Hydatidiform mole - what is it?
Having heard a disappointing conclusion from the doctor, the woman tries to find out on her own what a hydatidiform mole is and why this disorder is dangerous. This pathology in obstetrics usually refers to a disease of the fetal egg, in which the chorionic villi degenerate into small bubbles with liquid. The process is accompanied by the proliferation of epithelial tissue. Pathology can be diagnosed by ultrasound examination and characteristic symptoms.
The pathological process can have varying degrees of prevalence, therefore, to facilitate diagnosis and correctly prescribe therapy, doctors use the classification of hydatidiform mole. Thus, it is customary to distinguish the following types of pathology:
- incomplete;
- full;
- simple;
- proliferating mole.
Incomplete hydatidiform mole
Partial hydatidiform mole is essentially a triploid disorder. During its development, using microscopic analysis, doctors can detect 1 maternal chromosome and 2 paternal chromosomes. This happens when an egg is simultaneously fertilized by two sperm. With the further development of pregnancy, areas of normal placenta and embryonic tissue may be found in the uterus. Moreover, the embryo itself is often severely deformed and nonviable.
Incomplete hydatidiform mole has variable development time. Pathology is most often diagnosed at 9–34 weeks of gestation. Clinically, it can be manifested by a discrepancy between the size of the reproductive organ and the current stage of pregnancy. To accurately determine the disease, an ultrasound is prescribed, which can identify all the changes occurring in the embryo at this time.
Complete hydatidiform mole
Complete hydatidiform mole in the early stages is a simultaneous lesion of the entire volume of villous structures of the chorion. With this type of disorder, signs of embryo development are completely absent, and on the ultrasound monitor screen the doctor visualizes numerous bubbles along with edematous chorionic villi. According to the observations of doctors, the pathology undergoes degeneration into a malignant disorder in 20% of cases. As in the case of partial hydatidiform mole, complete mole cannot be treated and requires termination of pregnancy followed by cleaning of the uterine cavity.
Simple hydatidiform mole
A simple hydatidiform mole is a pathology in which the swelling of the chorionic villi is so pronounced that they merge into a single whole. Microscopic examination reveals large chorionic villi. They are often swollen and located directly inside the uterine cavity. In terms of its external features, a simple mole is very similar to a complete mole, which is why doctors often equate these two terms.
Proliferating hydatidiform mole
This invasive hydatidiform mole is characterized by profound abnormalities. During its development, the uterine myometrium grows deeper. As a result, a destructive process begins that requires medical attention. This form of pathology is accompanied by frequent bleeding, which can threaten the life of a pregnant woman. If pathology is detected at a late stage, the only treatment option is removal of the uterus.
What is a hydatidiform mole?
Hydatidiform mole is a benign tumor that develops in the uterine cavity as a result of fertilization of the egg, when instead of a normal embryo and placenta, numerous cysts appear in the uterus. Cysts in medicine are called blisters with fluid, and it is with the growth of such blisters in the uterine cavity that the name of this disease is associated - hydatidiform mole.
How common is hydatidiform mole?
Hydatidiform mole is detected in approximately 1 in 1000-1500 women with signs of early pregnancy.
Why does hydatidiform mole develop?
There are several known reasons for the development of hydatidiform mole, and all of them are associated with “failures” in the fertilization process. Thus, a hydatidiform mole can develop if an egg was mistakenly fertilized by two sperm at once, or if a sperm fertilized a defective egg that does not contain genetic information.
Who is at increased risk of hydatidiform mole?
- In women under 20 years of age and over 35 years of age
- In women who have already had a hydatidiform mole once
- In women who have already had an early miscarriage
- In women whose diet is poor in vitamin A
Partial and complete hydatidiform mole
There are two types of hydatidiform mole:
- Partial hydatidiform mole occurs as a result of erroneous fertilization of an egg by two sperm at once. In this case, areas of normal placenta and embryonic tissue may be found in the uterus, which, however, is deformed and non-viable.
- A complete hydatidiform mole develops when genetic information on the maternal side is missing for some reason. In this case, neither an embryo nor areas of normal placenta are found in the uterus.
Symptoms and signs of hydatidiform mole
The insidiousness of a hydatidiform mole is that at first it manifests itself as a normal early pregnancy: a delay in menstruation, a positive pregnancy test, nausea and vomiting in the morning, etc.
However, soon the woman begins to notice alarming symptoms:
- Bloody vaginal discharge similar to menstruation
- Vaginal discharge containing blood clots and areas of tissue that look like blisters
- Severe nausea and vomiting (which is often mistaken for severe toxicosis)
- Pain and discomfort in the abdominal area
- Increased sweating, cold hands and feet, rapid heartbeat, irritability
If the symptoms listed above appear, a woman should consult a gynecologist as soon as possible.
Why is hydatidiform mole dangerous?
In rare cases, a hydatidiform mole begins to behave like a malignant tumor: it grows into body tissue and can metastasize. This condition is called invasive hydatidiform mole.
It has been noted that complete hydatidiform mole more often leads to this complication: in approximately 20% of cases. With partial hydatidiform mole, this complication develops in 5% of cases.
An invasive mole may contain cancer cells. In this case, they talk about chorionepithelioma or chorionic carcinoma.
Fortunately, chorionepithelioma can be successfully treated and almost always goes away after a course of chemotherapy.
Diagnosis of hydatidiform mole
Since the first symptoms of a hydatidiform mole are very similar to the symptoms of pregnancy, a woman is often unaware of the presence of problems and consults a doctor to register her pregnancy. And already during the first gynecological examination, the gynecologist may suspect this disease.
What will the gynecologist find?
The size of the uterus during a hydatidiform mole usually does not correspond to the period of missed menstruation and exceeds the norm by several weeks. For example, a woman thinks she is pregnant and is 5 weeks pregnant, but her uterus is 8-9 weeks pregnant. Another common finding by a gynecologist during hydatidiform mole is an increase in the size of the ovaries due to the appearance of a large number of cysts in them.
What will the ultrasound show?
Ultrasound is the most reliable method for diagnosing hydatidiform mole. Using ultrasound, you can not only clarify the diagnosis, but also find out the type of disease (complete or partial hydatidiform mole). With a complete hydatidiform mole, an ultrasound will not detect either an embryo or placenta in the uterus. With partial hydatidiform mole, ultrasound reveals areas of normal placenta and embryo. The typical ultrasound appearance of a hydatidiform mole is that of many small cysts (blisters), which some doctors describe as a “blizzard.” In addition, ultrasound reveals enlarged ovaries with a large number of cysts.
Transvaginal ultrasound (through the vagina) is often used to detect hydatidiform mole in the early stages.
What will a blood test for hCG show?
A blood test for hCG during hydatidiform mole allows not only to clarify the diagnosis of hydatidiform mole, but is also used to diagnose malignant complications and to monitor the effectiveness of treatment. HCG levels during hydatidiform mole often exceed 100,000 mIU/ml (mIU/ml). A too rapid increase in hCG levels may indicate a dangerous complication of hydatidiform mole - the development of chorionepithelioma.
What other tests and examinations may be needed?
When the diagnosis of hydatidiform mole is confirmed, the woman may be prescribed additional tests: thyroid hormone test, general blood test, lung X-ray, computed tomography (CT) scan and others. All these tests are aimed at identifying possible complications of hydatidiform mole.
Treatment of hydatidiform mole
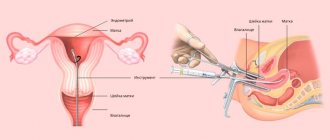
Treatment of hydatidiform mole involves removing the tumor from the uterine cavity. Most often, this procedure is called uterine curettage or cleansing, although vacuum aspiration (“sucking out” the contents of the uterine cavity with a special instrument) is often used to remove a hydatidiform mole. Regardless of the method of removing a hydatidiform mole, this procedure is performed under general anesthesia.
The material obtained as a result of curettage of the uterus is then sent for histological examination. Histology allows you to confirm the diagnosis of hydatidiform mole and clarify its type (complete or partial).
In some cases, the doctor is unable to eliminate the tumor entirely, and then another cleaning may be necessary. This is very important, since otherwise the tumor can grow into neighboring organs and even metastasize (in this case they talk about invasive hydatidiform mole). Invasive hydatidiform mole may be indicated by spotting or bleeding during the first weeks and months after curettage.
If malignant complications of a hydatidiform mole develop, treatment with anticancer drugs (chemotherapy) may be required.
How does the hCG level change after curettage of a hydatidiform mole?
The level of hCG in the blood is an important indicator to make sure that the treatment for hydatidiform mole was effective and your health is no longer in danger.
Normally, after treatment for a hydatidiform mole, the hCG level begins to decrease, reaching normal values (typical for non-pregnant women) within 8-12 weeks.
If after curettage the hCG level remains the same or continues to increase, the woman requires further diagnosis and treatment.
What happens after treatment for hydatidiform mole?
Over the next few months after curettage, you will need close supervision by your doctor. You will have to regularly take blood tests for hCG (initially once a week, then a little less frequently), undergo an ultrasound of the pelvic organs and visit a gynecologist for preventive examinations.
Planning pregnancy after hydatidiform mole
Fortunately, having experienced a hydatidiform mole does not reduce the chances of a successful pregnancy and the birth of a healthy child in the future. However, after treatment for hydatidiform mole, gynecologists recommend waiting a little while planning a pregnancy.
You can resume trying to conceive no earlier than 6 months after your hCG levels have returned to normal. If chemotherapy was used to treat a hydatidiform mole, it is recommended to postpone pregnancy planning for 12 months.
In order to avoid getting pregnant during the recovery period, it is recommended to use condoms. Birth control pills and intrauterine devices increase the risk of complications from hydatidiform mole and are therefore not recommended.
Hydatidiform mole - causes
The reasons for the development of pathology are different and depend on the type of disorder. Thus, a complete hydatidiform mole during pregnancy develops with uniparental disomy - the embryo does not receive a maternal set of genes, but gets two from the father at once. In some cases, this hydatidiform mole may be caused by the fertilization of an anucleated egg by two sperm at the same time. As a result, the fetus dies at an early stage of its development.
An incomplete pregnancy develops when an egg is fertilized by two sperm, and the set of maternal chromosomes is delayed. As a result, at one of the stages of division, the embryo receives one set of maternal and double sets of paternal genes. After a short time, the embryo dies. Among the factors contributing to the development of these disorders, doctors name:
- the age of the expectant mother is less than 20 and more than 35 years;
- a history of hydatidiform mole;
- early miscarriage in the past;
- severe deficiency in the diet of vitamin A.
Reasons for the development of complications
Currently, there is more than one hypothesis for the occurrence of trophoblast pathologies.
Among the main ones it is customary to highlight:
- gestational chromosomal disorders: uniparental disomy, triplody, or a defect resulting from the fertilization of one functionally defective egg by 2 sperm;
- exposure to an infectious agent: bacteria, viruses, protozoa;
- localization of the embryo in one of the fallopian tubes.
At the same time, there are a number of factors that provoke this pathology. These include:
- pregnancy occurring in women under 18 and over 45 years of age;
- history of spontaneous abortions;
- leukoplakia of the vulva;
- history of trophoblastic diseases;
- atrophic colpitis;
- various immunodeficiency conditions;
- gestosis during late pregnancy;
- multiple births;
- thyrotoxicosis;
- consanguineous marriages.
The causes of trophoblast degeneration can be combined, thereby increasing the likelihood of its occurrence in the present and subsequent pregnancies.
Hydatidiform mole - symptoms
During gestation, pathology can be assumed by the presence of characteristic symptoms. Doctors call one of the first signs the discharge of liquid dark blood from the genital tract, which contains expelled blisters. Discharge during hydatidiform mole is always abundant and prolonged, which can lead to the development of anemia, becoming threatening to the health and life of the pregnant woman.
In the invasive form of the disease, bubbles grow into the thickness of the myometrium, resulting in a risk of uterine perforation and intra-abdominal bleeding. There are other manifestations by which hydatidiform mole can be identified - the symptoms in the early stages of this disorder are as follows:
1. Severe manifestations of toxicosis:
- nausea;
- excessive vomiting;
- salivation;
- exhaustion.
2. Increasing liver failure.
3. Lack of reliable signs of the gestation process:
- the baby’s heart sounds are not audible during an ultrasound;
- parts of the embryo's body are not found in the fertilized egg.
Diagnosis of hydatidiform mole
The diagnosis of “hydatidiform mole” is made based on the results of the studies. Initially, the doctor examines the woman in a gynecological chair. When performing this procedure, the gynecologist determines the densely elastic consistency of the uterus, in which there are areas of excessive softening. At the same time, the actual dimensions of the organ in practice exceed those that should be expected.
After an examination in a chair, if there is a suspicion of pathology, the doctor prescribes instrumental diagnostic methods:
- analysis of the level of hCG in the circulating blood;
- Ultrasound.
When diagnosing, a pathology such as hydatidiform mole is differentiated from phenomena with similar clinical manifestations:
- multiple births;
- polyhydramnios;
- pregnancy due to uterine fibroids;
- spontaneous abortion.
In order to completely exclude metastatic screenings of hydatidiform moles, doctors may prescribe additional examinations:
- chest x-ray;
- abdominal examination;
- CT;
- MRI of the brain.
Hydatidiform mole – hCG
The hCG level during hydatidiform mole is one of the indicators of the disorder. With this pathology, there is a sharp increase in the concentration of the hormone in the bloodstream. On average, it exceeds 10,0000 mmU/ml. The simultaneous increase in the size of the reproductive organ, which does not correspond to the period, prompts gynecologists to think that this may be a sign of a hydatidiform mole (hydatidiform mole).
Hydatidiform mole - ultrasound
We can detect hydatidiform mole on ultrasound in the early stages of the pathology. To confirm their assumptions, doctors conduct it immediately after receiving the result of the hCG test. Among the obvious manifestations of the disorder, doctors note the following signs of hydatidiform mole, observed on the ultrasound monitor screen:
- enlarged uterus with no fetus in it;
- homogeneous small cystic tissue (blizzard symptom);
- the presence of thecal lutein cysts in the ovaries, the diameter of which is more than 6 cm.
Hydatidiform mole - treatment
Treatment of hydatidiform mole is aimed at preventing possible complications and preserving the woman’s life. Pregnancy with such a disorder requires urgent termination. In some cases, the body independently cleanses the uterine cavity of a large number of bubbles, which come out along with bloody discharge. If this does not happen, surgery is prescribed.
It is performed under general anesthesia. If possible, doctors choose the laparoscopic method. To completely cleanse the uterine cavity from the existing embryonic membranes, curettage using a curette is used. Doctors often use vacuum aspiration to exclude the presence of residual material. In this way, complications can be prevented.
Removing a hydatidiform mole
Hydatidiform mole in the uterus can be removed in several ways. The choice of the type of surgical intervention is determined by the type of disorder, its stage, and the severity of the pathological process. For treatment, doctors use the following methods:
- Dilation and curettage.
It involves preliminary stretching of the cervix to ensure full access to the uterine cavity and removal of all the contents of the reproductive organ. This method is used for a partial form of the disorder. - Hysterectomy is the complete removal of the uterus with all its contents.
This method is used in cases of complete enlargement, expressed by the growth of chorionic villi into the deep layers of the organ. The ovaries cannot be removed during this operation.
Hydatidiform mole - treatment after curettage
In order not to cause complications that can be caused by hydatidiform mole, after cleaning the uterine cavity, the woman is monitored dynamically. A few days after the operation, an hCG test is prescribed, which is carried out twice, with an interval of 7 days. The result of therapy is satisfactory if 2 negative test results are obtained. The woman is also prescribed a physical examination of the pelvic organs, which is carried out every 2 weeks for 3 months.
Treatment of signs of hydatidiform mole
Treatment of hydatidiform mole during pregnancy depends on the individual characteristics of the course of the pathology, the period of gestation of the child, as well as the type of disease. In some cases, the fetus can be saved. However, the disease often leads to miscarriage or the need to remove the fertilized egg. If an accurate diagnosis is made, the woman is often offered to undergo minor surgery. During this procedure, curettage of the uterus is performed. The action is carried out in order to remove remnants of pathological tissue. Follow-up is then required for 8 weeks after surgery. The woman will have to undergo regular tests and ultrasound examinations every two weeks.
After the hydatidiform mole has been removed from the uterus through surgery, the level of hCG in the blood is monitored. The value of the indicator should gradually fall. This will be the main sign that the pathological processes in the uterus have stopped. If a negative hCG value is obtained, the test must be taken again. Actions are performed to ensure that the disease is truly cured. Additionally, the woman must undergo examination by a gynecologist-oncologist.
If an ultrasound shows that hydatidiform mole activity is observed, and an X-ray examination of the lungs indicates metastatic lesions, chemotherapy is administered. After remission is achieved and laboratory parameters return to normal, 2-3 additional courses are administered. The action is performed for prevention.
A patient experiencing a hydatidiform mole should be monitored by an oncologist for another year. The level of hCG in the blood is monitored monthly. It is not recommended to plan pregnancy during this period. The best means of preventing its onset are hormonal contraceptives. They allow you to normalize ovarian function after completing a course of chemotherapy and getting rid of the disease. Treatment is applied until the menstrual cycle returns completely to normal.
If there is no need for chemotherapy, and treatment was carried out in other ways, doctors recommend abstaining from pregnancy for a period of time. In other situations, the period is extended to 12 months. If conception occurs during this period, the level of hCG will certainly increase. This will lead to the fact that doctors will not be able to reliably determine the cause of the incident. It must be taken into account that hydatidiform mole can recur. The probability of this is 1-2%. However, reoccurrence of the pathology is still possible. In the vast majority of cases, the pathology does not in any way affect the ability to have a child in the future. A mother who has had the disease can give birth to a healthy child. The chance of premature birth also does not increase.
Hydatidiform mole - consequences
The consequences of hydatidiform mole can negatively affect the condition of the female reproductive system and health in general. A threatening complication of this disorder is the formation of chorionepithelioma (chorionic carcinoma) - a malignant form of trophoblast disease. It is characterized by invasive growths of the uterus, numerous metastases of areas of affected tissue to the lungs, liver, and brain. Often the pathology leads to death.
Among other consequences of hydatidiform mole, it is necessary to highlight:
- intrauterine infections;
- metrothrombophlebitis;
- thrombosis;
- amenorrhea;
- infertility.
Pregnancy after hydatidiform mole
The chances of re-conception are not affected in any way by a previous hydatidiform mole, and pregnancy after the disorder is possible. The exception is those cases when the uterus is removed due to severe destructive changes. Doctors advise not to start planning your next pregnancy immediately after a miscarriage. The recovery period lasts at least six months. During this period, hormonal medications may be prescribed. It is better to use barrier methods (condoms) as contraceptives.
Treatment
Once a diagnosis of malar pregnancy is made, a woman will not be able to carry and give birth to a baby. The exception is cases of bearing several fruits, when we are talking about twins. Then one of the fruits develops fully, and the second dies.
Most often, the pregnancy has to be terminated and the resulting cysts removed through surgery.
Surgical treatment consists of dilation and curettage of the uterus. Removal of formations occurs under general anesthesia. It is almost impossible to eliminate the entire pathological focus, but in most cases the remaining cells die off on their own. In order to speed up this process, medications such as Leucovorin, Methotrexate, Dactinomycin, etc. are prescribed. After removal, part of the altered lesion is necessarily sent for histology.
The early postoperative period includes hCG monitoring for six months. This examination is mandatory to identify a possible relapse. After all, it is human chorionic gonadotropin that indicates the completed conception, and can be released due to the presence of residual villi that have not been removed. In addition, in the postoperative period, monitoring by ultrasound of the pelvic organs and radiography of the lungs is indicated.
“Those patients who have a Rh-negative blood group in combination with partial hydatidiform mole should undergo a course of anti-Rhesus immunoglobulin,” advises the Russian Oncology Association.
Recommendations after treatment
Any patient who has undergone treatment for degeneration of the chorionic membrane must comply with the clinical recommendations of the Russian Association of Oncologists, which include:
- serum hCG test: weekly until 3 negative results are obtained in a row, then once a month for six months, and then once every 60 days for 6 months;
- radiography immediately after removal of the lesion, then after 1 and 2 months;
- Ultrasound CT scan half a month after removal of the hydatidiform mole and then every month until the level of human chorionic gonadotropin is completely normalized;
- independent maintenance of a menogram for at least 3 years.
Is pregnancy possible after a hydatidiform mole?
Many pregnant women, faced with a trophoblastic formation, and having insufficient knowledge, assume that it is cancer, and the only method of combating it is the complete removal of the genital organ and appendages.
Hydatidiform mole, both complete and partial, is a neoplasia that can be benign or, conversely, be malignant.
In fact, pregnancy after a miscarriage is possible. But when planning it, you should remember that the previously suffered trophoblast pathology is likely to make itself felt during the next pregnancy and childbirth.