Endometritis can be asymptomatic, with the exception of the acute period, marked by fever, fever, pain in the lower body, and serous-purulent discharge.
A complication of the disease is impaired growth of the endometrium or its rejection, which often results in uterine bleeding and the inability to become pregnant and bear a baby.
In the case of pregnancy and chronic endometritis, an integrated approach is required. When planning pregnancy, therapeutic measures are provided in advance, taking into account such factors as the duration and severity of the pathology, assessment of damage to internal tissues
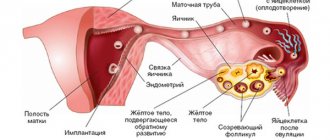
What is endometritis
Endometritis is an inflammation of the lining of the uterus (endometrium). This is a dangerous disease that can lead not only to a woman’s infertility, but also to a risk to her life and health.
Endrometritis - inflammation of the lining of the uterus (endometrium)
According to the etiological principle, endometritis can be divided into the following types:
- specific: gonorrheal;
- tuberculosis;
- actinomycotic.
In addition, endometritis can be acute or chronic (into which its acute form flows).
My friend had acute endometritis, which appeared immediately after childbirth. It was impossible not to notice it: the girl experienced severe pain in the lower abdomen, but did not observe any purulent discharge. She went to the doctor, who ordered an ultrasound and, after confirming the diagnosis, prescribed antibiotics. The treatment helped, but after getting sick, my friend was unable to get pregnant again. It is possible that other diseases present in her body are to blame.
Muzyuminka blog
Long background, I'll write briefly. I suffer from endometritis, a year and a half ago I came to the doctor with a complaint, let’s say, that I couldn’t get pregnant, to which all the doctors said that pregnancy is a complete stop, first we treat endometritis, then we think about how we can get pregnant. And she was treated and treated, and finally they found the cause, intracellular mycoplasmosis. I treated it, I think that’s it, all that remains is to treat the inflammation and you can plan normally, since because of this problem I’m suffering from bleeding. They recommended a good doctor, but I couldn’t see her for 4 months, either she was on vacation or I was out of town. But yesterday I found out that she got back from vacation and is still taking her as an uzist until next week, I think I’ll go and go and at the same time ask her to prescribe something for me to drink so that I don’t have to suffer like this, you know, the discharge is a rod and there’s no time for sex, otherwise as for planning. I arrive today at 7:30, stand in line, go up to the cashier, and in response, there are no more coupons, oh, I exploded, saying maybe it’s really not my destiny and I’ll be cured, let alone give birth, then I calmed down and went on a second visit to at least some to see a gynecologist, came, took a coupon, went to the doctor, went in, sat down calmly, she asked what was bothering me, I answered her, so and so I have endometritis and I began to tell what and how it happened and how I was treated, I wanted to tell you, but she shut me up right away and She said that she doesn’t care about my diagnoses and she is only interested in my complaints, well, I tell her that the spotting bothers me and the nagging pain sometimes, she pushed me into the chair as best she could. I thought my eyes had already popped out of my head from this feeling, I had no pain, but the very fact that they were about to squeeze something out there didn’t allow me to just relax, I looked and said endometritis was in remission, slight brown discharge, got off the chair and sat down next to her and off we go, I started asking when they were M, how they were going and when the blood smearing happened, I answered that it started on the 17th, today is the 12th day, on the 9th, 11th and 12th day there is a smear, she screamed saying, fuck me, tell me your days, I was taken aback, I say, I can’t tell you the date, but they say you’re wearing a calendar, count it. I counted and said, she still found something to bring, in general, I almost burst into tears there, the nurse sits next to me and tells me why I’m reacting so painfully, I’m still calmly trying to explain that I just wanted to tell everything so that it’s clear what and how and what I was being treated, but they shut my mouth, in general, I pulled myself together and sat and remained silent. She asks how much I’m planning with my husband, I say that it’s been in my head for years, and since the doctors are constantly either allowing or prohibiting (Here she stops me and begins to sternly say how they forbade you, what right do they have and what’s wrong with chronic end. everyone gets pregnant and gives birth calmly) I’m like this, everyone told me that it’s impossible, that it’s possible to get pregnant, but it’s not realistic, she’ll yell at me, saying that I’m born with hrs. I gave birth to endometritis 2 times, that every second person with endometritis goes to her and everything is okay and that I will never cure him and I directly quote “And you will die with him,” well, I already realized that there’s no point in arguing with her, it’s better to shut up and be silent and nod my head at the right time, in general I wanted to send everything and leave, but my interest took over, she ordered me to retake all the tests for hormones, prolactin, a blood test for compatibility with my husband (I have 1+, he has 4+, which means they are compatible), I immediately took an analysis of vaginal biocinosis, wrote out a referral to an endocrinologist (everything is fine with my thyroid gland, but my words weren’t enough for her), ASAT, Shuvarsky test, homocysteine, ultrasound, all bullshit girls, I’ll hand over everything, I need it anyway , but then the question arose, do I need to believe that in fact, with this diagnosis, I can get pregnant and give birth to a healthy baby, because as far as I read you here and looked at the graphs, it’s practically not realistic, for those who succeeded, for those I have several miscarriages behind me. who to believe, some doctors say you can’t, others you can... how so... then
Causes
The appearance of endometritis is caused by several factors at once - infection of the vagina, mechanical damage to the uterus, reduced immunity of a woman. If we consider specific reasons, they may be as follows:
- complications during natural delivery;
- dysbacteriosis (vaginosis) of the vagina;
- curettage of the cervical canal or uterine cavity;
- using the IUD as a contraceptive:
- abortion:
- endoscopic operations (surgery with small punctures) or hysteroscopy (instrumental diagnostic method of the uterus using special equipment).
Abortion is one of the causes of endometrium
Once upon a time, one of my friends had an abortion. She could not even imagine that after this she would not be able to have children. She developed chronic endometritis and other damage to the uterus, which she has been treating for many years. And it is not clear why exactly she cannot give birth to a child, but she understands that her infertility arose due to an abortion.
General description of endometritis
Of course, no disease brings anything good, and endometritis is no exception. What is endometritis? We will try to explain what this disease is. Based on the name, this is a pathological change in the endometrium - the upper layer of the inner surface of the uterus, which is involved in the inflammatory process. The causes of this disease include the following:
See also:
Chances of getting pregnant after an ovarian cystHow to get pregnant
When can you get pregnant after an abortion? How to get pregnant
Is it possible to get pregnant a week before your period? How to get pregnant
- Mechanical damage to the uterine cavity due to childbirth or surgery
- Childbirth by caesarean section
- Induced termination of pregnancy or abortion
- Consequences of a sexually transmitted disease or any other infection
- Abdominal operations
- Sex during your period
- Frequent use of hormonal female contraceptives
Symptoms
Symptoms of acute endometritis are as follows:
- lower abdominal pain;
- a sharp increase in body temperature;
- yellow purulent vaginal discharge with a putrid odor;
- intoxication (weakness, headache).
One of the symptoms of acute endometritis is pain in the lower abdomen.
Chronic endometritis occurs in a more sluggish form. Its symptoms are as follows:
- heavy and prolonged menstruation;
- irregular menstrual cycle;
- spotting between periods;
- pain in the lower abdomen not associated with menstruation:
- If a woman is pregnant, there is a possibility of miscarriage in the first trimester.
Ultrasound examination of the uterus
Signs of XE:
- expansion of the uterine cavity
- changes in the structure of the endometrium (thinning or discrepancy between the thickness and the phase of the cycle).
- presence of gas bubbles
- foci of sclerosis, calcification and fibrosis in the basal layer
- asymmetry of the walls of the uterus
Often several signs are identified. Ultrasound is performed twice: on days 5-7 and 17-21 of the cycle. However, based on ultrasound, the diagnosis of XE can only be suspected!
Hysteroscopy
Signs of XE:
- heterogeneous thickness of the endometrium
- polyps
- uneven redness
- increased bleeding of the endometrium
The procedure is carried out on days 7-10 of the cycle. It is possible to make a diagnosis only in 16-35% of cases. In approximately 30% of cases of XE, the hysteroscopic picture is ideal, therefore the method also allows only to suspect the disease.
Histological examination
Only with the help of this method can the diagnosis of XE be confirmed or refuted. It is carried out by pipel biopsy or diagnostic curettage on days 7-10 of the menstrual cycle (but in no case in the second phase!). The presence of CE is indicated by plasmacytes and lymphocytes, foci of fibrosis or sclerosis of the stroma during a long course of the disease, sclerosis of the walls of the spiral arteries feeding endometrial cells.
Immunohistoximic diagnostics
Its essence is to determine the sensitivity of endometrial receptors to estrogen and progesterone in order to select a further treatment regimen.
Infertility as a complication of the disease
The most common complication of endometritis is the spread of infection beyond the uterus. If left untreated, the following organs become infected:
- fallopian tubes;
- ovaries:
- pelvic organs.
Purulent endometritis provokes the development of peritonitis, and in some cases, sepsis.
Endometritis is a consequence of adhesions in the uterus, pelvis, and intestines that prevent the development of pregnancy, which cannot occur if the above complications develop.
Endometritis leads to the development of adhesions in the uterus
Chronic endometritis and pregnancy
Women suffering from chronic endometritis will face a number of difficulties when planning pregnancy. However, all of them are justified, because we are talking about a child, especially since a lot also depends on the mood.
Is it possible to get pregnant if you have the disease?
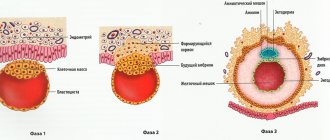
Doctors' answer to this question is clear: with untreated chronic endometritis, a woman should not decide to conceive, since the chances of conceiving and bearing a healthy baby in this case are minimal. The degenerated mucous membrane of the uterus cannot become a reliable basis for the attachment of the embryo in the event of successful fertilization.
Pregnancy and endometritis are incompatible
The course of pregnancy during the disease
Sometimes the egg is retained in the affected area of the endometrium, but a miscarriage can occur at any time. Most often this happens at the beginning of pregnancy, when the woman does not yet know about her situation. In addition, with the onset of pregnancy, the inflammatory process actively develops, affecting the walls of the uterus and spreading to the growing baby. This usually ends in miscarriage, intrauterine intoxication and death of the embryo.
Features of acute endometritis
This disease can be asymptomatic for a long time, but not its acute stage, here the symptoms appear instantly, this is often written about on Internet forums, where women describe symptoms and leave reviews about this or that type of treatment. Usually it all starts with a sharp rise in temperature; the readings can reach 40 degrees and above. In addition, there is a sharp cutting pain in the lower abdomen, weakness, and loss of appetite. Women often say that pain radiates to the back and side. One of the characteristic symptoms is considered to be gray putrid discharge, which has a rare unpleasant odor.
Moreover, the discharge may contain blood, which often complicates the diagnosis, because women may confuse it with painful menstruation.
Often the acute stage is subject to hospitalization; recovery can only be done in a hospital setting under round-the-clock medical supervision. It is especially important to consult a doctor if a woman is pregnant. After all, delay is fraught with the risk that as symptoms increase, the fetus may be rejected by the body and a miscarriage may occur.
Naturally, getting pregnant during endometritis is out of the question; few people are capable of this. After all, the endometrial mucosa is inflamed, and the fertilized egg cannot attach. But this applies only to the acute stage of the disease; the chronic form still leaves this possibility, especially after therapy.
Diagnostics
To diagnose endometritis, a full examination is carried out with determination of the size of the uterus, cervical canal and tissue surfaces, and analysis of vaginal discharge. In addition, the doctor prescribes a pelvic ultrasound, takes a smear from the vagina, draws blood and does an endometrial biopsy.
To diagnose endometritis, a pelvic ultrasound is prescribed
Treatment
Most often, endometritis can be completely cured with the help of antibiotics selected by a doctor taking into account the pathogenic microflora of the genital organs. Anti-inflammatory drugs are taken together with drugs that enhance immunity. In some cases, drugs are administered intrauterinely. In very advanced forms, endometritis is treated through surgery when medications are ineffective. If improvements are noticeable during treatment with medications, the doctor prescribes herbal and physiotherapeutic procedures. Thanks to them, endometrial cells are restored and its original properties are regenerated.
The general course of treatment lasts up to four months, and the doctor will make the first conclusions about improvement after the first 60 days.
Is it possible to get pregnant with endometritis?
When the acute form of endometritis transitions to chronic, many women complain that they cannot get pregnant.
Changes that occur with endometritis in the mucous membrane cause fertility problems.
The ability to conceive a child is assessed by such factors as the period of time during which this pathology exists, the frequency of recurrence of the pathology, and the depth of endometrial damage.
IMPORTANT!
Pregnancy with endometritis is possible subject to a course of therapy, as well as pre-conception preparation.
The course of treatment includes:
- Both local and general antibacterial therapy (elimination of the infectious factor, carried out according to the results of an analysis of the sensitivity of the flora to antibiotics);
- Immunomodulation (increasing both general and local immune status);
- Restoration of endometrial function, which is achieved through the use of hormonal agents and effects on metabolism;
- Improving ovarian function.
Diagnostic measures include:
- General clinical tests (blood and urine tests to detect inflammation);
- Smears and bacterial cultures from the vagina and cervix (excluding the presence of infection);
- Diagnostics using PCR (polymerase chain reaction) for diagnosing chronic diseases;
- Transvaginal ultrasound examination (assessment of the condition of the reproductive system organs);
- Hysteroscopy;
- Endometrial biopsy (assessment of tissue condition).
Carrying out all the activities increases the chances of getting pregnant.
Expert opinion
Shustova Olga Leonidovna
Obstetrician-gynecologist of the highest category
Chronic endometritis is the most commonly diagnosed disease in women of reproductive age, which worries both obstetricians and gynecologists and expectant mothers themselves. It has a lot of causes, different etiologies, and a variable clinical picture. Pregnancy with endometritis is possible, but it is unlikely to end happily. Therefore, if you have such a diagnosis, it is necessary to plan a future pregnancy with all the necessary diagnostic procedures and a course of therapy. Taken together, all activities will give an excellent result.
Planning pregnancy after treatment, IVF
After completely cured endometritis, a woman’s pregnancy is possible and absolutely safe. Before conceiving, a woman must make sure that her body is completely “freed” from the disease. To do this, she needs to undergo a series of tests described in the “diagnosis” section. You can plan to conceive six months after completing therapy and receiving its positive results.
After treatment of endometritis, a woman can become pregnant with IVF, but the risk of early pregnancy termination remains significant.
After treatment of endometritis, a woman can become pregnant with IVF, but the risk of early pregnancy termination remains significant
The likelihood of pregnancy with endometriosis
There is no clear answer to whether it is possible to get pregnant with endometritis. However, we can say unequivocally that this pregnancy, even if it occurs, will be problematic. If you know you have endometritis, you should not plan a pregnancy. This is a recommendation that all gynecologists are advised to adhere to. The fact is that your chances of bearing a healthy baby are negligible and you should not risk his health and life.
Problems will arise for the reason that the uterine mucosa will be degenerated and will not be able to serve as the basis for the normal attachment of the fertilized egg. That is, even if a sperm fertilizes an egg, a spontaneous miscarriage will most likely occur in the very early stages of pregnancy. Even if consolidation has occurred, the egg can detach at any time, that is, such a pregnancy will be at risk in all three trimesters.
In addition, it must be said that endometritis involves inflammation, which without appropriate treatment will only get worse, and pregnancy in this case will act as a catalyst. The worst thing is that the inflammatory process in some cases can spread to the fetus, leading to inevitable death or the development of serious malformations.
Prevention
To avoid endometritis, a woman should follow the following recommendations:
- keep genitals clean;
- practice protected sex;
- promptly treat any infection, especially related to the genital area;
- take antibiotics after cesarean section, abortion and other complex interventions;
- undergo a full examination after childbirth;
- see a gynecologist once a year;
- change intrauterine devices in a timely manner.
Chronic endometritis
As mentioned earlier, chronic endometritis may not make itself felt for a long time. But you should understand that delaying treatment does not lead to anything good; it significantly reduces your chances of getting pregnant on your own. As a result of the neglected process, the inner surface of the uterus changes, and blood circulation in the organ is disrupted. As a result, the inner shell is replaced by connective tissue, acquires a lumpy structure, and the thickness becomes heterogeneous.
The biggest problem with a chronic course is diagnosing the disease, because the symptoms remain vague. To understand the overall picture, you need to carry out a comprehensive examination, which will include:
- Analysis of complaints
- Abdominal ultrasound
- Laboratory test (PCR smear)
Only after this can the diagnosis be confirmed or refuted. In order for diagnosis to be easy, you need to visit a gynecologist at least once a year, and also listen to what you feel. You need to be especially careful when you are expecting a baby or planning a pregnancy to prevent miscarriage or missed pregnancy.