≡ Home → Modern approaches to the treatment of fibroids →
In modern gynecology, the concept of uterine fibroids has changed significantly. Previously, it was believed that the tumor grows solely against the background of high estrogen levels. Therefore, doctors prescribed hormonal drugs based on progesterone - and assumed that such a regimen would give a positive result.
Paradoxically, against the background of the use of progesterone drugs, fibroids sometimes began to grow. Scientists studied this phenomenon and found out that not only estrogen, but also progesterone is to blame for the development of the tumor. It also leads to the growth of the node - and this largely explains the fact why the formation grows in the first half of pregnancy.
Today, progesterone-based drugs are becoming a thing of the past. They are prescribed less and less for uterine fibroids - and they have been replaced by other effective remedies. We will tell you more about how progesterone acts on the development of the node and why we abandoned gestagens below in the article.
Reproductive system in women
External and internal genitalia in women are necessary for procreation and hormonal regulation of the body.
The female reproductive system is formed by the mammary glands and pelvic organs. In the ovaries, the formation of germ cells and the release of hormones necessary for the development of the female body occur. The mature egg is transported to the fallopian tube, where fertilization occurs after sperm penetrate the reproductive system. Then the germ of a new organism penetrates the uterine cavity, penetrates into the inner lining of the organ and receives everything necessary for further formation. Accessory structures, such as the gonads, are responsible for maintaining reproductive function. The uterus is a hollow organ designed for the development of the fetus. This anatomical structure is located next to the bladder and rectum. With the help of the cervix and vagina, the organ communicates with the external environment for the penetration of male cells during sexual intercourse. The uterus is also connected to the fallopian tubes, which ensures the introduction of the embryo of a new organism. The main stage of organ development occurs during a woman’s puberty, when hormones stimulate the final formation of the reproductive system. At this time, girls begin menstrual cycles, characterized by renewal of the inner layer of the uterus and the release of a mature germ cell into the fallopian tube.
Structure of the uterus:
- The mucous membrane (endometrium) is the internal lining of the organ, mainly consisting of tubular glands. The endometrium is necessary for the implantation of the embryo and the subsequent maintenance of embryonic development. If, after the release of a mature egg into the fallopian tube, fertilization does not occur, the endometrium is destroyed and renewed. Destruction of the endometrium during menstruation is manifested by uterine bleeding.
- The muscular (median) membrane, consisting of three layers of smooth muscle. Contractions of the uterine muscles are necessary to remove the destroyed endometrium and childbirth. In addition, the muscular structure of the uterus helps the organ stretch as the new organism grows.
- The outer shell of an organ, consisting of connective tissue. This section of the uterus is connected to the abdominal covering.
The uterus is a constantly renewing organ. Before the onset of menopause (up to about 50 years), characterized by changes in hormonal regulation of the body, women menstruate monthly. This physiological process indicates the ability of the female body to procreate. Unfortunately, hormonal changes during the menstrual cycle often lead to the development of pathologies of the reproductive system.
Hormonal drugs
Hormones are active elements involved in all physiological processes. They are produced by the endocrine glands and coordinate various processes in the body: growth, reproduction, etc.
Hormone therapy is the use of hormones and their artificial analogues for therapeutic purposes.
The production of hormones in the body occurs according to the principle of deficiency. When their level in the blood is below normal, the corresponding glands begin to produce them more actively, replenishing the deficiency. If there is not enough of a hormone, this indicates a malfunction of the iron that produces it, but if there is a lot of hormone, it means that the organ is not working within normal limits.
In modern medicine, three types of hormone therapy are used:
- Stimulating therapy is used when it is necessary to activate the function of the endocrine gland and determine its capabilities. Preparations containing neurohormones of the hypothalamus and anterior pituitary gland are used.
- Inhibitory or blocking therapy is used when there is excessive activity on the part of any endocrine gland, also for the treatment of certain types of neoplasms. This therapy is used in combination with radiation or surgery.
- Replacement therapy is used for problems of the endocrine system that occur with partial or complete inhibition of the function of the endocrine gland. Preparations containing the hormone itself or its synthetic analogue are used. The regimen for taking hormonal drugs must correspond to the physiological processes in the body.
Reasons for development
The exact cause of uterine fibroids is unknown. Doctors suggest that the key factor in the development of the disease is hormonal imbalance, but in many women, a benign tumor of the uterus occurs without disrupting the endocrine regulation of the organ. It is important to consider that sex hormones are responsible for the thickness of the muscle tissue of the uterus, so excess production of estrogen by the ovaries may be associated with tumor growth. The genetic information contained in the cells also causes various abnormalities of the reproductive system. Doctors include a woman’s lifestyle and individual history as additional etiological factors.
Possible reasons:
- Transmission of hereditary mutations. Studies have confirmed that individual gene mutations cause excessive growth of uterine muscle tissue. In this regard, uterine fibroids can be a hereditary pathology.
- Hormonal changes. The mucous and muscular lining of the uterus develops under the control of female sex hormones. Estrogen and progesterone act on the uterus during the menstrual cycle to prepare the reproductive system for pregnancy. It has been proven that tumor cells are more sensitive to these sex hormones, so excessive endocrine stimulation causes rapid growth of fibroids. At the same time, after menopause, characterized by a decrease in hormone production, the tumor decreases.
- Imbalance of other tissue regulatory factors. This may be an excess of insulin-like growth factor caused by pathologies of the hypothalamus, pituitary gland or liver.
Scientists believe that uterine fibroids develop from stem cells of the smooth muscle tissue of the organ, which are responsible for the regular renewal of the median lining of the uterus. Due to dysregulation, one stem cell begins to divide multiple times, resulting in the formation of an abnormal focus of muscle growth. The growth pattern of fibroids varies: the tumor can grow slowly over decades or multiply in size in just a few months. Often, previously detected tumors disappear without treatment within several years.
Antigestagens
This group of drugs blocks the action of progesterone at the receptor level. , which leads to increased contractility of the myometrium.
The group includes the drugs Mifepristone and Esmya.
Mifepristone has an antigestagenic effect and is a synthetic steroid. The active component of the drug activates the myometrium, increasing its tone and contractility. Once in the blood, the medicine does not allow progesterone to be released. The drug does not have gestogenic activity. Used for the treatment of uterine leiomyomas up to 12 weeks of pregnancy.
Risk factors
In addition to the direct causes of tumor formation, doctors need to take into account various risk factors associated with heredity, lifestyle and the woman’s individual history. Various forms of predisposition to uterine fibroids can be found in almost any mature woman.
Possible risk factors:
- Unfavorable family history. If a close relative of the patient was diagnosed with a benign uterine tumor, the risk of individual morbidity increases.
- Early onset of menstruation and late menopause. This factor causes a large number of menstrual cycles.
- Using hormonal medications, such as oral contraceptives. External influence on hormonal levels can cause the development of the disease.
- Wrong diet. Lack of vitamin D in the diet and excess consumption of red meat adversely affect the condition of the female reproductive system.
- Obesity and sedentary lifestyle.
- Bad habits. Alcoholism and smoking negatively affect all organs and tissues. In particular, frequent consumption of beer is a direct risk factor for uterine fibroids.
- Hereditary leiomyomatosis is a rare hereditary syndrome that causes the growth of tumors in various organs. Fibroids can also form.
Taking into account risk factors affecting women's health allows for timely detection of benign tumors and implementation of prevention.
From which it decreases
Only pituitary hormones can have an inhibitory effect on the tumor process. They are called gonadotropic, that is, affecting the sex glands - gonads. These include follicle-stimulating and luteinizing. It has long been known that during menopause, when they are elevated, fibroids resolve. The release of gonadotropins into the blood is provided by the gonadotropic releasing factor of the hypothalamus. Therefore, by introducing its analogue from the outside, tumor growth can be stopped.
The disadvantage of these hormones to reduce formation is that they cannot completely change hormonal levels. Although their effect is long-lasting, after its cessation the tumor completely restores its ability to grow.
In addition, they create an artificial menopause in the body with its manifestations - hot flashes, sweating, vaginal dryness, sexual desire disorders, bone tissue destruction. Because of these effects of hormones, the use of these drugs is advisable only for preoperative preparation.
Symptoms of menopause
Pathophysiology
Uterine fibroids are a type of smooth muscle tumors that develop in any part of the body (leiomyomas). It is a round, well-defined growth that is white or yellowish-brown in color. Large tumors cause severe symptoms and can be palpated from the abdomen. Many women develop microscopic fibroids throughout their lives that do not cause any complications.
In most cases, fibroid cells contain genetic or chromosomal mutations that are responsible for abnormal cell division and increased sensitivity to sex hormones. External cell structures (receptors) respond to estrogens and stimulate tumor growth. In women who do not suffer from hormonal disorders, uterine fibroids are also diagnosed, but in this case the tumors rarely reach significant sizes.
Doctors are aware of the rare phenomenon of ectopic fibroid growth. Sometimes this form of the disease is called metastasizing fibroids. Unlike malignant neoplasms, such structures rarely lead to dangerous complications. The spread of tumor cells to other organs may be associated with surgery to remove the tumor: excision of the affected tissue is accompanied by the penetration of individual cells into the bloodstream. At the same time, the effect of sex hormones on all parts of the body stimulates the growth of “metastases” in various tissues and organs.
Tumor migration options:
- Myoma of a blood vessel. The growth of a tumor in the veins is dangerous due to the possible migration of the pathological focus to the heart.
- Formation of “metastases” in the lungs and lymph nodes. Damage to lung tissue is also considered a dangerous complication.
- Disseminated intraperitoneal leiomyomatosis, in which tumors grow on the omental and peritoneal surfaces.
In very rare cases, prolonged ectopic growth of fibroids increases the risk of malignancy.
Phytoestrogens as an alternative
If there are contraindications to hormone replacement therapy or a woman is unwilling to take such medications, the doctor may prescribe herbal remedies. We are talking about phytohormones that have estrogen-like activity (Klimadinon, Klimonorm and others). Such drugs are used mainly during menopause to eliminate hot flashes. According to women's reviews, phytoestrogens really help to cope with the unpleasant sensations of menopause and get through this period of life with dignity.
Plant analogues of sex hormones are well tolerated and are considered practically safe, but their use is not justified in case of fibroids. The estrogen-like activity of the mentioned drugs plays against the woman, and tumor growth is observed against the background of their use. Phytoestrogens, as a rule, are not prescribed for fibroids due to the possible risk of disease progression.
An interesting video about a modern view of drug treatment of benign neoplasms
Symptoms
The symptoms of the disease depend on the size and location of the benign tumor. In most cases, women develop a small tumor that does not cause any symptoms. Small lesions can maintain their size until menopause, as a result of which the anomaly does not affect reproductive function in any way. On the contrary, large tumors negatively affect the functioning of the reproductive system and cause unpleasant sensations associated with compression of neighboring organs and tissues.
Possible symptoms and signs:
- heavy menstrual bleeding;
- uterine bleeding during menstruation continues for 8 or more days;
- pain in the perineum, anus and lower abdomen;
- bloating;
- disturbance of urination, feeling of incomplete emptying of the organ;
- frequent urge to urinate;
- retention of stool in the intestines (constipation);
- pain spreads to the back and lower extremities;
- sudden cramping pain.
Rarely, large fibroids can cause severe pain when they compress the arteries that supply blood to the uterine tissue. This dangerous complication requires immediate treatment.
Diagnostics
If unpleasant symptoms associated with the uterus and menstrual irregularities appear, you must make an appointment with a gynecologist. The doctor questions the woman and clarifies the anamnestic information to identify risk factors for the disease. An initial examination of the uterus, including palpation (feeling) of the organ, sometimes reveals a large tumor. For a more accurate diagnosis, the gynecologist prescribes instrumental and laboratory examinations.
Additional diagnostic methods:
- Instrumental gynecological examination. The gynecologist asks the woman to sit in a special chair. Then the doctor carefully expands the lumen of the cervix and inserts an endoscope equipped with a light source and camera into the organ cavity. Using hysteroscopy, the gynecologist examines in detail the internal structure of the uterus and detects any abnormalities.
- Ultrasound hysterosalpingoscopy. The doctor injects a special liquid into the uterine cavity and uses an ultrasound machine to assess the condition of the organ. This is a safe and painless test. A transducer that emits high-frequency sound waves creates an image of the uterus and fallopian tubes on a monitor.
- Probing of the organ. The gynecologist records the position of the cervix and inserts a special instrument into the organ. From the area of the cervix, the probe gradually moves towards the fundus of the uterus. Using probing, the doctor assesses the shape of the organ cavity and the patency of the uterine tract. This is a very important study in preparation for surgery.
- Ultrasonography. The pelvis contains the reproductive organs, so a specialist conducts research in this area. The doctor lubricates the skin with gel and applies a special sensor to obtain an image of the organs on the monitor. Ultrasound of the uterus allows you to detect large tumors and assess the condition of the organ. Most often, this is an initial examination, after which the gynecologist decides on the direction of further diagnostics.
- Computed tomography or magnetic resonance imaging are highly accurate visual diagnostic methods that enable the doctor to obtain layer-by-layer images of organs. The results of CT and MRI are necessary for a detailed study of the reproductive system and the search for ectopic foci of tumor growth. During the examination, the patient lies motionless on the tomograph table. Before taking a photo, you must remove all metal objects from yourself.
- Blood analysis. The nurse collects venous blood from the patient and sends the material to the laboratory. Specialists evaluate the amount and ratio of formed blood components, the concentration of sex hormones and identify specific tumor markers. Blood tests can also help identify complications of heavy menstrual bleeding.
A comprehensive diagnostic search is important to detect all tumors and carry out treatment. The listed studies are also carried out to screen for diseases of the uterus if the gynecologist discovers risk factors for oncology of the reproductive system in the patient.
Conservative treatment
The method of treating uterine fibroids depends on the patient’s age, size and location of the tumor. Small tumors that do not cause complications do not need to be removed. In this case, the gynecologist prescribes regular examinations, including visual and laboratory diagnostics. It is necessary to monitor the rate of tumor growth and the condition of the reproductive organs. If the tumor causes discomfort, treatment is carried out. Drug therapy can prevent further growth of fibroids.
Methods of treating the disease:
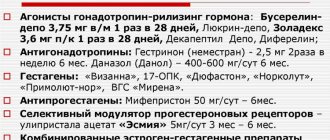
- Prescription of gonadotropin-releasing hormone agonists. These hormonal drugs prevent further tumor growth by blocking the production of estrogen and progesterone. The patient temporarily stops menstruating. The positive effects of such therapy can also include the elimination of anemia. The course of treatment with gonadotropin-releasing hormone agonists varies from several weeks to several months.
- Prescription of tranexamic acid. This is a non-hormonal drug that relieves heavy uterine bleeding during menstruation.
- Selection of additional medications depending on the patient’s condition. The gynecologist may prescribe oral contraceptives, progestogens and painkillers. Anemia requires a change in diet and administration of iron supplements.
A monthly injection of gonadotropin-releasing hormone agonists helps reduce fibroid size by 40-55%. However, such therapy can lead to bone damage in young women, so doctors carefully monitor their patients' condition.
Gonadotropin releasing hormone (GnRH) agonists
They have an inhibitory effect on the production of gonadotropin, which causes artificial menopause in the patient, which in 50% is accompanied by regression of myomatous nodes. The products in this group include: “Decapeptyl”, “Zoladex”, “Buserelin”, and others. The drugs have side effects such as:
- tides;
- increased sweating;
- depressive states;
- decreased libido.
To minimize such events, doctors use minimal doses of estrogen or intermittent agonist regimens.
Surgery
Unfortunately, therapy can only temporarily stop the growth of fibroids, so the only radical way to remove the tumor is surgery. Surgical treatment is mandatory for large fibroids, severe pain, constant bleeding and complications of the disease. Modern technologies make it possible to carry out safe and non-traumatic interventions characterized by a low risk of relapse. When selecting a surgical procedure, the gynecologist takes into account the patient’s age, size and location of the tumor.
Operation options:
- Laparotomy is the removal of uterine nodes using abdominal access. This is a traditional method of surgical treatment of fibroids, performed for large, deep tumors.
- Endoscopic interventions by inserting instruments through the cervix. This low-traumatic treatment is suitable for removing tumors located in the mucous membrane of the organ. Laparoscopy is also used.
- Tumor ablation. The specialist inserts a special instrument into the uterus that destroys the pathological focus using electricity or microwave radiation. This method of treatment does not lead to extensive damage to organ tissue.
- Embolization of vessels feeding a benign neoplasm. This is a relatively new and effective treatment method. The uterine arteries are occluded using catheterization.
- Removal of the uterus is a radical method of treating the disease, prescribed for large tumors, severe complications of fibroids and frequent relapses. This traumatic intervention leads to infertility and disruption of hormonal regulation, so gynecologists most often prescribe such treatment to women over the age of 45.
Often, for safe and effective surgery, it is necessary to first use conservative treatment methods.
Complications
Without treatment, uterine fibroids can grow over many years and gradually cause dangerous complications. The disease adversely affects the reproductive functions and general well-being of a woman.
Possible complications:
- Anemia is a lack of hemoglobin in the blood caused by excessive uterine bleeding. Symptoms of the pathology include pale skin, constant weakness, fatigue and dizziness.
- Attachment of the embryo in the area of submucosal fibroids followed by miscarriage. Muscle tumors also increase the risk of premature birth or placental abruption.
- Tumor metastasis. This rare complication occurs when large numbers of tumor cells enter the bloodstream. Components of the neoplasm can enter any organ and form new pathological foci under the influence of hormones.
If complications are detected, fibroids must be treated with surgery.
Prevention
A woman can avoid the development of diseases of the reproductive system with the help of medical recommendations.
The main ways to prevent uterine fibroids:
- Taking hormonal contraceptives and other drugs that affect the reproductive system only under the supervision of a doctor.
- Diet changes: avoiding excess consumption of meat, adding vegetables and fruits to the daily diet.
- Regular gynecological examinations (at least once a year).
To prevent relapse of the disease after treatment, a woman needs to regularly monitor her hormone levels.
Admission rules
What medications a woman should take and the regimen is determined by the attending physician. But there are several rules that must be followed while taking medications:
- The tablets are taken on an ongoing basis (sometimes in courses with a minimum break of 7 days).
- It is necessary to take into account the daily rhythm of hormone production by the body. Tablets are taken during the period of the highest level of their production - in the first half of the day until 11:00.
- If oral contraceptives have been chosen among all methods of treating tumors, they must be taken in the evening to achieve maximum therapeutic effect.
Women must strictly follow all doctor's recommendations and take the medicine at the exact time indicated.