregnancy, especially with resistant ovaries;
- decreased or absent libido;
- indications of heart attacks in young parents, recurrent miscarriage, liver disease, thrombophlebitis.
The goal of HRT is to pharmacologically replace the hormonal function of the ovaries in women with deficiency of sex hormones, using such minimally optimal doses of hormones that would actually improve the general condition of patients, ensure the prevention of late metabolic disorders and are not accompanied by the side effects of estrogens and progestogens.
Basic principles and indications for prescribing HRT
- The use of only “natural” estrogens and their analogues for HRT is indicated.
- Estrogen doses are low and should be consistent with those in the early proliferation phase of young women.
- The combination of estrogens with progestogens makes it possible to protect the endometrium from hyperplastic processes with an intact uterus.
- Women with a removed uterus are advised to use estrogen monotherapy in intermittent courses or continuously. If the indication for hysterectomy was endometriosis, then a combination of estrogens with progestogens or with androgens, or monotherapy with progestogens or androgens in a continuous mode, is used.
Women need to be provided with appropriate information to enable them to make an informed decision to undergo HRT. All women should be informed:
- about the possible impact of short-term estrogen deficiency, namely the occurrence of early typical symptoms of menopausal syndrome and the consequences of prolonged deficiency of sex hormones: osteoporosis, cardiovascular diseases, genitourinary disorders, etc.;
- about the positive effects of HRT, which can alleviate and eliminate early menopausal symptoms, and also actually serve to prevent osteoporosis and cardiovascular diseases;
- about contraindications and side effects of HRT.
To ensure optimal clinical effect with minimal adverse reactions, it is essential to determine the most appropriate optimal doses, types and routes of administration of hormonal drugs.
There are three main modes of HRT.
- Estrogen monotherapy. In the absence of a uterus (hysterectomy), estrogen monotherapy is prescribed in intermittent courses or continuously.
- Combination therapy (estrogens with progestogens) in a cyclic mode.
- Combination therapy (estrogens with progestogens) in a monophasic continuous mode.
Regimes 2 and 3 are prescribed to women with an intact uterus.
Estrogen monotherapy: intermittent courses (estrofem, progynova, estrimax, divigel, estrogel, climar patch, ovestin) or continuous regimen for 3-4 weeks with weekly breaks.
Combination therapy (estrogens with progestogens) in a cyclic mode:
- two-phase drugs: intermittent cyclic regimen (Divina, Klimen, Klimonorm);
- two-phase drugs: continuous mode (femoston 2/10 or femoston 1/10);
- three-phase drugs in continuous mode (trisequence, triaclim).
With this regimen, a menstrual-like reaction is observed, which is extremely important psychologically for a young woman.
Monophasic combination therapy (estrogens with progestogens) in a continuous mode (cliogest, climodien, pausogest).
With a continuous regimen of hormone therapy, a menstrual-like reaction is excluded.
Livial (tibolone) has continuous estrogenic, progestogenic and weak androgenic activity.
If a hysterectomy is performed for genital endometriosis, preference is given to monophasic combination therapy (Climodien, Cliogest, Pausogest) or Livial in order to exclude stimulation of possible endometriotic heterotopies by estrogen monotherapy.
If the clinical picture is dominated by changes in the cardiovascular system and atherogenic fractions of lipids in the blood, preference should be given to two- or three-phase drugs in which the gestagenic component is represented by progesterone derivatives (Climen, Femoston).
If the clinical picture is dominated by weakness, asthenia, decreased libido, pain in bones and joints, and osteoporosis, then preference should be given to biphasic drugs with a gestagenic component - a derivative of 19-nortestosterone (klimonorm), as well as Divin (MPA with a weak androgenic effect) ( table).
For urogenital disorders in perimenopause, preference is given to local (vaginal) monotherapy with estriol without the addition of progestogens. When urogenital disorders are combined with systemic metabolic disorders (osteoporosis, atherosclerosis), a combination of local and systemic therapy is possible.
Cyclic two- and three-phase HRT, along with improving the general condition, contributes to the regulation of the menstrual “cycle”, as well as the prevention of hyperplastic processes in the endometrium due to the cyclic addition of progestogens. It is extremely important to inform the woman about the following:
- when taking two- or three-phase HRT, a monthly menstrual-like reaction is observed;
- HRT drugs do not have a contraceptive effect.
So, combined two- and three-phase drugs are most suitable for women with premature menopause, as they provide cyclic protection of the endometrium with progestogens, similar to what happens in the normal menstrual cycle.
For severe diseases of the liver, pancreas, migraines, blood pressure more than 170 mm Hg. Art., with a history of thrombophlebitis, parenteral administration of estrogens in the form of a weekly patch (Klimar) or gel (Divigel, Estragel) is indicated. In such cases, with an intact uterus, it is necessary to add progesterone and its analogues (duphaston, utrozhestan).
The following examination is recommended before prescribing HRT:
- gynecological examination with oncocytology;
- Ultrasound of the genital organs;
- mammography;
- according to indications - lipid profile, osteodensitometry.
Contraindications for prescribing HRT: - vaginal bleeding of unknown origin;
- acute severe liver disease;
- acute deep vein thrombosis;
- acute thromboembolic disease;
- cancer of the breast, uterus and ovaries (current; if in history, then exceptions are possible);
- endometriosis (estrogens monotherapy is contraindicated);
- congenital diseases associated with lipid metabolism - hypertriglyceridemia, the use of parenteral forms is indicated.
If there are contraindications to HRT, the issue of using alternative therapy is decided: phytoestrogens (climadinon) or homeopathic remedies (climatoplan).
It is appropriate to note that if a woman has a severe reaction to “menopause” and fears of pregnancy, it is quite possible to use low- and micro-dose combined oral contraceptives: Logest, Mercilon, Novinet, Marvelon, Regulon, Yarina - since the number of contraindications increases with age.
Hormone therapy should be continued until the age of natural menopause (50-55 years); in the future, the issue is resolved individually, taking into account the woman’s wishes, her state of health, and reaction to hormonal drugs.
Premature menopause (premature ovarian failure) is a condition characterized by premature shutdown of the ovaries and the development of an estrogen deficiency state. Women with this condition are indicated for hormone replacement therapy to improve their general condition, improve quality of life, and prevent premature aging and diseases of old age.
V. P. Smetnik, Doctor of Medical Sciences, Professor of the Scientific Center of Obstetrics, Gynecology and Perinatology of the Russian Academy of Medical Sciences, Moscow
Composition of biphasic drugs for HRT registered in Russia
| A drug | Estrogens | Dose, mg/day | Progestogens | Dose, mg/day |
| Divina | estradiol valerate | 2 | IPA | 10 |
| Klymen | estradiol valerate | 2 | cyproterone acetate | 1 |
| Klimonorm | estradiol valerate | 2 | levonorgestrel | 0,15 |
| Femoston 2/10 | 17β-estradiol | 2 | dydrogesterone (duphaston) | 10 |
| Femoston 1/10 | 17β-estradiol | 1 | dydrogesterone (duphaston) | 10 |