Take the first step
and make an appointment with your doctor!
After conceiving a child, multiple changes begin to occur in a woman’s body, the purpose of which is to make pregnancy and birth more likely. They manifest themselves at all levels, from the anatomy of the genital organs to metabolism and hormonal levels. One important aspect is changes in the cervix during pregnancy. A woman who does not know about them can often mistake the normal processes happening to her for pathological ones and vice versa.
Cervix: structure and functions
This organ is the lower segment of the uterus, through which passes the narrow cervical canal connecting the uterine cavity and the vagina. The normal length of the cervix is 3-4 cm, its outer part protrudes into the vagina and, at the junction with its walls, forms the vaginal fornix, which serves as a kind of reservoir for sperm. The vaginal segment is dome-shaped and covered with pink stratified squamous epithelium. The cervical canal, on the contrary, is lined with columnar epithelium, which has a brighter shade. The color of the vaginal segment of the cervix is one of the criteria for its health.
In a woman’s reproductive system, this organ performs several important functions:
- protects the uterine cavity from penetration of pathogenic organisms, as well as from sperm (after conception) by closing the cervical canal with a “plug” of glycoprotein mucus;
- promotes the penetration of sperm during the ovulation period, filtering the most viable of them with a counter current of mucus produced by the glands of the cervix;
- ensures free outflow of blood and desquamated endometrial cells from the uterine cavity during menstruation;
- prevents premature birth of the fetus during pregnancy and promotes its correct passage through the genital tract during childbirth.
The condition of the cervix is an important diagnostic indicator that allows you to determine the presence of pregnancy or various pathologies of the female reproductive system. To do this, the gynecologist evaluates such characteristics as the color, size and consistency of the vaginal part, the diameter of the cervical canal, and its position relative to other genital organs (the uterus itself, vagina, etc.).
Take the first step
make an appointment with a doctor!
Diagnosis of cervical pregnancy
During diagnostic studies, it is necessary to differentiate cervical pregnancy from other pathologies:
- myoma;
- uterine fibroids;
- miscarriage.
Uterine fibroids (fibroids) are characterized by the absence of a positive pregnancy test and are not characterized by a delay in menstruation. With spontaneous abortion, pain in the lower abdomen and sacral area appears, as well as cramping pain.
To diagnose cervical intrauterine pregnancy, a gynecological examination is performed, which reveals cyanosis of the cervix, displacement of the external os and fertilized egg to the walls of the cervical canal. The size of the cervix is increased and exceeds the volume of the uterine body. With instrumental separation and palpation of the fetal egg, bleeding is noted.
Cervical pregnancy, ultrasound allows you to determine the expansion of the cervical canal, within which the fertilized egg is differentiated, very clearly visible during this examination. Also, during an ultrasound examination, the presence of placental tissue of the cervical canal and hyperechogenicity of the endometrium are detected.
In frequent cases, diagnosis of cervical pregnancy is carried out during uterine curettage surgery. This surgical intervention is performed according to clinical indications indicating spontaneous abortion. During surgery, removal of the fertilized egg is difficult, bleeding is observed during curettage and after surgery; a crater-shaped depression in the walls of the uterus is diagnosed.
In the isthmus-cervical form of ectopic pregnancy, there are no clinical signs during vaginal diagnosis. This type of distal pregnancy can be assumed by observing bloody discharge from the vagina. With increasing gestational age, bleeding is profuse, there is no pain.
What is the cervix like during pregnancy?
During the entire period of gestation, many changes in the cervix are observed. This is influenced by factors such as:
- individual characteristics of the structure of the genital organs of a particular woman;
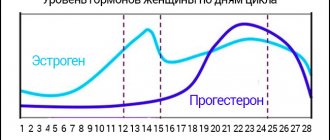
- hormonal balance (concentration of female sex hormones - estriol and progesterone);
- the weight of the fetus (or fetuses in multiple pregnancies) exerting pressure on the cervix;
- the presence of uterine pathologies, injuries and other defects.
Let's look at how the characteristics of the cervix change during pregnancy, provided that the woman is absolutely healthy:
- Size. Immediately after conception and until approximately the second half of pregnancy, the cervix lengthens. So, at the 24th week, its normal length is about 3.5-5 cm. However, then as the fetus grows, it shortens - at 28 weeks to 3.5-4 cm, and at 32 weeks - to 3-3 .5 cm. Ultrasound scanning of the length of the cervix can help track these changes. If the woman is healthy, then this procedure is not performed. However, if she has a complicated pregnancy or has had miscarriages in the past, she is given an ultrasound scan, as an excessively short cervix can trigger premature labor. Also, during pregnancy, the diameter of the cervical canal changes. Normally, it remains completely closed throughout pregnancy and opens only immediately before birth. Thanks to this, the uterine cavity and fetus are reliably protected from infections. Dilation of the cervix too early can also cause miscarriage. This risk is due to too short an organ, muscle weakness or too much weight of the fetus (as well as multiple births).
- Color. Before pregnancy, provided the woman has no pathologies (for example, erosion), the cervix has a pink tint. After conception, the number of blood vessels in it increases, which is why the color changes to bluish. Assessment of color is one of the additional criteria that allows you to determine the presence of pregnancy during a gynecological examination (hysteroscopy).
- Consistency. The cervix before pregnancy has a dense texture; after conception, under the influence of sex hormones, it becomes softer. The glands in the cervical canal begin to produce a large amount of mucus, which forms a “plug” that reliably seals the uterus and fetus for the entire period of gestation. Shortly before birth, when the cervix begins to dilate, this formation separates and comes out naturally, freeing the passage for the fetus.
Normal physiological changes in the cervix vary depending on the individual characteristics of the woman's body. For example, some of them may experience reduced secretion of mucus by the cervical glands, while others may experience a slight change in length during pregnancy. If some changes occur to a not too pronounced degree, this does not mean the presence of any pathology or high risk for the mother and fetus. However, at the doctor's discretion, he may order more frequent cervical monitoring to rule out this possibility.
Take the first step
make an appointment with a doctor!
Pathological changes in the cervix
Such changes are all those that go beyond the accepted physiological norm. The most common ones include:
- Isthmic-cervical insufficiency (ICI). This disorder consists of premature and asymptomatic shortening of the length of the cervix and its dilatation. The causes of ICN are multiple pregnancies, high fetal weight, insufficient tone of the uterine muscles, hormonal disorders, and injuries. If the pathology seriously threatens the fetus, the doctor may prescribe suturing (cerclage) of the cervical canal or placing a special bandage (pessary) around it. When ICN is mild, injections of progesterone are used, which increase the tone of the uterine muscles and thicken the endometrium.
- Neoplasms. Often, during routine examinations of a pregnant woman, cervical polyps are discovered. These are usually benign formations, which are outgrowths of the epithelium on thin “legs”. With their small number and size, they usually do not pose a danger. However, the growth of polyps threatens bleeding, pain, and inflammation. In rare cases, this tumor can develop into a malignant one - cervical cancer. If polyps are detected during pregnancy, a wait-and-see approach is used. If the tumors remain small and their number is small, surgical treatment is not performed. Removal of polyps is prescribed only in extreme cases, when their danger to the woman or fetus is obvious.
- Cervical erosion. Often this term refers to two pathologies that are different in nature, although similar in symptoms. Ectopia (pseudo-erosion) is the growth of the cylindrical epithelium of the cervical canal onto the vaginal part of the cervix. True erosion is a violation of the integrity of its mucosa, resulting from inflammation, infections, trauma (for example, during sexual intercourse). Both types of pathology manifest themselves as redness of the vaginal part of the cervix and may be accompanied by uncomfortable and painful sensations and light bleeding. As a rule, cervical erosion is not treated during pregnancy, since it does not threaten the life of the woman or the fetus and does not complicate the process of pregnancy and childbirth. Treatment is prescribed only if there is a risk of developing cervical cancer. Typically, it involves taking anti-inflammatory drugs.
Also abnormal and pathological changes include injuries to the cervix, inflammation, infection, formation of cysts in the glands of the cervical canal, etc. If they do not directly threaten the mother and her fetus, or do not complicate the course of pregnancy, then their treatment is postponed until delivery. Expectant management is used because during the gestation period the mother’s body is especially susceptible to various influences, including surgical and medicinal ones.
Take the first step
make an appointment with a doctor!
Treatment of cervical pregnancy
Initially, after diagnosis and detection of cervical pregnancy, the woman is urgently hospitalized. Further treatment consists of stopping bleeding. To do this, use a tight vaginal tamponade, which is sewn on the sides. A circular suture is also placed in the cervical area, and a Foley catheter is inserted into the cervical canal. During the treatment of cervical pregnancy, embolization of the branches of the uterine arteries is also used, and the internal iliac arteries are also ligated. Such methods allow you to remove the fertilized egg.
In individual cases, hysterectomy is performed. This method of treatment is carried out in individual clinical cases when it is impossible to stop bleeding and save organs. Extirpation of the uterus is indicated in the absence of positive dynamics after surgical procedures.
Detection of cervical diseases
To determine the presence or absence of pathological changes, the doctor conducts a screening examination of the cervix, including:
- cytological examination - analysis of particles of the epithelium of the cervix and cervical canal for the presence of atypical cells, including cancer cells;
- microflora smear - analysis of vaginal or cervical mucus for the ratio of beneficial, opportunistic and pathogenic microorganisms, indicating the general condition of the body, the reproductive system, the presence or absence of inflammatory diseases;
- smear for infection - examination of the mucous discharge from the vagina for the presence of clearly pathogenic microorganisms (viruses, bacteria, fungi, protozoa), indicating the presence of an infectious process in the genital tract.
Also, as part of a screening study, hystroscopy may be prescribed - a visual examination of the cervix using a thin and flexible instrument equipped with a camera or optical system (hystroscope). It is inserted directly into the vagina and cervical canal, allows you to evaluate the color and thickness of their mucous membranes, determine the presence of polyps and other neoplasms, the size of the cervical lumen, etc.
The combination of these methods gives doctors the opportunity to determine the general condition of a woman’s body and her reproductive system, and promptly identify possible pathologies and complications. This increases the likelihood of their successful treatment, including gentle conservative methods.
Causes
The reasons why an embryo decides to attach itself in the wrong place are different and all of them are associated with pathology that prevents the normal attachment of the egg in the uterus.
The embryo descends further into the lower parts of the reproductive system, in particular into the cervix. Here, the site of its introduction is not the endometrium, but the mucous membrane of the cervical canal.
Doctors suggest that one of the reasons that causes the embryo to move into the cervix is a previous medical abortion. This pathology can also be caused by fibroids located in the uterine cavity.
Previous births via cesarean section may prevent the embryo from implanting normally in the uterine cavity. With a large number of adhesions in the uterine cavity, the embryo also has no place to implant and is forced to look for another place. In rare cases, cervical pregnancy occurs when the structure of the uterus is abnormal.