What is the epidermis and why is it necessary?
The epidermis is the outer layer of the skin, consisting of several layers and cells that perform specific functions.
It includes the basal, spinous, granular, cycloid and stratum corneum. They are located above the dermis. There is constant renewal of the epidermis. This process is associated with the transformation and migration of keratinocytes from the deeper layer of the skin to the upper one. All this happens during differentiation. The epidermis contains elements of the immune system.
It performs certain functions, including:
- immune;
- protective;
- respiratory;
- receptor;
- resorption.
The most important function is considered to be protective, or barrier. The epidermis protects the body from the effects of negative environmental factors
It helps prevent dehydration. The germ layer prevents the penetration of toxins into the body and protects the body from dehydration. Cells in this layer are also able to reflect ultraviolet radiation.
It easily penetrates and damages living cells, but the stratum corneum effectively reflects it. Ultraviolet light is also absorbed by other skin cells - melanocytes. They are concentrated above the nuclei of keratinocytes and look like umbrellas. Melanosons protect not only nuclear DNA, but also the skin layer as a whole.
Treatment
In many situations, treatment of the underlying condition can restore normal skin pigmentation. Management of the benign form associated with obesity and insulin resistance conditions is based on reducing insulin levels in the circulation; Often a simple diet can significantly reverse skin damage.
Other underlying clinical conditions should be treated appropriately (as, for example, in the case of thyroid pathologies or adrenal disorders).
Microdermabrasion is an effective procedure for renewing the epidermis layer
Microdermabrasion is a mechanical peeling that is considered a safe and painless procedure. No anesthesia is required, and the recovery period is minimal. This cosmetic method helps get rid of dead skin and stimulates the formation of new cells.
Microdermabrasion is recommended for:
- Stimulates the production of elastin and collagen.
- Elimination of scars after skin diseases and postoperative scars.
- Elimination of age-related pigmentation and freckles.
- Removing stretch marks.
- Elimination of fine wrinkles in the eye and lip areas.
- Removing acne scars.
- With age-related skin changes.
- For uneven complexion and texture of the face.
The procedure also has contraindications that should be taken into account before starting:
- allergic reaction to one of the constituent components;
- inflammation of blood vessels, which is expressed in the formation of a capillary network;
- increased skin sensitivity;
- active stage dermatosis.
This method is distinguished by its effectiveness and lack of damage. Microdermabrasion can be based on the use of a peeling cream or a special device. In the first case, you need to use Abradermol cream, which has a slight abrasive effect. This procedure can be controlled without any problems.
The hardware procedure can be crystalline or diamond. The first type of microdermabrasion is based on the use of aluminum oxide microcrystals, which are fed through the tip of the device. As a result, dead skin is exfoliated, polished, and relief is restored. This method is not as safe, but it is effective.
This procedure has a milder effect. Before you start, you need to get rid of your makeup. After the procedure, a mask is made, which is selected depending on the skin type, and a cream is applied.
After microdermabrasion, scars, stretch marks are eliminated, the depth of wrinkles decreases, pigmentation becomes less pronounced, pores narrow, and the unpleasant oily sheen disappears.
During the recovery period, special care is required, which consists of following the recommendations:
- regular use of moisturizer with vitamins;
- using sunscreen or spray;
- refusal of solarium.
The number of procedures will depend on the severity of the problem and the characteristics of the skin. On average, it is recommended to conduct at least 4 sessions. The epidermis is the outer layer of the skin, which protects against the harmful effects of external factors.
If you know its structure, you can achieve noticeable positive results from cosmetic procedures. The skin is a mirror that shows what is happening to the human body, so you should not ignore any changes in it.
Article design: Anna Vinnitskaya
Prevention and tips to combat acanthosis nigricans
Maintaining a healthy lifestyle can prevent the disease from occurring in susceptible people and can also reduce the risk for many other types of diseases. Losing weight, dieting, and changing medications that trigger the disease are all important steps.
Dermatologists may also advise their patients with acanthosis nigricans to:
- Adopt a controlled and healthy diet. Obesity is the most common cause of acanthosis nigricans in adults and children. Research shows that when obese subjects lose significant body weight, spontaneous improvement in symptoms can be observed.
- Before using a whitening cream, exfoliant or other skin care product, consult a dermatologist. Some products, in addition to not having a positive effect on the hyperpigmented and thickened patches of acanthosis nigricans, can irritate the skin, worsening the condition.
DERMATITIS
Dermatitis is the general name for all forms of inflammation in the skin. It may be caused by a direct irritant effect on the skin of a pathogenic factor, an allergic reaction to substances in contact with the skin or taken orally, often with the presence of sensitization. Eczema (Greek eczema
- skin rash) is a synonym for the term “dermatitis” or a designation only for atopic dermatitis.
The main groups of dermatitis: atopic, allergic contact, seborrheic, simple irritant contact, dermatitis associated with ingestion of drugs, medications and food.
• Atopic dermatitis is a chronic recurrent inflammatory skin disease. Its manifestations are intense itching, sympathergic skin reaction, papular rashes and severe lichenification in combination with other signs of atopy. Histological examination of new lesions reveals acanthosis, edema of the dermis, and sometimes spongiosis and exocytosis (Fig. 25-6). In the dermis there are perivascular, often confluent infiltrates of lymphocytes with an admixture of neutrophilic granulocytes (Fig. 25-7). In old lesions there is hyperkeratosis and parakeratosis, in the dermis there is dilation of capillaries with swelling of the endothelium. In the vascular area, infiltrates of lymphocytes and histiocytes are visible; in the chronic course, fibrosis predominates. In old lesions the amount of melanin is increased.
Rice. 25-6. Eczema is acute. A lesion of the epidermis (erosive surface) with the formation of a crust (preparation by L.V. Lysenko and A.I. Lysenko). Hematoxylin and eosin staining (x200).
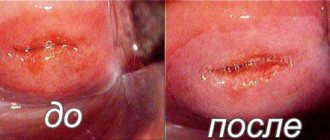
Can pseudo-erosion of the cervix pose a danger?
The disease poses a threat to the health and life of women. If focal keratosis is not detected during the procedure, the consequence is cervical atrophy. The estrogen hormone is reduced, the epithelium is suppressed, the tissue is smoothed out. Atrophic vaginitis is a common phenomenon. Postmenopause is one of the reasons.
Cervical atrophy causes infertility and cervicitis, which is characterized by purulent discharge, pain during intercourse and urination. The uterine pharynx and vagina have an inflammatory process that is often neglected. If a couple wants to have a child, then first it is necessary to cure cervicitis, otherwise the child may be born with developmental disabilities.
But the most dangerous is dyskeratosis. Over a short period of time, uncontrolled growth of tumor cells can occur. Human papillomavirus (HPV) and HIV infections are important; they increase the risk of cells degenerating from benign to malignant.
Authors | Last updated: 2019
Gynecological diseases occupy a leading position among women among all visits to doctors. Up to 15% of the fair sex have cervical erosion, which can be true, congenital or pseudo-erosion.
Pseudoerosion of the cervix (its other names are ectopia, endocervicosis) is more common in women aged 20–40 years. Before the onset of puberty, this process is considered physiological and requires only medical supervision. Treatment is prescribed for a progressive form of the pathology or in case of complications.
There is no ICD-10 code for cervical ectopia. According to the conclusion of the VII International Congress, which was held in Rome in 1990, this condition was classified as a group of normal colposcopic findings. However, this applies only to uncomplicated forms of pseudo-erosions.
After 40 years, cervical ectopia does not occur. The pathology affects women during the reproductive period, of which 50% of cases occur under the age of 25 years.
A little anatomy
The cervix (cervix) is the lower segment of the uterus. Conventionally, it can be divided into several parts:
- Vaginal, which is visualized when examined in mirrors;
- Supravaginal, which is not visualized;
- The isthmus, or the junction of the cervix and the uterus.
There are 2 pharynxes in the cervix:
- External, visible on the vaginal part of the organ;
- Internal, which passes into the uterine cavity.
The cervical canal passes through the pharynx, opening into the vagina on one side and into the uterine cavity on the other.
Normally, the vaginal part of the cervix is covered with squamous epithelium, and the cervical canal is lined with columnar epithelium.
The cervix is located between the vagina and the uterus, it is 2-3 cm long. Upon examination, only part of the cervix is visible; it is lined with multilayered squamous epithelium, and the cervical canal (the hidden part of the cervix) is single-layered cylindrical.
When the columnar epithelium shifts outward and replaces the flat epithelium, cervical pathology develops. Depending on the woman’s age and the reasons that caused the development of the pathological process, a diagnosis of congenital erosion or pseudo-erosion of the cervix is made.
Pseudo-erosion of the cervix is a displacement of the columnar epithelium onto the vaginal part of the cervix. Ectopia can be caused by a variety of conditions, including infections, injuries, and changes in the immune system. Pathology can also occur against the background of true erosion in the absence of timely therapy.
True erosion is characterized by thinning of the squamous epithelium on the vaginal part of the cervix, which leads to the formation of cracks and ulcers on it. If therapy is not started in a timely manner, epithelium from the cervical canal begins to creep onto the damaged mucous membrane.
In the case of pseudo-erosion, a gynecological examination visually reveals a zone of hyperemia located near the cervical canal. It has no clear boundaries and can occupy an area of 1 mm to 2 cm.
Ectopia is a displacement of the columnar epithelium onto the vaginal surface of the cervix.
With ectopia of the cervix, a transformation occurs over time - the transition of columnar epithelium to flat. This phenomenon is called squamous metaplasia. The transition process occurs in the transformation zone, which requires increased attention from a specialist.
On a note
Up to 90% of all cases of cervical cancer occur in the transformation zone. Malignization (malignancy) of ectopia occurs very rarely, but it cannot be completely excluded. Observation by a gynecologist is required.
Types of cervical pseudo-erosion are classified according to:
- Origin;
- Changes in tissue structure;
- The nature of development.
Pseudoerosions are classified according to their origin:
- Congenital, which is associated with the anatomical feature of the structure of the female genital organs;
- Dishormonal, occurring when the hormonal status of the female body changes;
- Post-traumatic, which appear when the cervix is injured as a result of medical procedures, improper douching, or during active sexual intercourse.
According to the structure of changes, the following types of ectopia are distinguished:
- Glandular. In this case, against the background of the proliferation of cylindrical epithelial cells, glands that produce mucus are formed;
- Papillary. Accompanied by the formation of connective tissue growths at the site of the pathological process. In appearance it resembles warts;
- Metaplastic, or glandular-cystic. At the site of erosion, squamous epithelial cells grow into several layers. As a result of layering, the glands become clogged, making it impossible for mucus to flow out of them. Over time, the glands become swollen and may become inflamed. This is how Nabothian cysts are formed;
- Glandular-papillary. It is mixed, with a combination of signs of papillary and glandular erosions;
- Cystic. Accompanied by the formation of cysts with mucus. Often accompanied by epidermization.
A Nabothian cyst develops when the ducts of the glands of the cervix are blocked.
Epidermal pseudo-erosion causes the development of inflammatory reactions. Ectopia in combination with chronic cervicitis is a factor in the development of a complicated form of the pathological process.
According to the nature of development, endocervicosis is:
- Progressive. The pathological process goes through all stages of changes in the structure of the cervical tissue. Often accompanied by the development of inflammatory processes;
- Stationary. After the formation of Nabothian cysts, regression of the pathological process is observed with complete restoration of the squamous epithelium at the site of the lesion. Cysts with a diameter of up to 3 mm remain in the cervix. The cervix is deformed and hypertrophied;
- Healing. The structure of the cervical tissue is completely restored without deformation.
Forms of ectopia
By development time:
- Congenital - determined at the first visit to the gynecologist;
- Acquired - appears over time.
According to the nature of the flow:
- Uncomplicated – not accompanied by complaints or progression;
- Complicated – accompanied by the development of inflammatory reactions in the cervix;
- Recurrent – occurs again after therapy.
Complicated pseudo-erosion of the cervix can become malignant, which requires immediate treatment.
The etiology of cervical pseudo-erosion depends on whether this change is congenital or acquired.
Congenital endocervicosis is most often associated with improper formation of the genital organs in utero or during their further development. During puberty and pregnancy, the condition is physiological against the background of relative hyperestrogenism.
The acquired form occurs as a result of the close interaction of external and internal factors and accounts for up to 80% of all cases of pseudo-erosions.
External factors
Among external factors, the most important ones are:
- Damage to the mucous membrane of the cervix of a bacterial or viral etiology;
- Traumatization of the cervix during sexual intercourse, including barrier methods of contraception (condoms, vaginal caps, etc.);
- Cervical injury during childbirth or abortion.
Due to damage to the cervical mucosa by various pathogenic microorganisms, cervicitis can develop, which in turn can cause erosion.
Internal factors
Among the internal factors that provoke the appearance of pseudo-erosion are:
- Hormonal imbalance, which can be either a manifestation of an independent disease or a concomitant pathology;
- Chronic diseases of the genitourinary organs with frequent exacerbations and accompanying disorders of the immune system.
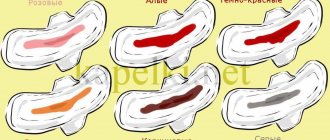
Uncomplicated forms of cervical ectopia are asymptomatic. Most often, endocervicosis is a finding during a gynecological examination. However, up to 80% of cases are complicated pseudo-erosion. It is characterized by:
- The appearance of yellowish discharge from the genital tract;
- Changes in the menstrual cycle (lengthening or shortening, irregularity) with concomitant hormonal disorders;
- Painful menstruation;
- Bloody discharge from the genital tract between menstruation;
- Bloody discharge and pain during intercourse.
Discharge from ectopic cervix indicates the onset of the inflammatory process.
Often complicated ectopia can be detected in combination with other gynecological pathologies:
- Infertility;
- Polyps;
- Cysts;
- Tumors.
Diagnosis of cervical ectopia begins during an examination in a gynecological chair. An area of hyperemia around the cervical canal, which has a blurred border, is visually determined. To determine the condition of the cervix, smears are taken on:
- Flora of the genital tract;
- Oncocytology.
Based on the analysis of the cytogram for uncomplicated ectopia, the following conclusion can be given:
- Without features. Squamous epithelial cells are identified;
- Proliferation (cell reproduction) of columnar epithelium;
- Endocervicosis.
In case of a complicated course, the following cytogram picture is possible:
- Inflammation;
- Leukoplakia, or dyskeratosis;
- Dysplasia I, II or III degrees.
SKIN CHANGES IN CONNECTIVE TISSUE DISEASES
Autoimmune diseases play an important role in the structure of skin diseases. In the pathogenesis of immunological disorders in focal scleroderma and subacute cutaneous lupus erythematosus, the main factor is combined violations of the effector and regulatory components of immunity. One of the main immunological defects is an imbalance between the activity of T helper cells - Th1 and Th2 cells, involved in the reactions of cellular and humoral immunity, respectively. This leads to the generalization of the process and the transformation of cutaneous forms of autoimmune pathology into systemic ones.
Unlike lupus erythematosus, the complexity of the course of focal scleroderma is due to a switch from the Th1 pathway to a Th2-dependent immune response, leading to the development of a group of immunopathological reactions in patients. Disruption of the interaction between the immune and connective tissue systems is one of the main factors determining the pathogenesis and clinical picture of these forms of autoimmune diseases.
LUPUS ERYTHEMATOSUS
The manifestations and pathogenesis of systemic lupus erythematosus are described in detail in chapters 6, 10, 15, 16. In addition to systemic lupus erythematosus, there is a cutaneous form, it is called discoid (chronic) lupus erythematosus. Skin changes in both variants of the disease are similar.
Discoid lupus erythematosus ( Lupus erythematodes
) - limited erythematous lesions on the face, ears, scalp, red border of the lips. Favorite localization is the area of the naso-cheek folds (“butterfly phenomenon”).
Etiology
The key cause of parakeratosis is the development of human papillomavirus (HPV) in the body. With the active progression of papillomavirus infection, pathological changes occur in the structure of cells:
- multiple nuclei;
- hyperkeratosis;
- dyskeratosis;
- koilocytosis.
Cellular and tissue changes in the mucous and epithelial layer of the cervical canal can be provoked by the following factors:
- frequent abortions;
- progesterone deficiency;
- cervical erosion;
- dysfunction of the gonads;
- pseudo-erosion of the cervix;
- vaginitis;
- curettage of the uterus;
- ingrowth of the intrauterine device.
Also among the provocateurs of keratinization of uterine tissue are secondary immunodeficiencies and nervous exhaustion. The true cause of the development of parakeratosis can only be determined through laboratory and hardware examination.
INFECTIOUS AND PARASITIC DISEASES OF THE SKIN
The barrier function of the skin can be disrupted by microorganisms and parasites. With unstable immunity, even abscesses, carbuncles or boils can be life-threatening.
Main infectious and parasitic skin diseases.
• Bacterial infections: skin abscess, boil, carbuncle, impetigo, acne vulgaris, leprosy.
• Viral infections: viral warts, molluscum contagiosum.
• Fungal infections.
• Parasitic skin diseases (scabies).
VIRAL INFECTIONS
Viral warts
(
verruca
). Transmission of the agent usually occurs through direct human contact or self-infection. The resulting papules can disappear spontaneously over a period of 6 months to 2 years.
An ordinary (vulgar) wart can appear anywhere, most often on the skin of the hands, especially on the back surfaces and in the periungual areas. Here the warts look like gray-white or red flat and convex papules with a diameter of 0.1-1 cm with a rough surface. In addition, there are plantar and palmar warts.
Genital wart
(genital condyloma, venereal wart) develops in the skin of the penis, female genital organs, inguinal and intergluteal folds. A genital wart is a soft reddish or pinkish exophytic formation with a papillary surface resembling a cauliflower. In some cases, these formations are multiple and can reach several centimeters in diameter.
The histological feature of all types of warts is epidermal hyperplasia. In the cytoplasm of the epithelial cells of the superficial layers of the epidermis (the upper part of the spinous and granular layers) there are no keratohyalin granules, but vacuolization is noted - koilocytosis. Cells affected by the virus with a light halo around the nuclei are called koilocytes. Electron microscopy reveals numerous viral particles inside the nuclei of koilocytes. Warts are also characterized by acanthosis and hyperkeratosis. In the basal layer of the epidermis, a large amount of melanin is sometimes noticeable. As a rule, there are no changes in the dermis, but sometimes mononuclear infiltration and exocytosis occur. Severe swelling of the dermis with vasodilation and focal inflammatory infiltrates are characteristic mainly of genital warts.
Acanthosis CMM how to treat
Acanthosis of the cervix is a thickening of the mucous membrane of the cervical canal; the disease is precancerous and requires immediate treatment. The disease develops under the influence of both external and internal factors - hormonal disorders, physical fatigue, impaired immune function, infectious diseases of the genital tract.
In some cases, the affected areas cover a significant part of the epithelium, but in the initial stage the disorders are of a point nature. They are easy to notice with the help of a colposcope; when the suspicious area is stained with iodine, it does not react to the substance and remains unstained, while neighboring tissues change color.
Signs of acanthosis include an unpleasant odor and bloody discharge after sexual intercourse.
Cervix with parakeratosis, which is caused by nonspecific causes, is treated with medications and local procedures - ointments, suppositories. A specific bacterial infection is treated with antibiotics. The papilloma virus has no cure, but is controlled by taking vitamins to strengthen the immune system.
For acanthosis, surgical treatment is indicated if there is a high risk of malignant degeneration.
The impact of chemical peels at the level of different layers of the epidermis
Chemical peeling is damage to the upper epidermal layers using various chemical agents that help in correcting imperfections in appearance.
Alpha hydroxy acid (AHA) and beta hydroxy acid (BHA) medications may be used during the procedure. AHAs include lactic, mandelic and glycolic acids. BHA includes salicylic acid.
| Types of peeling procedures | a brief description of |
| Surface | It is carried out using ANA. Recommended for increased skin pigmentation. It does not have a strong effect, so after the procedure the defect does not go away, but becomes less pronounced. The main purpose of this peeling is to get rid of dead skin particles and refresh the skin color. The procedure is gentle. To achieve noticeable results, a course is required. Superficial peeling does not require anesthesia. The procedure is not traumatic. Can be done at any age. Affects only the upper layers of the epidermis. |
| Average | This peeling is based on the use of stronger acids that reach the middle layers of the epidermis. The procedure significantly reduces the severity of pigmentation, helps smooth out scars, and eliminates fine wrinkles. Advance preparation is required. This type of peeling completely removes the stratum corneum of the skin; as a result, after the procedure, a crust forms, which goes away in 5-7 days. The recovery period can be more than 2-3 weeks. The procedure is recommended for patients aged 25 to 35 years. |
| Deep | It is considered a dangerous procedure. Based on the use of highly concentrated acids or phenol. The recovery period can last more than six months. If the procedure is performed incorrectly, scars may form. Copes with medium and deep wrinkles. Damages all layers of the epidermis. This type of peeling is recommended for middle-aged patients. It is performed in a hospital setting and requires pain relief. Currently used extremely rarely, as safer and more effective procedures exist. |
Preliminary preparation of the skin is required, the process of which is determined by the cosmetologist. She starts 2 weeks before the peel. Preparation is based on the use of AHA 5% cleansing gel with glycolic acid. The use of the gel is carried out gradually. At first it is used 1 time per day, gradually increasing to 2 times.
Before peeling, you need to cleanse the skin of makeup. Carry out degreasing with special means that normalize the acid balance. Then the active substance is distributed over the face and then removed.
The procedure ends with treating the skin with a post-peeling agent that neutralizes the acid. A burning sensation may be present. The layers of the epidermis of human skin are necessarily damaged during peeling, and to what extent will depend on the type of procedure that is selected by the cosmetologist, and on the age category of the patient, the condition of the skin, and phototype.
What is parakeratosis? Symptoms of the disease
Cervical parakeratosis is distinguished by the form of manifestation and the cause of its occurrence. There is an opinion that with a lack of the microelement zinc, the risk of this pathology increases. With various skin diseases, keratosis may develop in the cervical canal as a concomitant process.
Most often, parakeratosis of the cervical epithelium begins in the presence of a viral infection. It may be an oncogenic human papillomavirus (HPV). As a result of exposure to toxic substances produced by the virus, the body's defenses are reduced, and it is not able to perform the work of exfoliating the upper layer of squamous epithelium in the cervical canal. Therefore, the layers accumulate one above the other, forming areas of dense keratinization; such areas have minimal ability to stretch, which leads to damage and bleeding. The appearance of blood after sexual intercourse is especially noticeable.
Other infections that can cause keratinization of the squamous epithelium:
- chlamydia;
- ureaplasma;
- genital herpes;
- mycoplasma;
- cytomegalovirus infection.
As a result of keratinization, scales that do not contain glycogen appear, which is typical for women during menopause, when the amount of starch in epithelial cells decreases.
Nonspecific vaginitis and cervicitis can also contribute to the development of parakeratosis. Ectopia, when tissue shifts and the inside of the cervical canal is visible in the center of the cervix, can also cause the disease. About 80% of malignant cell degeneration occurs at the tissue junction.
A special type of keratosis is atopic. If you have an allergy, disorders can occur in unusual places, the squamous epithelium of the cervix is no exception, this situation is rare, but this possibility should not be excluded.
Treatment of erosion in the old way, using diathermocoagulation or cauterization, is a procedure that destroys the epithelial layer. After they are carried out, symptoms of hyperkeratosis may appear after some time.
The structure of squamous epithelium is normal
Normally, the mucous membrane is pink and uniform in color and structure. Hyperkeratotic changes appear as dense white structures of various shapes on the cervix and on the mucous membrane lining the cervical canal. This is the initial stage of leukoplakia, which poses a danger to the health of women of reproductive age. With leukoplakia and parakeratosis, there is a risk of degeneration into squamous cell carcinoma. The peculiarity of this pathological process is its asymptomatic course. Women rarely pay attention to minor discharge, and upon examination by a gynecologist, lesions of the stratified squamous epithelium are discovered, which can spread to the cervix area.
Flat epithelium consists of 4 layers:
- surface;
- intermediate;
- parabasal;
- basal.
As a result of changes in the morphology of the epithelium - the absence of a granular layer, thickening of the stratum corneum - the production of keratohyalin (the precursor protein of keratin) is reduced, which affects the functioning of the entire epithelium.
ACUTE AND CHRONIC DERMATOSES
Dermatoses are the main group of skin diseases. The role of infectious agents in their occurrence is usually small.
HIVES
Urticaria ( urticaria)
) - a sudden widespread rash on the skin of itchy, edematous plaques surrounded by a zone of arterial hyperemia, followed by the formation of blisters. In most cases, urticaria is a consequence of degranulation of mast cells and the release of vasoactive mediators from their granules.
Urticaria is characterized by swelling that affects the deep layers of the dermis and subcutaneous fat. According to epidemiological studies, 10-30% of the population experiences one case of urticaria during their lifetime. Focal changes appear and disappear within a few hours (usually less than 1 day). Occasionally they remain for several days, weeks or even months. Externally, the lesions range from small itchy papules to large, edematous plaques. It is possible for them to merge to form angular, linear or arched shapes. Urticaria rashes are most often located on the skin of the torso, distal extremities and ears. Persistent forms of the disease may reflect a failure to clear the antigen that causes urticaria or may be a complication of the underlying disease.
The histological features of urticaria are sometimes so subtle that in many biopsies the pattern is identical to normal skin. More often, perivenular infiltrates of mononuclear cells and rare neutrophils are detected in the superficial layers of the dermis. Eosinophils can be found in such infiltrates (especially in the middle parts of the dermis). Collagen fibers appear more disjointed than in normal skin, indicating swelling of the dermis. The edema fluid in histological preparations is not colored. Superficial lymphatic vessels are always dilated.
Cervical parakeratosis: signs, symptoms, diagnosis and treatment
Cervical parakeratosis is a condition that is manifested by pathological keratinization of the integumentary epithelium of the cervix.
This phenomenon is not typical for a healthy organ; a relative exception is pseudoparakeratosis, in which keratinized cells can appear as a result of degenerative processes in endocervical smears in the second half of the cycle, as well as in the postmenopausal period.
Regular visits to the doctor will allow you to identify pathology at an early stage
What is parakeratosis in terms of etiology? This pathology is considered as a consequence of active inflammatory processes, as well as injury to the cervical canal during childbirth, abortion, and surgical interventions.
It should be noted that this condition is background, that is, under some circumstances it can provoke dysplastic changes in tissues, which threatens cancer pathologies.
Therefore, when parakeratosis is detected, therapeutic measures should be taken immediately.
Essentially, parakeratosis is a failure in the process of keratinization of the mucous membrane of the cervical canal. The condition is not an independent disease; it is a symptom of some pathology of the cervix.
Parakeratosis manifests itself as incomplete keratinization, but in the absence of adequate therapy it can transform into hyperkeratosis, that is, increased keratinization. In this case, the upper layer of the mucous lining of the cervix becomes keratinized, and the foci of the pathological process in structure represent several epithelial layers that have not undergone desquamation.
Both parakeratosis and hyperkeratosis are characterized by the following symptoms:
- there is no granular layer;
- the stratum corneum is thickened;
- rod-shaped nuclei are detected in the cells.
The progression of the pathological process provokes a decrease in tissue elasticity, while the lesions have a rough, wrinkled appearance.
Parakeratosis is a characteristic sign of a disease such as cervical leukoplakia. It is defined as precancer, so detection of this disease requires immediate initiation of treatment.
There are two types of parakeratosis: focal and superficial. The superficial version involves the involvement of a small area of the epithelium in the process, while it is not invasive. This type of pathological condition requires observation, but is rarely dangerous.
Erosion: why it is dangerous and its causes
In addition, the focal variant of the condition is also characteristic of dysplastic lesions. In cervical intraepithelial neoplasia (CIN), areas with parakeratosis are identified in the early and late stages.
Visually, pathological lesions are defined as flat white spots with a matte tint. A common location is the mucous membrane of the vaginal portion of the cervix, a rare location is the depth of the cervical canal. Women of childbearing age are most susceptible to progression of the condition.
Human papillomavirus
The main etiological factor of parakeratosis is the presence in the body of the human papillomavirus, which is a highly oncogenic type. Activation of infection by this virus provokes cellular changes in the form of pathological and excessive keratinization, disrupted structure of the nuclear apparatus of cells (multiple nuclei, koilocytosis).
Some other factors also contribute to the progression of the condition, namely:
- traumatization of the cervix during childbirth, abortion, curettage, installation of an intrauterine device, and other manipulations;
- therapy for cervical erosion;
- inflammatory diseases, including those caused by sexually transmitted infections;
- hormonal imbalance (insufficient production of progesterone);
- ovarian dysfunction;
- the presence of foci of ectopia.
The specific cause is determined during a complete examination of the patient.
The following are considered as additional provocateurs of pathology:
- weakened immune system;
- exhaustion of the nervous system;
- overwork of the body;
- reduced resistance.
Symptoms of keratosis
Parakeratosis and hyperkeratosis are often asymptomatic; as a result, the woman may not be aware of the existence of the problem. Therefore, regular preventive examinations are so important, which help to identify pathologies that occur without symptoms or with a small number of them.
In a number of situations, symptoms can be erased due to the presence of active symptoms of a provoking pathology, most often of an infectious-inflammatory nature.
The following symptoms can help you suspect a problem:
- discomfort during sexual intercourse;
- small amounts of spotting after sex;
- excessive production of vaginal secretions, which may have an unpleasant odor.
Why does a cyst form on the cervix, why is it dangerous?
The presence of such symptoms should be a reason for mandatory contact with a gynecologist. The doctor will conduct an examination, prescribe additional diagnostic measures, make a diagnosis and determine the direction of the course of therapeutic correction.
Histological examination of a biopsy specimen is an important diagnostic step.
In addition to a gynecological examination, the following diagnostic measures may be needed:
- Schiller's test.
- Colposcopy in extended format.
- Biopsy followed by histological examination of the biomaterial.
- Examination of smears for flora.
- Examination of blood and secretions for sexually transmitted infections, including the human papillomavirus.
- Analysis of hormonal levels.
- Analysis of immune status.
The results of these diagnostic techniques will allow the doctor to make a diagnosis and determine treatment tactics.
If cervical parakeratosis is detected, treatment should be selected on an individual basis, based on the characteristics of a particular clinical case. The degree of the pathological process, the patient’s age and her general health are taken into account. Self-medication is unacceptable and impossible; the condition must be corrected according to prescriptions and under the supervision of a doctor.
Conservative therapy involves eliminating the factor provoking the problem. Treatment of bacterial and viral infectious diseases, vaginal dysbiosis is prescribed. Measures are taken to improve the functioning of the immune system.
Invasive techniques are advisable in cases where the process is widespread and the presence of neoplastic changes.
To prevent parakeratosis, it is recommended to regularly visit a doctor for preventive purposes. Vaccination against human papillomavirus infection is also recommended.
Cervical parakeratosis is not a separate nosology; a doctor will never make such a diagnosis. Actually, the term parakeratosis refers to increased division of epithelial cells with retention of nuclei in the stratum corneum. With pathology, the elasticity of the cervical tissue changes, and areas of the mucous membrane look rough and wrinkled.
Parakeratosis is characterized by the presence in the surface layer of multiple layers of small compact cells such as miniature superficial ones with pyknotic nuclei. Parakeratosis itself has no clinical significance, but the fact that parakeratosis of the cervix may be an indirect sign of some dangerous diseases is of concern.
Among them:
- viral tissue damage;
- leukoplakia - the process of formation of white plaques on the mucous membrane of the cervix, which are often associated with the presence of atypical cells, precursors of cancer;
- in fact, dysplasia and cancer, which are often hidden behind parakeratosis, subsequently spread to the body of the uterus.
Often parakeratosis is manifested by focal lesions of the cervical mucosa, which the doctor first identifies during a gynecological examination and may mistake for cervical erosion.
There are no specific symptoms that would clearly indicate the presence of a focus of pathology, but the following complaints may appear accompanying parakeratosis:
- an increase in the amount of discharge from the genitals;
- unpleasant smell of secretion;
- the appearance of itching and burning in the genital area;
- suspicion of exacerbation of chronic diseases of the uterus!;
- feeling of discomfort during sexual intercourse;
- spotting after sexual intercourse.
Inflammatory diseases of the genital organs become one of the leading causes of cellular changes. They are diagnosed in almost 70% of women who come to see a specialist at our gynecological clinic on Tsvetnoy Boulevard. What is dangerous is that clinical manifestations of inflammatory processes in the vagina and cervix often have a hidden, long-term asymptomatic course, which in turn creates difficulties in treatment and preconditions for the development of relapses. During the entire time a woman does not see a doctor, pathogenic microorganisms negatively affect the adjacent tissues of the uterus!
Often, the risk of inflammation with an increased likelihood of damage to the mucous membrane of the cervix, as well as carcinogenesis, including the uterus, is associated with infectious diseases, which has been proven by scientists in numerous studies.
Among the possible infectious agents often associated with cellular degeneration, including oncology, there are pathogens that are sexually transmitted infections (STIs), including trichomonas, chlamydia, herpes simplex virus type 2 (HSV-2), papilloma virus human (HPV, the most dangerous are HPV 16, HPV -18, HPV-31).
By the way, viruses are currently the main infections detected in women and leading to problems with reproductive health. They are inferior in frequency of detection to syphilis and gonorrhea. Particularly alarming is the fact that up to 600 thousand cases of cancer associated with HPV are registered annually in the world.
When infected with this virus, women may experience papillomatosis affecting the periuterine area. Often, condylomas are located in the thickness of the tissue lining the cervix and are detected when pronounced foci of keratinization develop, which requires differential diagnosis directly with parakeratosis. It is important to note that these manifestations can also be combined.
EPITHELIAL TUMORS
BENIGN EPITHELIAL TUMORS
These processes are widespread in the skin. They can arise from stratified squamous keratinizing epithelium, keratinocytes of hair follicles, and the lining of the ducts of the skin appendages. To establish a diagnosis, histological examination of biopsy specimens is necessary.
Seborrheic keratosis is a common disease characterized by numerous round, flat epidermal pigmented superficial plaques ranging from a few millimeters to several centimeters in diameter. Plaques most often appear in middle age or old age on the skin of the trunk, extremities, head and neck. Formations in seborrheic keratosis are built from complexes of small cells, similar to the cells of the basal layer of the normal epidermis and containing varying amounts of melanin in the cytoplasm. Characterized by hyperkeratosis, small keratin-filled cysts (horny cysts) and signs of keratin penetration into the bulk of the tumor (pseudoridal cysts).
Acanthosis nigricans ( acanthosis nigricans)
) - thickening and hyperpigmentation of the skin of the neck, armpits, external genitalia, perineum, anus and inguinal-femoral folds. It is believed that acanthosis nigricans is a diagnostically valuable skin marker of combined benign and malignant neoplasms. The reason for its appearance is the abnormal production of factors that stimulate epidermal growth by tumors.
Pathomorphological processes.
The physiological property of the epithelium of the oral mucosa is the process of keratinization. There are several conditions corresponding to a disruption of the normal keratinization process: parakeratosis, keratosis, hyperkeratosis, leukokeratosis, acanthosis, dyskeratosis.
Parakeratosis
- defective keratinization, when keratin appears in the protoplasm of the cells of the surface layer, but nuclei are still present. Epithelial cells lose the ability to produce keratohyalin, the connection between individual cells is disrupted, loosening of the stratum corneum, partial or complete disappearance of the granular layer are histologically determined. Parakeratosis is a normal condition in most areas of the oral mucosa and is classified as a pathological process in the keratinizing squamous epithelium.
Keratosis
- a clinical concept that unites a group of diseases of the skin and mucous membrane of a non-inflammatory nature, which are characterized by thickening of the keratinizing layer and the formation of the stratum corneum.
Hyperkeratosis
- a significant increase in the stratum corneum compared to its thickness in keratosis. During this process, a granular layer develops. In the literature, the term “leukokeratosis” is used to designate a white area of hyperkeratosis.
Acanthosis
- a histological term characterizing the thickening of the epithelium due to increased proliferation of the basal and spinous layers. The process is accompanied by lengthening of the interpapillary processes of the epithelium and their more pronounced growth into the connective tissue.
Dyskeratosis
- a pathological process in which dyskeratinization and degeneration of the cells of the spinous layer occurs, cell dysplasia is observed, the connections between them are disrupted, and the cells are located chaotically.
Granulosis
- an increase in the number of rows of the granular layer or the appearance of a granular layer where it should not be.
Papillomatosis
- proliferation of interepithelial connective tissue papillae, which can reach the surface of the stratum corneum.
Hyperkeratosis, granulosis, acanthosis and papillomatosis are pathomorphological processes of a proliferative nature.
Inflammatory infiltration
- a pathomorphological process characterized by the accumulation of cellular elements of blood and lymph in the actual mucous layer; accompanied by local compaction and an increase in tissue volume.
Acantholysis
- a pathomorphological process based on autoimmune mechanisms. Histologically, melting of intercellular connections is observed in the spinous layer; the cells become rounded, become much smaller in size and become separated, i.e. intraepithelial blisters form.
Vacuolar degeneration
- accumulation of fluid in the form of vacuoles inside the cells of the basal or spinous layer, which contributes to the formation of vesicles.
Ballooning degeneration
- focal changes in the cells of the spinous layer associated with the accumulation of fluid in them. As a result, the cells take on the appearance of “balls” or “balloons”, significantly increase in size, and separate, forming cavities filled with exudate. The presence of multinucleated “giant” cells is recorded.
Spongiosis
- intercellular swelling of the spinous layer. The process is characterized by local expansion of intercellular tubules due to the entry of exudate from the underlying mucous membrane itself, intercellular connections are broken and bubbles form.
General symptoms of the disease
With acanthosis nigricans in a person, the clinic will be as follows:
- compaction and peeling of individual areas of the epidermis;
- the appearance of hyperpigmentation (brown-black spots);
- formation of papillomas or fibromas (popularly such neoplasms are called warts).
Where are the following skin manifestations observed:
| Place | Photos of symptoms |
| In the armpits | |
| On the neck | |
| Under the knees | |
| On the elbows |
This disease also occurs in the groin, gluteal area, thighs, and near the mammary glands (in women). But not so often.
Even less commonly, signs of the disease may appear near the navel and on the face. In especially severe cases, damage to the mucous membranes, esophagus, rectum and vagina is noted.
First, in a sick person, individual areas of the epidermis turn yellow, which gradually become darker. Outwardly, it looks like banal pollution.
That's why many people try to wash it off. But, if you do not resort to appropriate treatment, the disease progresses. As a result, the skin becomes rough and constantly flakes, and pigmentation intensifies.
In the final stages, the skin becomes covered with small papillary-shaped compactions, sometimes also black. Their accumulation is quite large.
When the lesion affects the mucous components of pigmentation, no pigmentation is observed, but the formation of papillomas is likely.
The mucous membranes are covered with small villi and shallow grooves. If the disease affects the tongue, it becomes excessively wrinkled.
Family doctor Mohammed Ahmad
It is rare, but it happens when all these symptoms are accompanied by itching and tingling. The affected areas also lose hair.
It is important not to ignore any of these signs, since detecting this disease in the early stages makes treatment easier.
SKIN PIGMENTATION DISORDERS
This pathology is manifested by a decrease or increase in the amount of melanin. In addition, melanocytes can become the source of a malignant tumor - melanoma.
Melanocytes are located in the basal layer of the epidermis, their number varies in different areas of the skin. In their predecessors - melanoblasts, under the influence of tyrosinase in special organelles - melanosomes, the pigment melanin is synthesized from tyrosine through a series of intermediate stages. In melanosomes, melanin is released into the extracellular space, where it is taken up by keratinocytes. In these cells, lysosomal enzymes break down melanin. The main purpose of melanin is to protect underlying tissues from ultraviolet radiation. Skin color (including the intensity of tanning in people with white skin) is associated not so much with the number of melanocytes, but with the melanin content in them.
• Albinism (leukoderma) is a disease with an autosomal recessive type of inheritance, in which the synthesis of melanin in melanoblasts does not occur due to the absence of tyrosinase. Albinos have blond hair, pale skin and pink eyes.
• Vitiligo is a pigmentation disorder with the appearance of milky-white depigmented macules on the skin. Vitiligo lesions are characterized by loss of melanocytes. Probable reasons for this: autoimmune destruction or the formation of toxic intermediate products of melanogenesis that destroy melanocytes, skin inflammation (with leprosy, syphilis), burns, etc.
• Freckles are small (1-10 mm) reddish or light brown macules that first appear in early childhood after sun exposure. Hyperpigmentation is caused by an increased amount of melanin in the keratinocytes of the basal layer of the epidermis.
Diagnostics
Often visiting a doctor with cervical hyperkeratosis, a woman hears a result such as a cytogram corresponding to hyperkeratosis of the squamous epithelium. This indicates the presence of the disease and the appearance of one or more white spots on the epithelium of the cervix, indicating layering of the epithelium.
Also, against the background of the disease, the presence of a benign tumor (dermatofibroma) is often detected. In such cases, patients are interested in the question of what dermatofibroma with hyperkeratosis of squamous epithelium means. When diagnosing the disease, the identification of benign formations is not uncommon.
Diagnosis of the disease is carried out using the following methods:
As a result of the research, single accumulations of scales or multiple formations are detected on the surface of the mucous membrane of the cervix. After making a diagnosis and identifying the provoking causes, it is necessary to begin treatment. In such cases, the pathology will have a positive prognosis.
Important! Timely detection of the disease and proper treatment will help avoid complications of the pathology in the future.
PAPULOSQUAMOUS DISORDERS
The main diseases of this group according to the WHO classification are psoriasis, parapsoriasis, and lichen planus.
PSORIASIS
Psoriasis is a chronic relapsing dermatosis caused by many factors. The skin is characterized by a rash of epidermal-dermal papules with profuse peeling. In various countries, 1-3% of the population suffers from psoriasis. With psoriasis, joints, as well as various organs and systems of the body, may be involved in the process.
Clinical and morphological forms of psoriasis: gypsum, vulgar, psoriatic erythroderma, as well as exudative (pustular).
Most often, psoriasis affects the skin of the elbows, knees, scalp, lumbosacral region, intergluteal gap and glans penis. The most typical focal change is a well-defined pink or orange-pink plaque covered with easily removable silvery-white scales. The pink color of the rash is called Pilnov's symptom. When papules are scraped, a triad of signs characteristic of psoriasis consistently appears: stearin stain (the surface of the papule acquires a white stearic color), terminal film (reddish shiny surface after removal of scales), pinpoint bleeding after removal of the film (Polotebnov's blood dew phenomenon, or Auspitz's symptom).
How to treat parakeratosis
If cervical parakeratosis is detected, treatment should be selected on an individual basis, based on the characteristics of a particular clinical case. The degree of the pathological process, the patient’s age and her general health are taken into account. Self-medication is unacceptable and impossible; the condition must be corrected according to prescriptions and under the supervision of a doctor.
Conservative therapy involves eliminating the factor provoking the problem. Treatment of bacterial and viral infectious diseases, vaginal dysbiosis is prescribed. Measures are taken to improve the functioning of the immune system.
Surgical correction involves removing foci of pathology. The specific technique is determined according to the size and location of areas of parakeratosis. The range of possible methods includes the following:
Invasive techniques are advisable in cases where the process is widespread and the presence of neoplastic changes.
To prevent parakeratosis, it is recommended to regularly visit a doctor for preventive purposes. Vaccination against human papillomavirus infection is also recommended.
More details about the pathology in the video:
Parakeratosis is a background disease that is observed after trauma to the cervix during childbirth, termination of pregnancy, installation of an IUD, infectious processes, and ectopia. There are several types of keratoses, some of them are not dangerous, others pose a serious threat to a woman’s health.
Disruption of the process of keratinization of the epithelial layer of the cervical canal is considered a precancerous condition, so the woman is examined and registered with an oncologist.