What it is?
Hysteroscopy of the uterus is a method of instrumental operational diagnostic examination. It is done in order to have a comprehensive understanding of the condition of a woman’s uterus, its internal functional layer. This is very important for assessing the likelihood of success of the procedure. With a thinned endometrium, with an uneven and thin functional layer, the likelihood of implantation of implanted embryos is, alas, low.
Hysteroscopy before IVF is done in order to know for sure whether a woman can become pregnant and carry a child. This examination is also considered mandatory after an unsuccessful IVF attempt. It will help establish the reasons why the pregnancy did not take place.
Causes and overcoming tubal infertility
Tubal infertility is one of the leading reasons why a woman cannot become pregnant. It develops as a result of previous inflammatory processes of the fallopian tubes, abdominal cavity, endometriosis, after surgical interventions for ectopic pregnancy and abortion.
Today, the most effective and, perhaps, the only method of overcoming this type of infertility is IVF. After hysteroscopy, there is a higher percentage of successful fertilization than without the use of this research method. The fact is that more than half of applicants for artificial insemination have problems with the condition of the endometrium. They do not allow the embryo to implant and therefore IVF pregnancy does not occur after transfer.
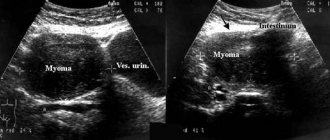
Usually, on the eve of in vitro fertilization, a woman undergoes tests such as an ultrasound. IT helps to identify uterine polyps, disruption of the endometrial structure, and myomatous nodes. But there are situations when ultrasound does not allow one to make an unambiguous conclusion about the condition of the endometrium. This happens with adenomyosis, anovulation, and polycystic ovary syndrome. In these patients, it is impossible to exclude chronic endometritis using echoscopy and establish the reason that, with impeccable conditions at all stages of the IVF protocol, positive results do not occur.
How is it carried out?
Hysteroscopy is performed using special equipment - a hysteroscope, which is a very thin and elegant probe with a built-in optical system. At the end of the probe there is a tiny video camera, which will broadcast the image to the monitor. The probe is inserted into the uterine cavity through the cervical canal.
For diagnostic purposes, hysteroscopy is performed with the thinnest probes, the diameter of which does not exceed 7 mm. This procedure is virtually painless for the patient and in most cases does not require anesthesia. The examination, although not the most pleasant, is not painful and not lengthy. The cervix is not dilated during this procedure; if a woman has increased sensitivity, she can be given pain relief.
Hysteroscope probes that are wider in diameter are used in operative hysteroscopy, when it is necessary not only to conduct a visual examination of the endometrium and uterine walls, but also to take tissue samples for analysis by biopsy.
Sometimes it becomes necessary not only to do a biopsy, but also to perform hysteroscopy with curettage, in order not only to assess the condition, but also to remove some nodes, adhesions, and neoplasms.
These types of hysteroscopy (with biopsy and separate diagnostic curettage - RDV) require dilatation of the cervix and mandatory anesthesia.
Hysteroscopy of the uterus can be diagnostic or therapeutic
Usually, it is performed under local anesthesia, since the size of the hysteroscope, which is inserted through the cervical canal into the uterine cavity, is very small and does not cause pain in the woman. The doctor inserts a hysteroscope and examines the uterine cavity from the inside. Indications for hysteroscopy are:
- clinical signs of fibroids, endometriosis, polyp, cancer;
- bleeding during menopause;
- developmental pathologies;
- infertility;
- disturbances in the cyclicity of menstruation.
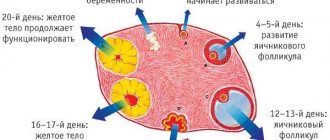
Before the examination, you need to make sure that the woman is not pregnant and does not have infectious diseases. The study is not done if there is uterine bleeding. As a rule, it is done on days 5-8 of the menstrual cycle, at which time the endometrium is just beginning to grow, and all pathologies of the basal layer are clearly visible.
During diagnostic hysteroscopy, it is possible to detect myomatous submucosal nodes, polyps, tumors, perform a biopsy and send the resulting biomaterial for research. Polyps and fibroids can be excised during hysteroscopy, while their base is cauterized with an electrocoagulator or laser.
In some cases, if hysteroscopy is done in the middle of the cycle. Small neoplasms may not be noticed, so when they are suspected, curettage is performed. Repeated hysteroscopy after curettage reveals all changes in the endometrium.
Hysteroscopy of the uterus, the consequences and complications of which can worsen a woman’s condition, at the same time makes it possible to identify pathological processes. They interfere with the onset and gestation of pregnancy, or are life-threatening.
After the procedure
After the hysteroscopy is performed, the patient is allowed to stand up and walk. For some time she has been experiencing bloody discharge from the genital tract and a slight pain syndrome. Slight hyperthermia after hysteroscopy is observed for 3-4 days. If it increases or persists longer, you should definitely consult a doctor, as this may be a sign of complications.
Complications during hysteroscopy are as follows:
- bleeding when large vessels are damaged;
- infection and endometritis;
- perforation of the uterus.
To avoid consequences, you must follow your doctor's recommendations. You cannot take a hot bath, visit the pool, monitor the temperature and the quantity and quality of discharge. Sexual activity can be carried out 2-3 weeks after the intervention.
Timing of IVF
After diagnostic hysteroscopy, if no pathologies are identified, IVF can be done within 15-30 days, that is, in the next menstrual cycle. If pathologies are identified, it takes time to carry out preliminary treatment if doctors consider it appropriate.
After hysteroscopy with biopsy, IVF can be prescribed after about 2-3 months, and after the procedure with curettage, IVF is planned no earlier than six months later. In each specific case, the doctor prescribes the timing of the in vitro fertilization protocol after hysteroscopy, taking into account individual risks and examination results.
Indications
Hysteroscopy is a great help for fertility doctors. We can safely say that it increases the chances of successful IVF, since it allows the doctor to know all the “weak” points of the female body. An examination is not always prescribed, but only for certain indications, including:
- infertility caused by recurrent miscarriage (a history of several miscarriages or missed pregnancies);
- infertility caused by endometriosis;
- infertility due to a history of several abortions;
- if the doctor suspects polyps, adhesions, damage to the mucous membranes after operations;
- infertility due to uterine fibroids;
- idiopathic infertility, the cause of which has not been established;
- infertility associated with irregularities in the regular menstrual cycle.
Hysteroscopy is mandatory after several unsuccessful IVF attempts. The effectiveness of hysteroscopy is considered very high; the examination is classified as highly accurate.
Advantages and disadvantages of hysteroscopy
A hysteroscopic examination helps to clarify and confirm the suspected diagnosis of uterine cavity pathology, as well as, in some cases, eliminate the cause of infertility, which will prevent IVF failure.
The advantages of the method include:
- the possibility of visual assessment of the uterine cavity;
- minimally invasive;
- no need for hospitalization;
- if necessary, microsurgical treatment.
The results of the examination make it possible to analyze factors that impede pregnancy, determine tactics for further combating infertility, and the time of referral for IVF. But perfection does not exist in nature.
Experts point out certain disadvantages of the method:
- reflects only changes in the inner layer of the uterus;
- contraindicated in certain conditions;
- may be accompanied by adverse effects and complications.
Before the procedure, it is important to discuss with the attending physician the characteristics of the woman’s condition, the presence of concomitant diseases, and clarify possible contraindications to hysteroscopy.
Goals before IVF
A hysteroscopic examination before IVF is prescribed for both diagnostic and therapeutic purposes; it helps determine the preparation of the patient’s body for in vitro fertilization.
Hysteroscopy allows:
- diagnose individual diseases;
- remove a small tumor of the uterine cavity;
- take material for histological examination;
- carry out diagnostic curettage;
- decide on a method of treating infertility.
Diagnostic hysteroscopy will make it possible to prepare the endometrium for IVF, and possibly avoid surgical intervention. If pathological conditions are detected, it is likely that the doctor will prescribe a control hysteroscopy after completion of the course of treatment in order to assess the effectiveness of therapy and prepare for IVF.
Statistics say: the IVF procedure is only 35-40% effective on the first try. The absence of pathological conditions in the uterine cavity increases the chances of success.
Hysteroscopy allows not only to diagnose endometrial diseases, but also to simultaneously carry out surgical treatment: dissection of adhesions, removal of polyps and submucous fibroids.
Contraindications
They try not to perform hysteroscopy if a woman has malignant tumors in the uterine area or severe stenosis of the cervical canal.
The diagnostic procedure is not carried out for women who were ill at the time of the examination with the flu, acute respiratory viral infection or any other disease - time is required to recover, after which the temporary ban will be lifted and the woman will be able to undergo the examination.
Some vascular and heart diseases, as well as uterine bleeding at the time of hysteroscopy, are considered a contraindication to the procedure. A relative contraindication is the absence of a history of pregnancy or childbirth.
Some doctors try not to refer women who are about to have their first pregnancy for hysteroscopy.
Preparing for the procedure before IVF
Before hysteroscopy, a woman must undergo all tests prescribed by the doctor. Typically, general blood and urine tests, a biochemical blood test, and a vaginal smear for microflora and infections are prescribed. If the laboratory diagnostic results are positive, the woman is sent for an ultrasound of the pelvic organs. And only then can she undergo hysteroscopy of the uterus.
Before IVF, hysteroscopy is prescribed between the 6th and 10th day of the menstrual cycle, the report is kept from the first day of the last menstruation. There is no need to go to the hospital for examination. If hysteroscopy is performed only as a diagnosis and is not accompanied by a biopsy or curettage, then the woman will stay in the clinic for no more than three hours. The procedure itself takes about 10-15 minutes.
After curettage, the hospital stay can last up to a day or a little more if any complications develop. The procedure in this case can last up to an hour. By the way, the likelihood of complications after the procedure is not so high - no more than 1%.
When can you do IVF after hysteroscopy – Gynecology
When preparing for IVF, a woman undergoes many examinations and takes a large number of tests.
This is not a whim of medical institutions, but a real necessity: the doctor must be well aware of the difficulties he may encounter when artificially inseminating a particular patient.
Hysteroscopy is considered one of the most important and informative tests. What this examination is, how it is carried out and what it shows, we will tell you in this material.
Hysteroscopy of the uterus is a method of instrumental operational diagnostic examination.
It is done in order to have a comprehensive understanding of the condition of a woman’s uterus, its internal functional layer. This is very important for assessing the likelihood of success of the procedure.
With a thinned endometrium, with an uneven and thin functional layer, the likelihood of implantation of implanted embryos is, alas, low.
Hysteroscopy before IVF is done in order to know for sure whether a woman can become pregnant and carry a child. This examination is also considered mandatory after an unsuccessful IVF attempt. It will help establish the reasons why the pregnancy did not take place.
Hysteroscopy is performed using special equipment - a hysteroscope, which is a very thin and elegant probe with a built-in optical system. At the end of the probe there is a tiny video camera, which will broadcast the image to the monitor. The probe is inserted into the uterine cavity through the cervical canal.
For diagnostic purposes, hysteroscopy is performed with the thinnest probes, the diameter of which does not exceed 7 mm.
This procedure is virtually painless for the patient and in most cases does not require anesthesia. The examination, although not the most pleasant, is not painful and not lengthy.
The cervix is not dilated during this procedure; if a woman has increased sensitivity, she can be given pain relief.
Hysteroscope probes that are wider in diameter are used in operative hysteroscopy, when it is necessary not only to conduct a visual examination of the endometrium and uterine walls, but also to take tissue samples for analysis by biopsy.
Sometimes it becomes necessary not only to do a biopsy, but also to perform hysteroscopy with curettage, in order not only to assess the condition, but also to remove some nodes, adhesions, and neoplasms.
These types of hysteroscopy (with biopsy and separate diagnostic curettage - RDV) require dilatation of the cervix and mandatory anesthesia.
After diagnostic hysteroscopy, if no pathologies are identified, IVF can be done within 15-30 days, that is, in the next menstrual cycle. If pathologies are identified, it takes time to carry out preliminary treatment if doctors consider it appropriate.
After hysteroscopy with biopsy, IVF can be prescribed after about 2-3 months, and after the procedure with curettage, IVF is planned no earlier than six months later. In each specific case, the doctor prescribes the timing of the in vitro fertilization protocol after hysteroscopy, taking into account individual risks and examination results.
Hysteroscopy is a great help for fertility doctors. We can safely say that it increases the chances of successful IVF, since it allows the doctor to know all the “weak” points of the female body. An examination is not always prescribed, but only for certain indications, including:
- infertility caused by recurrent miscarriage (a history of several miscarriages or missed pregnancies);
- infertility caused by endometriosis;
- infertility due to a history of several abortions;
- if the doctor suspects polyps, adhesions, damage to the mucous membranes after operations;
- infertility due to uterine fibroids;
- idiopathic infertility, the cause of which has not been established;
- infertility associated with irregularities in the regular menstrual cycle.
Causes of female infertility
Hysteroscopy is mandatory after several unsuccessful IVF attempts. The effectiveness of hysteroscopy is considered very high; the examination is classified as highly accurate.
They try not to perform hysteroscopy if a woman has malignant tumors in the uterine area or severe stenosis of the cervical canal.
The diagnostic procedure is not carried out for women who were ill at the time of the examination with the flu, acute respiratory viral infection or any other disease - time is required to recover, after which the temporary ban will be lifted and the woman will be able to undergo the examination.
Some vascular and heart diseases, as well as uterine bleeding at the time of hysteroscopy, are considered a contraindication to the procedure. A relative contraindication is the absence of a history of pregnancy or childbirth.
Some doctors try not to refer women who are about to have their first pregnancy for hysteroscopy.
Before hysteroscopy, a woman must undergo all tests prescribed by the doctor. Typically, general blood and urine tests, a biochemical blood test, and a vaginal smear for microflora and infections are prescribed. If the laboratory diagnostic results are positive, the woman is sent for an ultrasound of the pelvic organs. And only then can she undergo hysteroscopy of the uterus.
Before IVF, hysteroscopy is prescribed between the 6th and 10th day of the menstrual cycle, the report is kept from the first day of the last menstruation.
There is no need to go to the hospital for examination.
If hysteroscopy is performed only as a diagnosis and is not accompanied by a biopsy or curettage, then the woman will stay in the clinic for no more than three hours. The procedure itself takes about 10-15 minutes.
After curettage, the hospital stay can last up to a day or a little more if any complications develop. The procedure in this case can last up to an hour. By the way, the likelihood of complications after the procedure is not so high - no more than 1%.
Before hysteroscopy, a woman is advised to refrain from eating for 12 hours. On the day of the procedure, you should do an enema, empty your bowels, and empty your bladder half an hour before the procedure. Taking aspirin and any drugs based on acetylsalicylic acid is prohibited at least a week before hysteroscopy to avoid bleeding.
If a woman has taken anticonvulsants or painkillers, this should be reported to the doctor before hysteroscopy. Sex is not recommended 3-5 days before the procedure.
As already mentioned, not all women undergoing IVF are recommended by their doctor to undergo hysteroscopy. The modern approach of the World Health Organization to this issue is somewhat different - this organization strongly recommends hysteroscopy for everyone who goes for IVF.
Firstly, this will improve the protocol, since the fertility specialist will have more initial information. Secondly, it will save patients time and money.
After an unsuccessful attempt, a hysteroscopy will still have to be done, and it is better to do it before the first attempt to increase the chances of pregnancy.
If your doctor has not prescribed hysteroscopy, you can contact him with this question and ask him to add the examination to the appointment before IVF. This is a woman's right.
You can have a hysteroscopy performed as prescribed by a doctor completely free of charge. It is carried out in most public hospitals and clinics, as well as at antenatal clinics. However, be prepared for the queue for the procedure to be impressive.
If you need to get the examination done faster, you should contact a private clinic that provides similar services.
The cost can vary - from the basic 4-7 thousand for a diagnostic procedure to 30 thousand rubles for hysteroscopy with RDV and subsequent histological analysis of tissue from the uterine cavity.
The best option for a woman planning IVF is to have a hysteroscopy with the doctor who will plan the IVF protocol.
The most positive reviews from women are about office hysteroscopy, which for diagnostic purposes can be performed directly in the office of an obstetrician-gynecologist at the gynecological cross. It's fast, not painful and quite informative.
According to women who have undergone this procedure, hysteroscopy with curettage significantly increases the chances of pregnancy. Most women, after an unsuccessful attempt and subsequent procedure, manage to become pregnant in the second or third protocol.
To learn about the features of hysteroscopy before IVF, see the following video.
Source:
Eco after hysteroscopy: when can it be done?
Today, infertility is becoming an increasingly pressing problem among women. According to statistics, female infertility occurs on average in 19% of cases, more than half of this number is accompanied by endometrial diseases. One of the options for solving the problem of infertility is IVF (in vitro fertilization).
But the presence of an intrauterine pathology in a woman significantly reduces the effectiveness of this procedure. When choosing a method for detecting intrauterine diseases, specialists choose hysteroscopy, an invasive examination of the uterine cavity. This method serves as the “gold standard” in diagnosing endometrial pathology.
When you can do IVF after hysteroscopy can only be judged after receiving the results of this study.
According to indications before IVF, a woman may be prescribed hysteroscopy
If the examination is not scheduled
As already mentioned, not all women undergoing IVF are recommended by their doctor to undergo hysteroscopy. The modern approach of the World Health Organization to this issue is somewhat different - this organization strongly recommends hysteroscopy for everyone who goes for IVF. Firstly, this will improve the protocol, since the fertility specialist will have more initial information. Secondly, it will save patients time and money. After an unsuccessful attempt, a hysteroscopy will still have to be done, and it is better to do it before the first attempt to increase the chances of pregnancy.
If your doctor has not prescribed hysteroscopy, you can contact him with this question and ask him to add the examination to the appointment before IVF. This is a woman's right.
Price
You can have a hysteroscopy performed as prescribed by a doctor completely free of charge. It is carried out in most public hospitals and clinics, as well as at antenatal clinics. However, be prepared for the queue for the procedure to be impressive.
If you need to get the examination done faster, you should contact a private clinic that provides similar services. The cost can vary - from the basic 4-7 thousand for a diagnostic procedure to 30 thousand rubles for hysteroscopy with RDV and subsequent histological analysis of tissue from the uterine cavity. The best option for a woman planning IVF is to have a hysteroscopy with the doctor who will plan the IVF protocol.
Reviews
The most positive reviews from women are about office hysteroscopy, which for diagnostic purposes can be performed directly in the office of an obstetrician-gynecologist at the gynecological cross. It's fast, not painful and quite informative.
According to women who have undergone this procedure, hysteroscopy with curettage significantly increases the chances of pregnancy. Most women, after an unsuccessful attempt and subsequent procedure, manage to become pregnant in the second or third protocol.
To learn about the features of hysteroscopy before IVF, see the following video.
medical reviewer, psychosomatics specialist, mother of 4 children
Hysteroscopy is one of the diagnostic methods in gynecology, which allows you to visually assess the condition of the patient’s uterine cavity. It is performed under local anesthesia or general (intravenous) anesthesia using a special optical device - a hysteroscope.
Hysteroscopy and IVF
Many women are interested in whether to do hysteroscopy before IVF. In many cases, this examination is mandatory.
- infertility of unknown etiology;
- signs of uterine development abnormalities;
- recurring uterine bleeding;
- habitual miscarriage;
- history of several unsuccessful IVF attempts.
Hysteroscopy before IVF is mandatory if uterine factor infertility is suspected. In this case, the diagnostic procedure can immediately become a therapeutic one. The technique makes it possible to remove some formations in the uterine cavity.
After hysteroscopy, the doctor immediately prescribes treatment for a disease that reduces fertility. If it is a myomatous node or polyp, it is removed. If the disease requires conservative therapy, the necessary medications are prescribed.
After completing the course of treatment, a repeat hysteroscopy is performed before IVF. It is needed to evaluate the result of the treatment. If it is satisfactory, then the patient can enter into the protocol.
Features of the procedure
When searching for the cause of infertility, in many cases the doctor prescribes diagnostic hysteroscopy. However, some women are afraid to undergo the procedure and doubt whether hysteroscopy is necessary before IVF. This procedure is really necessary, as it allows us to identify diseases that reduce the chance of success during in vitro fertilization.
- Polyps.
- Myomatous nodes in the uterine cavity.
- Endometrial hyperplasia.
- Endometriosis.
- Anomalies of organ development.
- Strictures, adhesions, synechiae in the uterus.
Hysteroscopy of the uterus before IVF allows you to identify these diseases in time and, if necessary, immediately carry out surgical treatment.
The procedure is carried out using a special optical instrument - a hysteroscope. It involves the use of anesthesia to eliminate pain. Office endometrial hysteroscopy can be used to diagnose uterine pathology. Before IVF, it is performed on an outpatient basis and does not require pain relief or hospitalization.
Its main features are:
- No need for general anesthesia.
- No risk of cervical trauma
- High safety profile.
Hysteroscopy after unsuccessful IVF is prescribed quite often. It happens that a woman manages to obtain high-quality eggs, they are successfully fertilized, but after the transfer the embryo does not implant into the uterine mucosa. In such cases, hysteroscopy often helps to determine the cause of failure.
Carrying out the procedure
In ART clinics, if endometrial pathology is suspected, many patients undergo hysteroscopy before IVF. On what day of the cycle is the diagnosis performed? Most often this is days 6-9 of the cycle. During this period, the endometrium is still thin and most pathologies can be identified.
Hysteroscopy and IVF
Hysteroscopy and IVF after this manipulation are discussed on infertility forums. Women are interested in how it can help, and when can IVF be done after hysteroscopy?
A detailed study of the uterine cavity will help identify small adhesions and polyps that are not visible on ultrasound, but can cause IVF failure. There are many reviews on the Internet where, after unsuccessful attempts, they did a hysteroscopy and found minor changes. And after they were eliminated, women became pregnant after the first protocol. Therefore, this procedure before IVF significantly increases the chances of getting pregnant.
Moreover, if a woman has already had a hysteroscopy, this does not mean that repeated manipulation is pointless. If two years ago, during the study, synechiae were dissected or a polyp was removed, this does not mean that they could not arise again. Therefore, with two or three unsuccessful IVF, reproductive specialists advise repeating the procedure.
When to do IVF after hysteroscopy, the doctor decides. It depends on the result obtained from the study. If during the study no pathologies were found, or only an endometrial biopsy was done, then the protocol can be entered into in the next cycle, although reproductive specialists advise waiting for the endometrium to fully recover, because stress after the intervention affects hormonal levels, which can adversely affect affect during in vitro fertilization.
Pregnancy after a diagnostic procedure
Often, hysteroscopy before IVF or in the process of searching for the causes of infertility is performed not for therapeutic purposes, but for diagnostic purposes. As a result of examining the uterus, it often turns out that no medical procedures are required. After all, it is not at all necessary that the doctor will find polyps, synechiae or fibroids inside the uterus.
Modern hysteroscopes are very small in size. A tube of minimal diameter is inserted into the uterus without dilating the cervical canal. The procedure for examining the uterine cavity is completely non-traumatic. It does not require restoration. Therefore, IVF after hysteroscopy can be done immediately. There is no need for a rehabilitation period.
If hysteroscopy before IVF reveals any problems that limit the possibility of artificial insemination, treatment may be required. Sometimes it is conservative, in other cases it is surgical. In such a situation, the duration of rehabilitation depends on the severity of the disease and the chosen treatment method. It happens that a doctor prohibits a woman from becoming pregnant for several months after hysteroscopy due to the increased risk of spontaneous abortion.
Does hysteroscopy reduce the effectiveness of IVF?
Hysteroscopy does not reduce, but increases the effectiveness of IVF. Actually, this is why the procedure is carried out. It is performed precisely in order to remove obstacles to achieving pregnancy.
During the manipulation, the doctor can excise polyps, destroy synechiae, or perform other actions that will lead to the formation of an anatomically correct uterine cavity and improve the condition of the endometrium. The operation can be traumatic. In this case, pregnancy is impossible until the endometrium is fully restored. This is unlikely to take more than 2-3 months. IVF is then carried out, which has a much higher chance of success.
It is intrauterine pathological processes that often become the reason that pregnancy does not occur even when high-quality embryos are transferred. After all, IVF affects many stages of reproductive function (ovum maturation, fertilization, embryo growth up to 3-5 days), but doctors still have little control over implantation processes. Therefore, without timely treatment of uterine diseases, including the hysteroscopic method, pregnancy is often impossible, or the likelihood of its occurrence is much lower.
Thus, hysteroscopy is an effective method of treating infertility. This operation usually does not have any negative health consequences. In capable hands, hysteroscopy helps a woman achieve the desired pregnancy.
What is hysteroscopy
If we explain the essence of diagnostic hysteroscopy in simple language, then it comes down to examining the uterus (its cervix, cavity and tubal orifices) using optical (fiber optic) devices (hysteroscope, hysterofibroscope and hysteroresectoscope).
In modern gynecology, hysteroscopy before IVF has become the most popular endoscopic examination. This method is considered completely safe, does not threaten women's health and does not interfere with getting pregnant. This method is unique in that it can provide a solution to several issues at once regarding the prevention and detection of problems in a woman’s gynecological health. This optical method can be used for the following purposes:
- surgical;
- diagnostic;
- control.
The diagnostic test consists of a qualitative examination of the uterus.
During surgical exploration, the integrity of the uterine mucosa is disrupted.
The control method is carried out to assess the quality of the treatment provided.
Thanks to hysteroscopy, the causes of many gynecological pathologies are identified (inflammatory diseases, endometrial polyps, infertility, bleeding) and the identified pathologies are immediately treated (polyps, adhesions, etc. are removed)
Why is hysteroscopy needed before IVF?
Hysteroscopy prescribed before IVF allows a woman to replace several unpleasant procedures at once (for example, curettage in a hospital setting). Ultrasound, for example, is not able to detect minor intrauterine pathologies. The hysteroscopy method and its optical capabilities make it possible to:
- assessment of patency of the cervical canal;
- diagnostics of endometrial health;
- cauterization of erosions;
- cervical biopsy;
- dissection of adhesions or intrauterine septa;
- removal of polyps.
This method also allows the doctor to choose the correct IVF protocol scheme and treatment method.
Hysteroscopy before IVF is not mandatory but extremely useful and desirable. Most often, this method is used for diagnostic purposes (office hysteroscopy), but sometimes it is combined with minor surgical procedures (curettage).
Most women believe that successfully performed IVF already guarantees the result of bearing and delivering a healthy child on time. However, many gynecological pathologies of the mother can interfere with the successful continuation of pregnancy and reduce this expensive procedure to nothing.
Therefore, it is completely justified to perform a hysteroscopy before a number of negative embryo transfer results are obtained. This will maximize the chances of a successful pregnancy and birth of a child.
After hysteroscopy, when can I do IVF?
katyunchik
How long after hysteroscopy can IVF be done?
Girls, hello everyone. Please tell me how long after hysteroscopy you can do IVF? Thanks to all. Continue reading →
Alina
Hysteroscopy
Girls, did everyone have hysteroscopy before IVF? There was one attempt at IVF, unfortunately not successful, we have a very strong male factor, but the doctor insists on a hysteria.. I have no indications for it, but the doctor argues his insistence by saying that IVF works for all healthy people the FIRST time.. Read further →
Julia
Hyperplasia, or rather foci of glandular hyperplasia of the endometrium
The girls had a diagnostic hysteroscopy and did not scrape. An analysis came back that foci of glandular endometrial hyperplasia were found. Who had it? Do I need to do this again for mystera, but with cleaning and then treatment? Or maybe just treatment? Please tell me! I'm worried! New mother in IVF! I'm already thinking about IVF. But now this hyperplasia is an obstacle
Source: https://www.BabyBlog.ru/theme/posle-gisteroskopii-kogda-mozhno-delat-eko
What can be determined during hysteroscopy
By prescribing a hysteroscopy method before IVF, the doctor thereby aims to prepare the endometrium for the most successful in vitro fertilization. This method is called minimally invasive, that is, it is as harmless as possible to the woman’s health. In addition, how to carefully assess the condition and quality of the uterine mucosa; with this endoscopic method, it is possible to simultaneously perform minor surgical interventions to remove obstacles to the implantation of the embryo in the uterine cavity (benign neoplasms, nodes, adhesions, etc.)
Thanks to this minimally invasive method, it is possible to identify the following types of pathologies:
- hyperplasia, polyps or atrophic changes in the endometrium;
- congenital pathology of the uterus;
- adenomyosis;
- foreign objects;
- intrauterine synechiae;
- submucosal nodes.
Very often, women suffering from infertility experience several pathologies of the gynecological organs, which can actually be identified during examination.
Complications
The risk of possible complications of hysteroscopy is minimal. Conventionally, doctors divide the adverse effects of this manipulation into mechanical and inflammatory. Possible damage to the uterine wall with a hysteroscope, prolonged uterine bleeding, impaired discharge of secretions, accumulation of blood inside the uterus (hematometra), and the development of inflammatory processes in the female genital organs.
If your body temperature rises, intense pain in the lower abdomen, or increased bleeding, consult a specialist immediately.
Hysteroscopy is not only justified before IVF, but also can significantly improve the quality of artificial insemination. Compliance with the necessary conditions of manipulation will help couples suffering from infertility experience the joy of having a new family member.
Preparing for the study
There are a number of rules for preparing for this study. It includes both a special examination and drug treatment. Before hysteroscopy, a thorough examination of the woman is necessary, which includes:
- gynecological examination on a chair;
- fluorography;
- examination of discharge (from the vagina, cervical canal) for microflora and degree of purity;
- analysis to determine helminthic infestations;
- Ultrasound of the pelvic organs;
- complete blood count, determination of blood group and Rh status;
- blood tests for dangerous infections (syphilis, AIDS);
- other types of studies as indicated (blood biochemistry, urine analysis, cardiac ECG, consultation examination by doctors of other specialties, etc.)
Preparation and execution
Any intrauterine procedure can contribute to changes in the normal microflora due to disruption of the cervical barrier, damage to the endometrium, and the woman’s stressful state during the procedure. All this can contribute to the development of complications.
Hysteroscopy does not require special preparation. To reduce possible adverse outcomes to a minimum, it is recommended to:
- general clinical laboratory tests of blood and urine;
- determination of blood group, Rh status;
- study of the state of the coagulation system;
- undergoing electrocardiography and fluorographic examination;
- taking a vaginal smear to detect pathogenic microorganisms.
The possibility of prophylactic antibiotic therapy should be discussed with your doctor. Evidence-based medicine does not support that a single dose of antibiotics the day before the procedure will help prevent infection.
The procedure is carried out on an empty stomach. It is necessary to avoid a large dinner and not to have breakfast on the day of the examination, and also reduce fluid intake to a minimum. During the day before the manipulation, it is undesirable to be sexually active.
It is best to leave contact lenses and jewelry at home in advance, and there is no need to apply makeup or smoke before the procedure. If a woman is afraid of the upcoming examination, it makes sense to ask the doctor about a possible one-time dose of a mild sedative.
The manipulation is carried out by a trained specialist in a specialized medical institution.
Before hysteroscopy, a woman signs an “Informed Voluntary Consent” for it to be performed. The patient has the right not only to familiarize herself with the text of the document, but can also ask the doctor any questions that concern her.
The diagnostic endoscopic procedure requires general anesthesia. The woman is put under short-term general anesthesia.
The time for diagnostic hysteroscopy usually does not exceed half an hour. After local and general anesthesia, the specialist inserts cervical dilators and then a hysteroscope into the uterine cavity and examines the internal walls. To smooth out folds and improve the quality of diagnosis, the uterus is filled with sterile saline solution. Before removing the hysteroscope, fluid is removed from the canal.
After the procedure, some women report minor spasmodic pain in the suprapubic area, spotting and spotting for several days after the intervention. Therefore, doctors prohibit sexual intercourse during this period. After removing the hysteroscope, the patient is recommended to stay in a medical facility for several hours under the supervision of a specialist.
Implementation time before IVF
Hysteroscopy is informative on days 6-9 of the monthly cycle, when the state of the endometrium makes it possible to identify the largest number of diseases that impede successful IVF. The question of the possibility of IVF after the hysteroscopy procedure is decided strictly individually for each woman.
In the case of endoscopic surgical treatment, IVF will be effective only after several months. It takes time for the endometrium to recover.
If no pathological processes are identified during a hysteroscopic examination, the patient begins preparations for IVF. If the uterine mucosa is in normal condition, artificial insemination is carried out after subsequent menstruation.
On what day is hysteroscopy done before IVF?
Most often, the hysteroscopy procedure is performed on days 5-7 of the cycle (proliferative phase). It is at this time that the uterine mucosa is least susceptible to bleeding.
The procedure is not recommended at other times for the following reasons:
- risk of bleeding;
- possibility of complications;
- low information content of the procedure (due to thickening of the endometrium).
Occasionally, the procedure is recommended for 3-5 days before the start of menstruation (in the secretory phase).
Indications for hysteroscopy before IVF
Like any endoscopic examination, hysteroscopy has its indications and contraindications.
This method may be indicated for:
- Disorders of the cervical canal (areas of narrowing, foreign bodies, polyps).
- Intrauterine disorders (polyps, nodes, synechiae, hyperplastic or dystrophic processes, chronic endometriosis).
- Several unsuccessful attempts at IVF.
Contraindications
No matter how good and effective hysteroscopy is, in some cases it is absolutely forbidden.
Contraindications for this method are:
- The patient’s serious condition for any ailment (until the condition is fully compensated).
- Any infectious diseases (due to the risk of infection spreading in the body).
- Cancers of the cervix (due to the risk of spreading to surrounding tissues). This can be facilitated by liquid media used during manipulation.
- Uterine bleeding. However, this procedure will have low effectiveness due to the presence of blood clots in the uterus.
- Pathologies of blood clotting (due to the risk of severe bleeding after any surgical interventions).
- Menstruation. Due to the low effectiveness of the study (poor review), it is carried out no earlier than 5-7 days of the cycle.
- Inflammatory processes in the genital organs. This method is not used for exacerbation of chronic ailments. It is first important to treat inflammation and reduce the activity of ongoing pathological processes.
- Narrowing (stenosis) of the cervix. This can seriously damage the integrity of the canal when the endoscope is inserted.
In all such cases, hysteroscopy is performed only for health reasons.
Recovery period
Primary restoration of the mucosa is completed within two to three weeks after the manipulation. Healing of microscopic damage to the endometrium and cervical canal occurs. During this period, areas of epithelium, blood clots and mucus are released.
It is not recommended for a woman to:
- performing douching;
- insertion of tampons, suppositories and other devices into the vagina;
- visiting a bathhouse or sauna.
Complete rehabilitation involves the formation of a new endometrium and the final restoration of the functions of the uterine mucosa. Doctors say that restoration of the endometrium after hysteroscopy is possible in a few months, so it is sometimes recommended to postpone IVF for this period.
How is hysteroscopy performed?
Most often, diagnostic hysteroscopy is used before IVF. The procedure is performed in a gynecological clinic or center. The procedure can also be performed on an outpatient basis.
No incision is made during this study. Optical equipment is inserted into the body through the vagina.
The sequence of such a study is as follows:
- The patient is in a gynecological chair.
- Previously, this operation was performed without anesthesia. However, due to the pain, the manipulation is now performed under general short-term anesthesia (usually intravenous drip). If intravenous anesthesia is contraindicated, mask anesthesia is used.
- In rare cases, other types of anesthesia are used (epidural, spinal, endotrachial anesthesia).
- During the study, the main vital functions of the body (cardiac activity, breathing) are monitored.
- Treatment of the external parts of the genital organs and the surface of the thighs (inner) with an alcohol solution.
- Exposure of the cervix using a vaginal speculum.
- Insertion of a probe into the uterine cavity with Hegar dilators.
- Introduction into the cavity of a special composition that allows you to examine uterine abnormalities.
After opening the cervical canal, insertion of the hysteroscope.
- On the monitor, the surface of the uterus is enlarged and perfectly visible.
- If necessary, microoperations are performed in the cavity (curettage of the uterine mucosa, removal of polyps, etc.)
- The image being manipulated is written to disk.
- At the end of the operation, the hysteroscope is removed and the uterine cervix closes spontaneously.
- After recovery from anesthesia, the woman is observed by an anesthesiologist for at least 2 hours.
- Usually the patient is inpatient (from several hours to 4 days).
In vitro fertilization is an effective reproductive technology
In vitro fertilization, or IVF, is one of the most effective infertility treatments. It is used when a woman has diseases that are an obstacle to spontaneous pregnancy. Hysteroscopy plays an important role in the diagnosis of pathologies.
With IVF, fertilization of the egg occurs outside the woman's body. It is preceded by stimulation of ovulation, retrieval of eggs and their washing. Then the man's ejaculate is obtained, from which sperm are isolated. They are placed on a nutrient medium where the egg is already located.
Male reproductive cells independently move towards the oocyte, one of the sperm fertilizes it. After fertilization, the egg is placed in a thermostat, where the embryo develops. On the third or fifth day it is transferred to the uterine cavity. Pregnancy occurs after implantation of the embryo.
Unfortunately, not in all cases of IVF it is possible to achieve the desired result the first time. So, after the first IVF attempt, pregnancy occurs in approximately thirty percent of cases. This happens for various reasons. One of them is concomitant pathology of the endometrium, which was not identified at the stage of preparation for IVF. This situation can be corrected if hysteroscopy is included in the complex of diagnostic examinations.
How should a woman behave after the procedure?
After the procedure, a woman is usually recommended the following course of action:
- take antibiotics according to the regimen prescribed by your doctor;
- hygienic washing of the genitals (twice a day);
- daily temperature measurement twice;
- for painful manifestations, use painkillers recommended by the doctor;
- exclusion of bathing in the bathtub or ponds (only a shower is acceptable);
- exclusion of any stress (physical, psychological), sexual activity, thermal procedures (for at least 2 weeks);
- monitor the type and amount of discharge from their genitals.