When asked whether an endometrial polyp can resolve or come out on its own with menstrual blood, doctors answer in the negative. The possibility that an endometrial polyp can disappear on its own, theoretically, cannot be excluded. But, as medical practice shows, such benign formations do not resolve on their own and require drug treatment or, in large cases, surgical intervention.
The influence of the polyp on the cycle
The neoplasm has a negative impact on sexual health. The nature of the menstrual cycle will largely depend on the location of the growth. Signs of a polyp in the uterine cavity (endometrium):
Abnormal tissue growth in the cervical canal of the cervix causes the following:
- bleeding during sex;
- scanty periods;
- brown color bleeding.
Among the common signs it is worth highlighting:
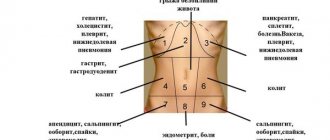
- pain in the abdominal area;
- intermenstrual bleeding;
- cycle failure.
In some situations, the damaged tumor begins to become inflamed, which is why purulent discharge appears on any day of the month.
There are also other types of polyps:
- glandular;
- fibrous;
- adenomatous;
- placental (after pregnancy, miscarriage on the remnants of the placenta).
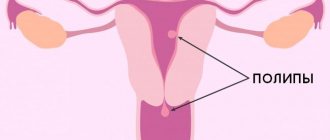
Uterine polyp - what is it?
A benign neoplasm that resembles a mushroom. It has a leg and a head with a diameter from a few millimeters to 3 cm. The average size is 10 mm. Appears in the internal cavity of the uterus - the endometrium or inside the cervical canal. Formations can occur at any age starting from 10 years, when the body is just preparing for menstruation. Most often formed in women before menopause. There are single and multiple.
- Failure of the menstrual cycle with delay, bleeding;
- Bloody discharge after sexual intercourse, as a result of touching polyps;
- Leucorrhoea in large quantities;
- Lower abdominal pain;
- Discharge mixed with blood between periods; infertility.
Polyps develop asymptomatically for a long time, and irregular periods cause concern. It is precisely this problem that women turn to a gynecologist. Large polyps are detected during examination, small polyps are detected on ultrasound. They are not life-threatening, but in 2% of cases they degenerate into a malignant tumor. In this regard, treatment of uterine polyps begins immediately after detection.
Spontaneous disappearance of the polyp
The polyp may come out with menstruation, but this happens in rare cases. No photo will help to understand whether it was a growth or an ordinary blood clot. You should not hope that the growth will resolve on its own. Without treatment, the risk of relapse increases because the trigger has not been eliminated.
Often the first ultrasound gives a false result when endometrial folds are perceived as pathology. Therefore, doctors prescribe a repeat examination.
There is an opinion that traditional medicine or biological supplements are unable to completely eliminate the problem of abnormal tissue growth.
Small growths
A polyp up to 1 cm in diameter can come out along with menstruation, but only after appropriate treatment. In medical practice, there are cases of spontaneous release, but most often the growth does not completely disappear. Therefore, it is important to go to the hospital in time for any symptoms to avoid polypectomy.
Treatment options
Therapy is selected based on the underlying cause and age of the patient.
Hormone therapy
Polyps in the early stages of development are eliminated with hormonal drugs over several months. The main selection criteria are age and health status.
Up to 35 years - combined oral contraceptives (estrogen + progesterone):
Find out why periods are sometimes delayed after Regulon by clicking on the link. Premenopause - progestin pills:
Find out about the nature of menstruation after Norkolut in the article at the link. Menopause period:
Important! When hormonal therapy does not produce results, it is necessary to select other treatment methods.
If the tumor grows, the doctor will tell you on what day of the cycle the endometrial polyp is removed. In most cases, the procedure is prescribed after menstruation.
Other drugs
You can cure a growth without surgery not only with hormones. Drugs are selected based on the cause of tissue proliferation. Antibiotics help if the problem is caused by pelvic inflammation and if there is a sexually transmitted infection.
The following drugs are used:
- Gentamigin;
- Doxycycline;
- Zitrolide;
- Tetracycline;
- Tinidazole;
- Ornidozole;
- Gentamigin;
- Erythromycin.
As maintenance therapy, the doctor prescribes iron tablets and vitamin complexes. This helps prevent anemia due to severe blood loss, as well as improve the patient’s immunity. If you take homeopathic remedies and traditional medicine, then they are allowed, but only after agreement with the treating specialist.
When is surgery necessary?
Surgery is necessary in the following cases:
- large size of the growth;
- no improvement after taking hormones;
- severe uterine bleeding;
- suspicion of cancer;
- age after 40 years.
The importance of the day of the cycle for the operation
On exactly which day of the cycle a hysteroscopy is performed to remove a polyp, only a doctor can answer. In the medical field, they are confident that the best time for surgery is the second or third day after the end of menstrual flow. The deadline should not exceed ten days after menstruation.
This approach is justified by the fact that during this period the mucous layer of the uterus is at its thinnest. Therefore, it is easier for the gynecologist to recognize the tumor for precise removal.
Basic methods
Modern gynecology offers several ways to remove polyps:
- Hysteroscopy. Hysteroresection allows you to most accurately assess the condition of the genital organs and completely remove the tumor at the root. After the main hysteroresectoscopy procedure, the doctor performs cauterization.
- Curettage. An outdated method that is used extremely rarely. It is useful for polyposis, when you need to scrape out several formations at once using a curette.
- Laser. The safest method that reduces the risk of infection and bleeding. But not all medical institutions have a laser scalpel.
- Laparoscopy. The operation through a small incision in the abdominal cavity involves the removal of the uterus. It is carried out if atypical cells have been detected or there is a high probability of cancer.
There is also endometrial ablation, but after this procedure the woman will never be able to have children. Therefore, this method is intended for patients during menopause.
Scraping during menstruation
During monthly bleeding, it is not advisable to perform surgery for the following reasons:
- menstrual flow interferes;
- too thick endometrium;
- inability to thoroughly examine the received materials.
It should be noted that the answer to the question whether it is possible to remove a polyp during menstruation is ambiguous and there are exceptions when the procedure is still carried out:
- In order to stop heavy blood loss.
- When the growth is located on the cervix.
In the first case, it is impossible to postpone the procedure until the end of menstruation. In the second situation, there is a significant opening of the cervical canal. It is easier for the surgeon to determine the boundaries of the tumor and capture it with a special device.
Therefore, you should not be surprised if, after asking on what day of the cycle the cervical canal polyp is removed, the doctor does not rule out surgical intervention on critical days.
How to prepare for surgery?
Removing a polyp does not require any serious preparation, but there are some restrictions.
A week before the procedure, it is recommended to refrain from intimacy. Also undesirable :
- douching,
- candles,
- vaginal tablets,
- medicinal tampons.
On the eve of the operation, it is recommended to eat easily digestible food. It is necessary to give up black bread, cabbage, and legumes. In the evening, instead of dinner, it is better to drink a glass of kefir.
On the day of surgery, breakfast and any kind of liquid are excluded.
What tests need to be taken?
Before surgery, each patient undergoes such diagnostic procedures:
- Examination on a gynecological chair using a mirror; the doctor evaluates the cervix for inflammation and other damage, examines the cervical canal through which instruments will be inserted during removal;
- Cytological examination of a smear to exclude malignant processes;
- Bacteriological examination of a smear to exclude a bacterial infection, because there is a risk of introducing it into the uterus, which may result in the development of endometritis;
- Transvaginal ultrasound, which reveals the location and size of polypous lesions;
- General clinical examination (general and biochemical blood test, urine test, electrocardiogram, fluorography, test for HIV and viral hepatitis, microreaction to syphilis).
Only after the results of all the above tests is the patient allowed to undergo surgery.
Menstruation after tumor removal
When the polyp no longer harms the woman’s health, the recovery period begins. At this time, the patient must take care of herself and strictly follow the instructions of the attending physician. The rate of normalization of the functioning of the sexual sphere depends on the following factors:
- Removal method. The less intervention, the faster the woman recovers.
- Age. A young body and reproductive system return to normal after 35–40 years in different ways.
- Additional factors. Rest, following specialist recommendations and general health play an important role.
When does your period start?
The onset of menstruation after curettage of a polyp often falls on the next cycle. Permissible deviation is 1.5 months (40–50 days). Menstruation begins faster after the removal of cervical growth due to less stress on the body.
A long delay of a non-pathological nature may be associated with the patient’s age and hormonal status. If bleeding persists for more than two months, you must:
- take hormone tests;
- do a vaginal smear;
- undergo an ultrasound.
It is important to exclude progesterone deficiency in time. The lack of this hormone not only disrupts the cycle, but also provokes relapse of the polyp.
Nature of bleeding
Features of the first menstruation after polyp removal will depend on the location of the tumor:
Cervical canal
There is scanty menstruation due to the use of antibiotics. Intermenstrual discharge should completely disappear, but spotting is allowed for a week after surgery. It is important not to allow liquids to linger. After all, they can cause an inflammatory process.
Uterine cavity
Menstruation after removal of an endometrial polyp is heavy and accompanied by pain. In the middle of the cycle, there is normally no brown discharge. Long menstruation (over 10 days) indicates incomplete removal of the growth. In this case, repeated examination and intervention is required.
When doctors have removed a polyp, it is important to rule out endometritis, endometrial hyperplasia.
Without eliminating these diseases, you can forget about the normal functioning of the reproductive system. The risk of recurrence of the polyp after treatment increases.
Can a polyp come out with menstruation?
Despite the fact that traditional healers assure that it is possible to get rid of a polyp with herbs, doctors state the complexity of such a problem and even hormonal drugs do not always manage to get rid of the scourge completely, but only to achieve its separation from the walls of the uterus.
An independent release of a polyp is simply impossible.
In rare cases, it happens that it resolves spontaneously, but one cannot hope for this and wait for it to degenerate into a malignant tumor. Women are strongly advised to consult a doctor and undergo a histological examination to avoid the development of oncology.
Prevention
A uterine polyp most often appears against the background of hormonal disorders and improper functioning of the ovaries; to prevent the development of this disease, hormonal imbalance should be avoided and inflammatory and infectious diseases should always be treated. There are also a number of other preventive measures, the observance of which can prevent pathological growth of epithelial tissue:
- do not eat foods contaminated with dioxide, as well as meat containing hormones;
- you should choose a place of residence in an ecologically clean area;
- you must not overcool or overheat, clothing must be selected according to the weather, you do not need to sit on cold surfaces;
- you should streamline your sex life and avoid unprotected sexual intercourse;
- actively engage in sports to prevent blood stagnation in the genitals;
- take medications, including hormonal contraceptives, as prescribed by a doctor;
- visit a gynecologist for preventive purposes.
Drug treatment
Polyps are not just growths on the skin or mucous membrane in the uterine cavity. These are proliferations of cells modified by viruses. Such structures are prone to malignancy - degeneration into a cancerous tumor.
It is possible for doctors to prescribe medication with painkillers for cramps and abdominal pain caused by compression of the nerve endings in the tissues by the polyp. The following drugs are usually indicated:
In addition, antiseptics are prescribed to eliminate bacterial complications that lead to pain in the lower abdomen and the discharge of bloody discharge with clots:
To avoid the proliferation of pathogenic microflora and infection in the uterine cavity, the following therapy is prescribed locally:
- means for irrigation of the uterine cavity;
- enemas;
- hormonal drugs to correct the level of progesterone and estrogen in the blood.
Treatment with medications has the following advantages:
- allows you to eliminate unpleasant symptoms;
- stops bleeding typical of polyps in the uterus;
- prevents the development of infertility.
Taking hormonal drugs during pregnancy is contraindicated. This is dangerous for the fetus, although the polyp itself does not have much effect on the pregnancy process. Women are still recommended to plan a pregnancy and undergo a full examination before conceiving a baby.
Reasons for education
Doctors still cannot come to a consensus on why polyps appear; today there are several versions regarding the reason for the appearance of this benign formation, each of which has the right to exist:
- hormonal imbalance. The growth of the inner uterine layer can be triggered by high levels of estrogen in the blood. The endometrium can grow in patches in the form of polyps or evenly, then endometrial hyperplasia is diagnosed. With a lack of progesterone, tumors grow more actively;
- proliferation of blood vessels. When a vessel becomes clogged and grows, epithelial cells can grow uncontrollably around it;
- inflammation of the genital organs (cervicitis, endometriosis). During inflammatory processes, the number of leukocytes in the tissues surrounding the uterus increases. On the one hand, they fight infection, on the other, they promote the growth of the endometrium;
- abortions and failed curettages. If the operation is performed poorly, this provokes the formation of erosions and increased growth of mucosal cells in certain areas;
- endocrine diseases that lead to malfunction of the thyroid, liver or adrenal glands, causing excessive production of hormones;
- hereditary predisposition;
- low physical activity causes the development of the disease due to stagnation of blood in the pelvic organs;
- neoplasm can occur while taking certain drugs, especially tamoxifen, which fights cancerous tumors, but provokes the growth of polyps.
Other treatments
Unfortunately, removing a polyp with medications alone is almost impossible. Taking into account their size and progression, to slow down the growth of the tumor, doctors often resort to hysteroscopy as the most effective and safest method today. It is performed by introducing a video camera with a tube into the uterine cavity, and removal of the formation is carried out by exposing the polyps to high-frequency waves.
Some doctors are still guided by the old method - curettage of polyps from the uterine cavity during surgery under anesthesia. This method is ineffective and painful for the following reasons:
- damages the walls of the uterus;
- leads to bleeding;
- causes complications due to it being carried out almost blindly.
In addition, during curettage, there is a high probability that polyps will not be completely removed. Then you will need to repeat this operation or treat it in a different way.
Regardless of the prescribed method, when adenomatous polyps are identified, surgery cannot be avoided.
Of course, it is impossible to wait for their degeneration into a malignant tumor. It is reasonable to treat with medications after surgery in order to prevent possible exacerbations and relapses in the future.
Diagnostics
If a woman develops the uncomfortable symptoms listed above, only a gynecologist can determine what to do in a particular case. A number of diagnostic measures are carried out to confirm the diagnosis.
If there is a suspicion of malignant processes in the neoplasm, an additional biopsy and subsequent histology of the polyp may be performed.
Examination by a gynecologist
The very first method of diagnosing any gynecological diseases is examination in a chair using mirrors. The doctor can detect protruding tumors. These may be red or pink growths that are round or grape-shaped. The cervix with this disease will be hypertrophied and thickened. The polyp may also be white if it is keratinized and covered with many layers of epithelial cells. If the growth is purple or burgundy, blood circulation in it is impaired. The polyp itself is soft and elastic.
Cerviscopy and colposcopy
Cerviscopy is performed using a hysteroscope and allows you to detect even the smallest polyp in the uterus, determine its structure and location. At the same time during the procedure, the doctor may take a biopsy and perform fractional curettage of the uterine wall. Using a colposcope, you can evaluate the condition of the cervix.
Ultrasound
If during a gynecological examination the doctor discovers a polyp on the cervix, then the woman is necessarily sent for an ultrasound examination, since there is a high risk of a growth appearing in the endometrium. The doctor examines not only the polyp on ultrasound, but also the condition of the tubes and ovaries, which will allow him to draw a complete picture of the disease.
Hysteroscopy
This is the most effective research method, during which a hysteroscope optical device is inserted into the uterine cavity. At its end there is a camera that transmits an image of the inside of the uterus to a computer monitor. Thanks to this technique, it is possible to determine the location of the growth, its size and the number of tumors. During the procedure, single polyps can be removed followed by morphological examination.
When does menstruation begin after removal?
Typically, menstruation begins 1.5 months after the operation. It all depends on the following factors:
- age;
- the patient's well-being;
- polyp size;
- their tendency to grow rapidly.
A direct role in when the period comes and how long the cycle will be delayed is played by how the woman follows the doctor’s instructions prescribed during the rehabilitation period. If the delay is more than 2 months, then you need to contact a gynecologist to prescribe hormonal drugs with progesterone.
Usually, a removed polyp leads to a change in the nature of menstruation. This is a completely normal reaction of the body to surgery. Most likely, the first periods will be heavy and painful, but in the intervals between them there should be no brown or colorless discharge.
Women need to be careful at first, not lift heavy objects, avoid stress. By the second cycle, your periods should return to normal. After eradicating polyps from the cervical canal, the first discharge usually appears on days 10-12, but this discharge has nothing to do with menstruation. The uterus is injured and even minor contact leads to bleeding from erosive areas that have not yet healed.
Normally, menstruation will begin 43-45 days after surgery. With extensive surgery and removal of many small polyps at once, the delay may be longer. If curettage was performed under anesthesia and nearby healthy tissue layers were affected, and not just those affected by the endometrium, then bleeding immediately after the operation may last more than 10 days. This is a sign that particles of neoplasms may have remained in the uterine cavity; the operation was performed poorly and not in full. Women need to see a doctor. Most likely, the procedure for cleaning the uterine cavity will have to be repeated.
Women need to take care and be more attentive to their health during the recovery period:
- dose physical activity;
- review your diet;
- Avoid sex for at least 2 weeks.
If side unpleasant symptoms appear, you should contact a doctor as soon as possible. The main thing is to take measures to restore the menstrual cycle after removal of polyps, minimize blood loss and prevent infection of the wound in order to avoid problems with conception in the future.
When a doctor suggests an operation to remove tumors, do not be afraid. If the procedure is performed efficiently and the polyps are eliminated in full, the uterus will soon quickly recover and the menstrual cycle will return to normal.
Polyp coming out during menstruation: myth or truth
Among gynecological diseases, a common pathology of the genital organs in women is the proliferation of polyps. The neoplasm is classified as a benign tumor. The peculiarity of the disease is the high probability of transition to a malignant form.
The pathology is treated primarily surgically; according to experts, other methods are ineffective. However, women often have a question about whether a polyp can come out with menstruation.
To understand whether such a phenomenon is possible, you should understand in more detail the characteristics of the disease and methods of its treatment.
A polyp in the uterus can appear in any woman
How polyps affect the cycle
The formation of growths can greatly affect the functionality of the reproductive organ system. Depending on the location of the formation, a woman sometimes has no symptoms of pathology, or, on the contrary, signs of the disease begin to appear.
Most often, when a polyp forms and increases in size, deviations in the menstrual cycle are observed. Menstruation, as a rule, becomes irregular, accompanied by severe pain and varies in consistency and volume of discharge.
Note! The cause of the disorders is changes in hormone levels under the influence of pathological processes.
If a growth forms in the cervix or tube, it begins to interfere with the natural flow of menstrual flow. During menstruation, not the entire layer of rejected endometrium may be released, so after menstruation or before it begins, a woman periodically experiences scanty discharge with a strong unpleasant odor.
A polyp can affect the intensity of discharge
In cases where the neoplasm is located on the outer wall of the uterus, menstruation is more abundant due to damage to the affected tissues, which begin to become inflamed as a result of sexual intercourse.
Experts do not identify clear characteristic changes in the menstrual cycle with polyps. The main symptom is considered to be a delay in menstruation and the presence of discharge in its absence.
What are the causes of a polyp?
A polyp cannot appear in the genitals without a reason. The main provoking factor is hormonal imbalance, the consequence of which is the inflammatory process of endometrial tissue.
Possible reasons:
- ovarian dysfunction;
- hyperestrogenism;
- excess weight or, conversely, anorexia;
- chronic sexual infections;
- injury to the uterus;
- surgical abortion;
- endometriosis curettage;
- long-term use of intrauterine devices;
Malfunction of the ovaries leads to the formation of polyps
- thyroid disease;
- severe stress;
- diabetes;
- age-related changes after 45 years;
- weakened immunity.
Medicine has not established the exact causes of the disease. As a rule, pathological neoplasms appear when several provoking factors are combined.
Can a polyp come out with menstruation?
There are many myths that a growth can resolve on its own, or that a polyp will come out during menstruation.
Important! The neoplasm attaches to the tissues of the organ and, under the influence of drug therapy, rejection occurs in exceptional cases.
Spontaneous release of a small tumor is allowed if there has been trauma to the tissue at the site of its attachment. However, there is a high probability of tumor detachment without attachment. In this case, after some time, a relapse occurs in the form of multiple growths.
This pathology requires examination and treatment.
According to doctors, polyps do not resolve on their own and do not leave the body either under the influence of drug therapy or under the influence of folk remedies.
What is the conservative treatment for polyps?
Beginning treatment for polyps involves conservative therapy. Taking medications is also required after the operation.
In case of painful sensations, a woman is prescribed medications that have an analgesic effect:
- Paracitamol;
- Ibuprofen;
- Diclofenac;
- Analgin.
To prevent the development of a bacterial infection, douching with drugs is prescribed:
- Potassium permanganate;
- Septadine;
- Collargol.
Additionally, hormonal medications can be prescribed, but only on an individual basis, taking into account the level of estrogen in the body.
What other treatment options are there?
It is impossible to limit yourself to drug therapy alone for polyps. Depending on the characteristics of the tumor, the method of surgical intervention is selected. The operation makes it possible to prevent relapses and eliminate the likelihood of developing cancer.
Hysteroscopy is performed to remove the polyp.
The operation can be performed using three methods:
- curettage - cleansing endometrial tissue manually (a painful method, often leading to relapse);
- hysteroscopy is a diagnostic procedure during which growths are removed using ultrasound;
- laser removal is a non-traumatic and effective method of removing polyps using laser beams.
The choice of treatment method depends on the capabilities of the clinic and the patient herself, as well as the presence of possible contraindications. Most doctors no longer perform curettage, but use more modern methods.
Is it possible to remove polyps during menstruation?
Surgery for polyps can be carried out both during menstruation and at another period. However, some experts recommend performing the procedure during menstruation. This is due to the fact that removal of a polyp during menstruation reduces the risks of complications arising from trauma to the endometrium of the uterus.
While menstruation is ongoing, it is not recommended to remove polyps
There are natural difficulties that make it difficult to remove a polyp during menstruation - discharge containing endometrial particles and mucus can impair the patency of the hardware tube, the frequency of access to the lesion site and visibility. These disadvantages often lead to the reappearance of growths.
Note! If the polyp is located in the cervix, or the woman has bleeding (during menstruation), then the operation is performed during menstruation.
If the tumors are removed as planned, the procedure is scheduled for 2 or 3 days after the end of menstruation. The endometrial layer, which has not yet grown, allows for good visualization while maintaining free access
When will your period start after surgery?
The menstrual cycle changes after treatment. The reason for this is trauma to the uterine endometrial layer, taking medications and restoring hormonal balance after tumor removal.
Menstruation after removal of a polyp with normal rehabilitation begins on average 40 days later. If after removal of the polyp there are no periods for more than two months, you should consult a gynecologist. Complications may develop, or during the operation, not only the upper layer of the uterus was damaged.
After watching this video, you will learn about the treatment of polyps:
Menstruation after polypectomy is often heavy, but its duration should be limited to 7–10 days. Longer periods may indicate insufficient cleaning of the uterus.
Scanty periods after polyp removal, which come on time and do not cause any pathological symptoms, are the norm. If there has been a significant delay in juice for more than 60 days and there is pain, you should urgently consult your doctor.
Polyps are a dangerous disease, regardless of their location. The growths can migrate, grow and develop into a malignant tumor. You should not try to treat the disease with traditional methods or refuse surgery. Incorrect treatment can have life-threatening consequences.
Source: https://mesyachnie.com/informacija/polip.html